1. Introduction
Breast cancer is the most frequently diagnosed malignant tumor among women across the globe. Patients with breast cancer constitute up to 36% of all oncology patients. In 2022, 2.3 million women were diagnosed with breast cancer, resulting in 670,000 global mortalities (1).
Adjuvant radiotherapy plays a crucial role in the management of breast cancer. Following breast-conserving surgery for infiltrating carcinoma, adjuvant radiotherapy is typically recommended; however, it may be safely omitted in certain patients with low-risk disease based on specific pathological and clinical criteria. This approach significantly reduces the likelihood of local recurrence, highlighting the essential role of adjuvant radiotherapy in effectively controlling regional recurrence, thereby contributing to a decrease in disease-specific mortality (2). Adjuvant radiotherapy is anticipated to result in an absolute increase in 20-year survival rates of approximately 2 - 4%, except for women at particularly low risk for local recurrence (3).
On the other hand, considering the increased survival of patients with breast cancer in recent decades due to screening and effective treatments, we are witnessing long-term complications of treatment (4).
One of the most important long-term side effects of breast radiotherapy is the occurrence of secondary cancers. Patients with breast cancer who have undergone radiotherapy face a slightly elevated but statistically significant risk of developing second cancers (5).
In other words, these secondary cancers are very challenging due to the previous treatment received. Therefore, it is crucial to consider these effects when determining the treatment volume and the type of radiotherapy method.
Dermatofibrosarcoma protuberans (DFSP) is a slow-growing, locally aggressive fibrous tumor that affects subcutaneous tissue. It is often found in the proximal extremities and on the trunk, but its occurrence in the breast is extremely rare (6). Due to the high local recurrence rates, surgical excision with wide margins is recommended. Additionally, the role of adjuvant radiotherapy remains uncertain. Although it is very uncommon, distant metastasis can occur (7).
2. Case Presentation
The patient, a 34-year-old woman with no known family history of cancer, approximately 10 years ago, noticed a mass in the lower inner quadrant of her right breast. Following this finding, she was underwent a biopsy and diagnosed with triple-negative invasive ductal carcinoma, confirmed by immunohistochemistry (IHC). Breast conservative surgery and sentinel lymph node biopsy (SLNB) were performed. One lymph node was detected that was disease-free. The patient’s stage was T2N0M0 according to AJCC -7th (2010) edition. Adjuvant chemotherapy with a regimen of doxorubicin (60 Mg/m2) and cyclophosphamide (600 mg/m2) for four cycles, followed by paclitaxel (80 mg/m2 weekly for 12 weeks) was administered. The patient subsequently underwent adjuvant radiotherapy, receiving a total dose of 50 Gy in 25 fractions. Treatment was delivered using a Varian linear accelerator (Varian Medical Systems, Palo Alto, CA, USA) operating at 6 MV. Radiotherapy included supraclavicular and tangential fields, followed by a 10 Gy boost to the tumor bed. After completing the treatment, the patient was followed up, and her first visit occurred one month later. Aside from mild hyperpigmentation in the radiotherapy field and the surgical scar, there were no notable findings during the examination.
The patient did not visit the oncology clinic for follow-up care for 5 years after completing treatment, until in the 6th year, the patient was referred to this center with complaints of a mass and erythema at the site of the previous mass, which she had been experiencing for about 11 months.
A thorough physical examination revealed a nodule measuring about 2 × 2 cm in the scar site of previous surgery. Mammography and ultrasonography were performed. The ultrasonography examination indicated a 2.5 × 2.5 cm hypoechoic mass with lobulated margins and increased skin thickness without any reported axillary lymphadenopathy.
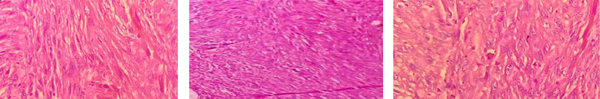
A core needle biopsy was performed, and histopathological examination confirmed the diagnosis of DFSP, characterized by spindle-shaped fibroblasts arranged in a storiform pattern (Figure 1). The IHC staining was positive for CD34 and negative for S-100 and desmin.
The patient underwent wide local excision. Given the patient’s negative imaging studies of the axillary area, no surgical exploration was performed. The final pathology also confirmed the diagnosis of DFSP with a negative 3 cm margin. Considering the negative margin of 3 cm and the history of previous radiotherapy, the patient did not receive any adjuvant therapy.
In this case, the patient was monitored closely post-surgery, with regular follow-ups every three months for the first two years and biannual checks thereafter. Imaging with breast and axillary ultrasonography was performed biannually. No recurrence was noted at the 4-year follow-up.
3. Discussion
Radiation therapy is a well-recognized potential cause of malignant tumors. The diagnostic criteria for post-radiation soft tissue sarcoma generally include: (1) A prior history of radiation exposure; (2) development of a secondary tumor within the previously irradiated area; (3) a minimum latency period of two years between radiation treatment and the onset of the secondary tumor and (4) evidence that the sarcoma is histologically different from the original irradiated tumor. All these criteria were met in the present case, although establishing this diagnosis can be challenging.
The DFSP accounts for less than 0.1% of all skin cancers and 6% of soft tissue sarcomas in the United States (8). In the study conducted by Laskin et al. (9), 53 cases of soft tissue sarcoma were documented after radiation treatment. The most commonly observed type was malignant fibrous histiocytoma (68%), followed by extraskeletal osteosarcoma (13%), fibrosarcoma (11%), malignant schwannoma (4%), extraskeletal chondrosarcoma (2%), and angiosarcoma (2%). Notably, the study did not identify any cases of DFSP, and the latency period for these 53 cases ranged from 2 to 40 years with a mean duration of 10 years. Additionally, Chang et al. (10) reported seven instances of post-radiation sarcoma among 2,868 patients who received cranial irradiation, which included four cases of fibrosarcoma and three cases of malignant fibrous histiocytoma. Only two documented case reports have described DFSP occurring in previously irradiated areas (11). Although DFSP is uncommon, it should be considered in the differential diagnosis of fibrohistiocytic tumors that develop after radiation therapy. To better understand the context of DFSP and soft tissue sarcoma, particularly in field of previous radiation therapy, we have compiled a summary of relevant literature in Table 1.
| Studies | Type of Sarcoma | Location | Radiation Dose | Latency Period | Treatment | Outcome |
|---|---|---|---|---|---|---|
| Laskin et al. (9) | Various (no DFSP) | General | Variable | 2 - 40 years | Surgery ± RT | Variable |
| Chang et al. (10) | Fibrosarcoma, MFH | Cranial | Variable | Not specified | Surgery ± RT | Variable |
| Dai et al. (12) | DFSP (head and Neck) | Head and neck | 60 Gy | Not specified | Surgery + RT | Good local control |
| Wang et al. (13) | DFSP (breast) | Breast | Not specified | Not specified | Surgery ± RT | No recurrence |
Summary of Soft Tissue Sarcomas in Field of Previous Radiotherapy
Considering the likelihood of recurrence and the distinct challenges associated with DFSP in previously irradiated areas, careful monitoring and consideration of adjuvant therapies are essential for effective management. However, due to the rarity of DFSP in radiation field, further studies should be conduct to clarify the mechanism and whether radiation therapy plays a contributory role in its development. Additionally, research should focus on identifying optimal treatment strategies for this rare but significant condition.