1. Background
Pain is an unpleasant sensation typically associated with actual or potential tissue damage (1). Postoperative pain management remains a critical concern, as inadequate pain control can lead to patient anxiety, physiological stress, and prolonged recovery (2-4). Effective pain management is particularly challenging in opioid-dependent patients due to altered pain perception, drug interactions, and tolerance development, which may necessitate higher analgesic doses (5-7). Opioids act as μ-receptor agonists, providing analgesia but also inducing tolerance with chronic use (8, 9). In opioid-dependent individuals, standard opioid regimens may be insufficient, increasing the risk of side effects (10).
Three key considerations in postoperative pain management for opioid-abuser patients include altered pain perception, drug interactions between prescribed opioids and abused substances, and comorbidities associated with long-term opioid use (11, 12). Addiction, particularly to opioids, is a growing global concern, especially in developing countries (13). Iran has one of the highest rates of opioid addiction worldwide (14-16). In the United States, over-the-counter opioid sales have quadrupled over the past 15 years, with one in five chronic nonmalignant pain patients receiving opioid therapy (17). Commonly abused opioids include:
1. Prescription opioids (e.g., oxycodone, hydrocodone, morphine)
2. Illicit opioids (e.g., opium, heroin, methadone, buprenorphine) (18).
Numerous studies on opioid addiction and the various mechanisms underlying their nociceptive effects highlight the critical role of pain management in these patients, particularly during the postoperative period for anesthesiologists. Given the significance of opioids in postoperative analgesia and the heightened tolerance observed in addicted patients, effective pain control becomes even more challenging (19). Opioids play a crucial role in managing both intraoperative and postoperative pain (20). However, due to tolerance development in opioid-dependent individuals, higher doses may be required, potentially leading to an increased risk of adverse effects (8). Consequently, alternative strategies — beyond opioid administration — are essential for optimal pain management in this patient population.
Lidocaine is a widely used medication for postoperative pain management, available in various formulations (21, 22). Intravenous lidocaine exerts analgesic, anti-hyperalgesic, and anti-inflammatory effects (23-26). Its mechanism of action involves sodium channel blockade and modulation of cell membrane permeability (27). However, its use is associated with potential neurological side effects (28-30) and cardiac arrhythmias in high-risk patients (31). The maximum recommended dose for its analgesic effect is 1.5 mg/kg/hr, administered for no longer than 24 hours (31).
Magnesium (Mg), the fourth most abundant cation in the body, plays a critical role in physiological homeostasis (31, 32). It exhibits analgesic properties in both human and animal models (33), primarily mediated by its agonist action on N-methyl-D-aspartate (NMDA) receptors in the central nervous system (CNS) (34-36). Over the past two decades, the use of magnesium for analgesia has gained increasing attention (37-39). While some studies report no significant difference in postoperative pain following preoperative magnesium administration (39), others demonstrate a notable reduction in opioid consumption after intravenous Mg injection (38, 40, 41).
Ketamine, another common analgesic, has long been utilized for acute and postoperative pain management, often in combination with opioids (42). Similar to magnesium, ketamine exerts its analgesic effects through NMDA receptor modulation (43). Studies indicate its particular efficacy in pain management for opioid-abuser patients (44, 45). However, its use may be associated with side effects such as agitation, headache, memory disturbances, tachycardia, and hypertension (46).
Distal radius fractures are the most common upper limb fractures and among the most frequent orthopedic injuries in Western countries (47). They predominantly affect individuals aged 18 - 34, with higher prevalence among young males and postmenopausal women (48-51). Postoperatively, patients often experience significant pain during both active and passive movements, underscoring the importance of effective pain management in enhancing rehabilitation, patient compliance, and minimizing psychological distress (52).
2. Objectives
Given the critical role of postoperative pain control in distal radius fracture surgery and the lack of studies evaluating combination therapy with ketamine, lidocaine, and magnesium (KLM) cocktail, this study aims to investigate the efficacy of the KLM cocktail in managing postoperative pain following distal radius fracture surgery.
3. Methods
This double-blind, randomized clinical trial was approved by the Research Ethics Committees of the School of Medicine of Shahid Beheshti University of Medical Sciences (IR.SBMU.MSP.REC.1402.283) and registered with the Iranian Registry of Clinical Trials (IRCT20240803062628N1). Permission was obtained to access patient medical records. Prior to enrollment, all participants provided written informed consent. Eligible patients were those scheduled for distal radius fracture surgery (confirmed radiologically) at Shohada Tajrish Hospital, Tehran, between 2023 and 2024, with a documented history of opium use (1 – 5 g/day).
Exclusion criteria comprised: (1) Surgical duration exceeding 2 hours; (2) intraoperative bleeding necessitating packed cell transfusion; (3) hemodynamic instability requiring pharmacologic intervention; (4) cardiovascular disease; (5) known hypersensitivity to the study medications; (6) arrhythmia, seizure disorders, or psychiatric conditions.
The sample size was determined using Cochran’s formula, with PASS 2022 software for validation. Based on a significance level (α) of 0.05, power (1–β) of 0.8, and standard deviations of 18.52 (KLM group) and 17.37 (morphine group) for Visual Analogue Scale (VAS) pain scores, the minimum required sample size was 20 per group. To enhance statistical reliability, 30 participants were allocated to each group. The calculation followed:
n1 = n2
μ1μ1 = Mean VAS reduction in the KLM group,
μ2μ2 = Mean VAS reduction in the morphine group.
Participants were randomly assigned via a computer-generated number table to one of two groups:
(1) The KLM group: Received 1.5 mg/kg IV lidocaine, 30 mg/kg IV magnesium, and 0.3 mg/kg IV ketamine diluted in 50 mL 0.9% normal saline, infused over 15 minutes preoperatively.
(2) Morphine (M) group: Received 0.1 mg/kg IV morphine in 50 mL 0.9% normal saline, administered similarly.
Study medications were prepared in identical, unlabeled syringes to ensure blinding of both anesthesia providers and patients. General anesthesia was induced with 0.02 mg/kg midazolam, 3 μg/kg fentanyl, 1 – 1.5 mg/kg propofol, and 0.15 mg/kg cisatracurium, and maintained with sevoflurane (2 – 3% MAC). Neuromuscular blockade was reversed using 0.06 mg/kg neostigmine and 0.02 mg/kg atropine. Intraoperative monitoring included train-of-four (TOF), Bispectral Index (BIS), electrocardiography (ECG), pulse oximetry (SpO2), and non-invasive blood pressure (NIBP). Postoperative pain was evaluated using the VAS (0 - 10) at PACU admission and at 3, 6, and 12 hours postoperatively. Data were analyzed using SPSS v26.0. Normality was assessed via the Shapiro-Wilk test. Normally distributed quantitative data were reported as mean ± SD and compared using independent t-tests or ANOVA (for multiple groups). Non-normal data were expressed as median (IQR) and analyzed using the Mann-Whitney U or Kruskal-Wallis tests. Categorical variables were summarized as frequencies (%) and compared using the chi-square or Fisher’s exact test, as appropriate. A P-value < 0.05 was considered statistically significant.
The primary outcome was postoperative pain scores at 24 hours. Secondary outcomes included analgesic consumption, length of hospital stay, and complication rates. For moderate to severe pain, patients received intravenous morphine (0.05 mg/kg every 4 hours as needed) or oral acetaminophen (500 mg every 6 hours) combined with ibuprofen (400 mg every 8 hours). Rescue analgesia (e.g., tramadol 50 mg IV) was administered if pain scores exceeded 4 on the VAS.
4. Results
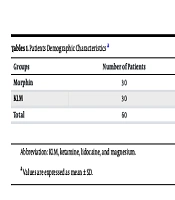
After applying the inclusion and exclusion criteria, 60 patients were enrolled in the study and randomly allocated into two groups (30 patients per group). The mean age of participants was 38.78 years, with the morphine group averaging 38.4 ± 9.601 years and the KLM group averaging 39.17 ± 11.579 years (Table 1). No statistically significant difference was observed in age between the two groups (P = 0.241). Of the total participants, 12 (20%) were female (7 in the morphine group and 5 in the KLM group), and 48 were male (23 in the morphine group and 25 in the KLM group). The difference in gender distribution was not statistically significant (P = 0.137).
| Groups | Number of Patients | Men Age | Women Age | Total Age |
|---|---|---|---|---|
| Morphin | 30 | 38.2 ± 5.1 | 38.6 ± 4.8 | 38.40 ± 4.9 |
| KLM | 30 | 39.0 ± 4.7 | 39.3 ± 5.2 | 39.17 ± 4.9 |
| Total | 60 | 38.6 ± 4.9 | 38.9 ± 5.0 | 38.78 ± 4.9 |
Abbreviation: KLM, ketamine, lidocaine, and magnesium.
a Values are expressed as mean ± SD.
Following administration of the analgesic cocktail, all patients were induced under the same general anesthesia regimen. Postoperative pain was assessed using the VAS, 0 – 10) at the recovery unit by an anesthesia nurse and subsequently at the 3rd, 6th, and 12th postoperative hours by ward nurses (Table 2).
| Groups | VAS in Recovery | VAS 3 (h) Later | VAS 6 (h) Later | VAS 12 (h) Later |
|---|---|---|---|---|
| Morphine | 4.13 ± 0.92 | 3.80 ± 1.05 | 3.07 ± 0.88 | 2.57 ± 0.75 |
| KLM | 3.27 ± 0.85 | 3.47 ± 0.91 | 2.50 ± 0.72 | 1.63 ± 0.68 |
| P-value | 0.038 | 0.246 | 0.008 | 0.000 |
Abbreviations: VAS, Visual Analog Scale; KLM, ketamine, lidocaine, and magnesium.
a Values are expressed as mean ± SD.
4.1. Pain Assessment (Visual Analog Scale Scores)
- Recovery unit: The mean VAS score was 4.2 ± 1.3 in the morphine group and 3.5 ± 1.1 in the KLM group (P = 0.038).
- 3-hour postoperative: The mean VAS score was 3.8 ± 1.2 in the morphine group versus 3.5 ± 1.0 in the KLM group (P = 0.246).
- 6-hour postoperative: The mean VAS score was 3.5 ± 1.0 in the morphine group versus 2.8 ± 0.9 in the KLM group (P = 0.008).
- 12-hour postoperative: The mean VAS score was 3.2 ± 0.8 in the morphine group versus 2.1 ± 0.7 in the KLM group (P < 0.001).
4.2. Adverse Effects
Among the 60 participants, 16 experienced drug-related side effects, with 10 in the morphine group and 6 in the KLM group. The most common adverse effects were:
- Nausea: Eight cases (6 in the morphine group, 2 in the KLM group)
- Vomiting: Five cases (3 in the morphine group, 2 in the KLM group)
- Shivering: Three cases (1 in the morphine group, 2 in the KLM group)
These side effects were managed with antiemetics (ondansetron 4 mg IV for nausea and vomiting) and warming blankets for shivering. The difference in side effect incidence between the groups was not statistically significant (P = 0.243).
4.3. Opioid Consumption (Secondary Outcome)
Total postoperative morphine consumption was significantly higher in the morphine group (12.5 ± 3.2 mg) compared to the KLM group (8.4 ± 2.7 mg) (P = 0.015).
5. Discussion
Postoperative pain management remains a critical challenge for anesthesiologists. Variability in management approaches, patient factors, and procedural differences complicate effective pain control. This issue is particularly pronounced in opioid-dependent patients, who are at heightened risk of receiving suboptimal analgesic dosing and experiencing adverse effects (53). Opioid tolerance, a key consideration in pain management, significantly influences analgesia strategies in this population (54, 55).
Over the years, several pharmacological agents have demonstrated analgesic efficacy. Lidocaine, magnesium, and ketamine each exhibit distinct analgesic mechanisms, yet comprehensive studies on their combined use remain scarce. The present study evaluated a preoperative KLM cocktail alongside morphine for postoperative pain management in opioid-dependent patients undergoing distal radius fracture surgery. Pain intensity was assessed using the VAS, and drug-related side effects in the recovery unit were recorded by blinded nursing staff.
A 2021 retrospective study by Zanza et al. examined the efficacy of a magnesium-lidocaine-ketorolac combination in opioid-abuser patients, reporting reduced morphine consumption and improved VAS scores compared to morphine alone (56). These findings align with our study, reinforcing the potential benefits of multimodal analgesia in postoperative pain management. In a 2018 systematic review, Peng et al. investigated intravenous magnesium’s role in pain control following orthopedic surgeries. While no significant difference in postoperative pain was observed compared to opioids, magnesium-treated patients experienced fewer adverse effects — a result consistent with our findings (57).
Barreveld et al. assessed ketamine’s efficacy in opioid-dependent patients, noting a statistically significant reduction in moderate pain but no marked difference in severe or mild pain management or opioid consumption (58). Similarly, Etezadi et al. evaluated intravenous ketamine and magnesium in spine surgeries, demonstrating significant improvements in postoperative pain and opioid reduction, mirroring our results (59).
Our study revealed a significant reduction in postoperative pain among patients receiving the KLM cocktail compared to morphine, except at the 3-hour postoperative mark. These findings underscore the cocktail’s efficacy in pain management, particularly in the later postoperative phases. Given the unique cultural and physiological considerations of opioid-dependent patients, tailored analgesic evaluation is essential.
Regarding adverse effects, no significant differences were observed in the recovery unit. However, further research is warranted to explore potential side effects associated with combination therapy. Finally, we recommend additional studies comparing various postoperative pain management modalities, including regional techniques. Evaluating surgery-specific variables may further minimize bias and enhance hospitalization outcomes for opioid-dependent patients.
This study has some limitations, including a relatively small sample size and short follow-up period. Additionally, the blinding method could be further improved, as the nature of the interventions (morphine vs. KLM) may have influenced patient or assessor perceptions. Future studies with larger cohorts and longer follow-ups are recommended.
5.1. Conclusions
Preoperative intravenous administration of a combined regimen of KLM improves postoperative pain scores in opium-addicted patients. However, this approach demonstrates no significant difference in recovery unit drug-related side effects compared to morphine.