1. Background
Locoregional anesthetic methods used perioperatively in hip fracture surgery focus on optimizing pain management while minimizing opioid usage and postoperative complications. Recently, a novel locoregional approach for hip fracture pain relief has been introduced: The pericapsular nerve group (PENG) block (1). This interfascial plane block targets the articular branches of the femoral, obturator, and accessory obturator nerves that innervate the hip joint. To achieve comprehensive analgesia or anesthesia of the subcutaneous tissues and skin, this technique may be paired with a block targeting the lateral femoral cutaneous nerve (LFCN) (2).
In 2016, the erector spinae plane block (ESPB) gained widespread application at the thoracic level, utilizing ultrasound guidance to administer local anesthetic between the thoracic vertebrae's transverse process and the erector spinae muscle. A 2018 case study documented the use of lumbar ESPB in managing pain following total hip arthroplasty (THA). The local anesthetic was administered at the fourth lumbar vertebra (L4), spreading both upward (cephalad) and downward (caudad) within the paravertebral region, resulting in effective pain relief for the hip area (3).
2. Objectives
The objective of this study was to investigate whether combined PENG and LFCN blocks are as effective in providing analgesia for hip arthroplasty as an ESP block, while minimizing the occurrence of quadriceps muscle weakness.
3. Methods
3.1. Study Design, Setting, and Location
This randomized, double-blind, parallel-group clinical trial was conducted over six months in the combined assembly operating theatres at Ain Shams University Hospitals, Cairo, Egypt, between 15 May 2024 and 30 November 2024.
3.2. Eligibility Criteria
The study enrolled participants aged 18 to 65 years, classified as American Society of Anesthesiologists (ASA) physical status I to III, of both sexes, and scheduled for unilateral THA due to osteoarthritis.
Exclusion criteria included spinal malformations, post-traumatic femoral neck fractures, liver or kidney dysfunction, hypersensitivity to the drugs used in the study, neuromuscular or coagulopathy disorders, infection at the injection site, psychiatric disorders, long-term use of opioids, use of gabapentin or pregabalin, and a body mass index exceeding 35 kg/m2. Fifty participants were enrolled and randomized into two groups, 25 in each group.
3.3. Ethical Considerations
Ethical approval was obtained (approval number: FAMSU R79/2024), and each participant signed a written consent form after receiving detailed explanations about the study's objectives, associated risks, and benefits. Personal information was kept confidential, and participation was entirely voluntary, with individuals free to withdraw at any time. The trial was registered on ClinicalTrials.gov (trial ID: NCT06402006). Confidentiality of all participant information was assured.
3.4. Randomization, Allocation Concealment, and Blinding
A computer-generated table was used to randomize 50 adult patients into two groups (25 patients each). The randomization sequence was concealed using sealed, opaque envelopes. The patients and data collectors were blinded to the intervention groups. Surgeons were not present during block administration, and anesthesiologists who prepared and performed the block did not participate in postoperative care.
Group A underwent PENG and LFCN blocks, while group B (control) received the ESP block.
3.5. Preoperative Preparation
Before surgery, all participants underwent a detailed medical history and clinical evaluation, accompanied by routine laboratory investigations. They were instructed to fast from solid food for 8 hours and from clear liquids for 2 hours prior to the procedure. Upon arrival in the operating room, an intravenous line was established, and Ringer’s acetate was administered at 10 mL/kg. Baseline monitoring included non-invasive blood pressure (NIBP), electrocardiography (ECG), and arterial oxygen saturation (SpO2). Pain intensity was assessed using the Visual Analogue Scale (VAS), and all participants received preoperative training. For patients experiencing discomfort or unable to tolerate the procedure, sedation was administered, consisting of midazolam at a dose of 0.02 mg/kg, with or without fentanyl at 0.5 - 1 mcg/kg (4).
3.6. Interventions
In group A, an ultrasound-guided PENG block was conducted prior to spinal anesthesia induction using a 2 - 5 MHz curvilinear array transducer on the SonoSite M-Turbo ultrasound device. With the patient lying supine, the probe was aligned parallel to the inguinal crease and rotated clockwise until the iliopsoas muscle tendon, ilio-pubic eminence, anterior inferior iliac spine (AIIS), and femoral artery were visualized. A 22G, 80 mm needle was directed in-plane from the lateral side of the probe until its tip touched the ilio-pubic eminence. After confirming negative aspiration, 20 mL of 0.5% bupivacaine was administered. Proper injection was confirmed by observing fluid spread between the iliopsoas tendon and the periosteum of the ilio-pubic eminence (5).
In the PENG block, the objective was to deposit local anesthetic into the fascial plane between the iliopsoas tendon and the superior pubic ramus to bathe the articular branches of the femoral nerve, accessory obturator nerve, and obturator nerve, ensuring reliable spread to all targets and consistent analgesia of the anterior hip capsule. Clinical studies have converged on a volume of 20 mL, as smaller volumes (e.g., 10 - 15 mL) risk incomplete coverage, while larger volumes offer no additional benefit and increase systemic absorption risk. Using a 0.5% concentration of bupivacaine (i.e., 5 mg/mL) provides a total dose of 100 mg in 20 mL. This concentration-volume combination is justified as 0.5% bupivacaine provides a dense sensory (and some motor) block with an onset of 5 - 10 minutes and a duration of 6 - 8 hours — ideal for perioperative and early postoperative analgesia. It offers an opioid-sparing effect, a wide safety margin, and optimized spread without undue risk. Ultrasound guidance further minimizes the risk of intravascular injection and ensures precise deposition of the full 20 mL in the intended location (6).
The LFCN block was performed using a linear ultrasound probe (10 - 15 MHz). With the patient lying supine, the probe was angled downward toward the AIIS until the LFCN was visualized between the tensor fasciae latae and sartorius muscles. After confirming negative aspiration, 5 mL of bupivacaine was injected (5).
In group B, the ESP block was performed prior to spinal anesthesia with the patient in the lateral decubitus position. A curvilinear probe (2 - 5 MHz) was placed on the third lumbar vertebra in the parasagittal plane to identify the transverse process of L3. The needle was directed in-plane, caudo-cephalically, to the lateral edge of the L3 transverse process. Twenty milliliters of 0.5% bupivacaine were injected under direct visualization along the ESP. Accurate placement was confirmed by the local anesthetic spreading both cephalad and caudad from the injection site, creating separation within the plane between the erector spinae muscles and the transverse processes (7).
Rescue medication consisted of pethidine at 0.5 mg/kg per dose, repeated as needed (when the VAS score reached 4 or higher), ensuring that the total daily dose did not exceed 1 mg/kg every 8 hours. Additionally, all patients received a standardized multimodal analgesic regimen during recovery, consisting of 1000 mg of paracetamol every 8 hours and 30 mg of ketorolac every 12 hours (8). Ketorolac was avoided in patients with allergies or gastritis; paracetamol was omitted if the patient was allergic. Tramal 50 mg IV infusion was used as rescue medication if pethidine failed to control pain.
The primary anesthetic technique was spinal anesthesia, which involved administering 3 - 3.5 mL of 0.5% hyperbaric bupivacaine into the L2 - L3 or L3 - L4 space using a 25G pencil-point needle. This was supplemented with 20 µg of fentanyl as an adjuvant while the patient was in the sitting position. Hypotension, defined as a ≥ 20% reduction from baseline blood pressure, was managed with intravenous ephedrine (6 mg boluses) (8). In the event of spinal anesthesia failure or prolonged surgeries, general anesthesia would have been initiated, but no conversions to general anesthesia occurred during the study.
The study endpoint included evaluation of outcomes up to 48 hours postoperatively.
3.7. Measurement Tools
Pain intensity was assessed postoperatively using the VAS at 0, 6, 12, 24, and 48 hours (where 0 indicates no pain and 10 represents the worst imaginable pain). Moderate-to-severe pain, defined as a VAS score of 4 or higher within the initial 48 hours post-surgery, was also recorded (9). Hip joint motor recovery was evaluated after the resolution of spinal anesthesia using active hip flexion, quantified with a protractor (from 0º to 90º) (8).
3.8. Study Outcomes
Primary outcomes included the evaluation of pain using the VAS at 0, 6, 12, 24, and 48 hours postoperatively (0 indicating no pain, 10 indicating the worst imaginable pain), recording instances of moderate-to-severe pain (VAS ≥ 4) within the first 48 hours, the duration until the first experience of pain and request for analgesia, analgesic consumption during post-anesthesia care unit (PACU) stay (in minutes), and analgesic use within the first 48 hours (converted to IV pethidine equivalents). Secondary outcomes included motor recovery of the hip joint, time to first ambulation, and length of hospital stay.
3.9. Sample Size
With power set at 0.80 and α = 0.05, and using PASS 11th release (Hintze, 2011) (10), the minimum required sample size was 11 patients per group to detect a statistically significant difference between the assumed times to first rescue analgesia: 13.3 ± 3.5 hours in the PENG group and 9.5 ± 2.3 hours in the ESP group (11). A total of 25 participants were included in each group to account for a potential 10.0% attrition rate and to support analysis of additional outcomes.
3.10. Statistical Analysis
The collected data were coded, organized into tables, and statistically analyzed using IBM SPSS Statistics software version 28.0 (IBM Corp., Chicago, USA, 2021). The Shapiro-Wilk test assessed the normality of quantitative data, which were expressed as mean ± standard deviation (SD). Independent t-tests and one-sample t-tests were applied for comparisons. Qualitative data were presented as frequencies and proportions, with comparisons analyzed using the chi-square test. The log-rank test was used to compare time-to-event variables such as time to the first dose of pethidine and time to first ambulation. A P-value < 0.050 was considered statistically significant. Relative effect was calculated for the PENG block group compared to the ESP block group.
4. Results
4.1. Attrition and Baseline Comparisons
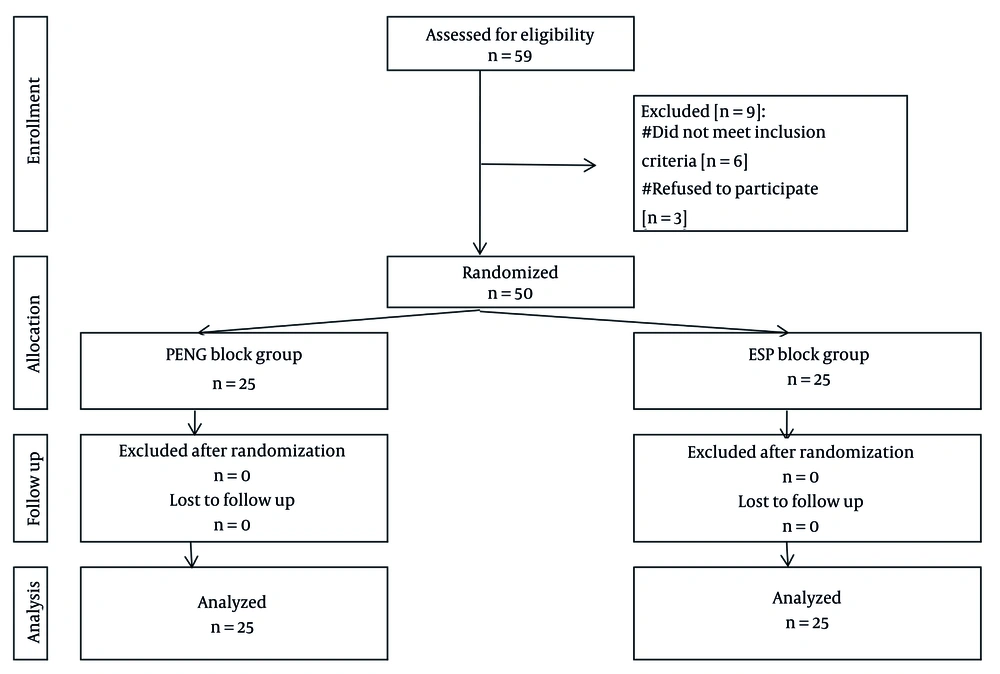
Attrition refers to the loss of participants after randomization. As illustrated in the CONSORT flowchart (Figure 1), 59 patients were assessed for eligibility. Nine were excluded for not meeting the inclusion criteria, and 3 patients declined to participate, leaving 50 participants who were randomized into two groups of 25 each. All 50 participants completed the study, with no post-randomization attrition.
4.2. Baseline Characteristics
Table 1 compares the baseline characteristics of groups A and B, showing no significant differences in age, Body Mass Index (BMI), sex distribution, ASA physical status, or duration of surgery (all P > 0.05). This indicates that both groups were comparable at baseline.
| Variables | PENG Block Group (Total = 25) | ESP Block Group (Total = 25) | P-Value |
|---|---|---|---|
| Age (y) | 49.9 ± 7.3 | 50.2 ± 6.9 | 0.890 |
| Sex | 0.774 | ||
| Male | 14 (56.0) | 15 (60.0) | |
| Female | 11 (44.0) | 10 (40.0) | |
| BMI (kg/m2) | 29.5 ± 2.7 | 30.2 ± 2.8 | 0.344 |
| ASA | 0.920 | ||
| I | 7 (28.0) | 6 (24.0) | |
| II | 13 (52.0) | 13 (52.0) | |
| III | 5 (20.0) | 6 (24.0) | |
| Operation duration (min) | 2.3 ± 0.7 | 2.1 ± 0.6 | 0.178 |
Abbreviations: BMI, Body Mass Index; ASA, American Association of Anesthesia; PENG, pericapsular nerve group; ESP, erector spinae plane.
a Values are expressed as No. (%) or mean ± SD.
4.3. Pain Outcomes
Table 2 compares postoperative pain scores, the total 48-hour area under the curve (AUC), and the number of moderate-to-severe pain episodes within 48 hours between the study groups. Group A demonstrated significantly lower postoperative pain scores at 6, 12, and 24 hours compared to group B (P < 0.05), with mean differences of -0.4 ± 0.2, -0.7 ± 0.3, and -0.8 ± 0.2, respectively. However, no significant differences were observed at 0 and 48 hours (P > 0.05). Regarding the total 48-hour AUC and the number of moderate-to-severe pain episodes within 48 hours, group A showed significantly lower values (P < 0.001), with mean differences of -0.5 ± 0.1 and -1.7 ± 0.2, respectively. These findings suggest that group A experienced superior pain control compared to group B.
| Postoperative Time | PENG Block Group (Total = 25) | ESP Block Group (Total = 25) | P-Value | Relative Effect | |
|---|---|---|---|---|---|
| Mean ± SE | 95% CI | ||||
| Hour-0 | 0.8 ± 0.9 | 1.0 ± 0.5 | 0.263 | -0.2 ± 0.2 | -0.7 to 0.2 |
| Hour-6 | 2.3 ± 0.6 | 2.8 ± 0.7 | 0.026 | -0.4 ± 0.2 | -0.8 to -0.1 |
| Hour-12 | 2.9 ± 1.3 | 3.6 ± 1.0 | 0.039 | -0.7 ± 0.3 | -1.3 to 0.0 |
| Hour-24 | 3.0 ± 0.8 | 3.8 ± 0.7 | 0.001 | -0.8 ± 0.2 | -1.2 to -0.3 |
| Hour-48 | 2.5 ± 0.6 | 2.7 ± 0.6 | 0.164 | -0.2 ± 0.2 | -0.6 to 0.1 |
| Total 48-hour AUC | 2.6 ± 0.4 | 3.2 ± 0.4 | < 0.001 | -0.5 ± 0.1 | -0.8 to -0.3 |
| 48-hour times of moderate/severe pain | 1.2 ± 0.4 | 3.0 ± 0.8 | < 0.001 | -1.7 ± 0.2 | -2.1 to -1.3 |
Abbreviations: AUC, area under curve; SE, standard error; CI, confidence interval; PENG, pericapsular nerve group; ESP, erector spinae plane.
a Values are expressed as mean ± SD.
4.4. Analgesic Requirements
Table 3 compares analgesic requirements and doses between groups A and B. Group A had a significantly shorter time to the initial pethidine dose, and lower total 48-hour doses of pethidine and paracetamol compared to group B (P < 0.001), with mean differences of 5.0 ± 0.7, -79.0 ± 7.5, and -1240.0 ± 197.3, respectively. These findings indicate that group A required less analgesic medication and had better pain control.
| Time | PENG Block Group (Total = 25) | ESP Block Group (Total = 25) | P-Value | Relative Effect | |
|---|---|---|---|---|---|
| Mean ± SE | 95% CI | ||||
| Pethidine | |||||
| Time to first dose (hour) | 13.4 ± 3.1 | 8.4 ± 1.7 | < 0.001 | 5.0 ± 0.7 | 3.6 to 6.4 |
| Total 48-hour dose (mg) | 49.0 ± 21.0 | 128.0 ± 30.9 | < 0.001 | -79.0 ± 7.5 | -94.0 to -64.0 |
| Paracetamol | |||||
| Total 48-hour dose (mg) | 600.0 ± 204.1 | 1840.0 ± 965.2 | < 0.001 | -1240.0 ± 197.3 | -1636.7 to -843.3 |
Abbreviations: SE, standard error; CI, confidence interval; PENG, pericapsular nerve group; ESP, erector spinae plane.
a Values are expressed as mean ± SD.
4.5. Functional Recovery and Hospital Stay
Table 4 shows no significant differences between groups A and B in terms of range of motion and active hip flexion. Similarly, no significant difference was found in hospital stay duration (P = 0.113). However, group A demonstrated a significantly shorter time to first ambulation, with a mean difference of -9.4 ± 1.0 (P < 0.001). Overall, while range of motion and hospital stay were comparable, group A achieved earlier mobilization.
| Variables | PENG Block Group (Total = 25) | ESP Block Group (Total = 25) | P-Value | Relative Effect | |
|---|---|---|---|---|---|
| Mean ± SE | 95% CI | ||||
| Range of hip flexion (degree) | 71.8 ± 7.6 | 66.0 ± 13.5 | 0.065 | 5.8 ± 3.1 | -0.4 to 12.1 |
| Time to first walk (h) | 21.2 ± 3.2 | 30.6 ± 3.5 | < 0.001 | -9.4 ± 1.0 | -11.3 to -7.5 |
| Length of stay (h) | 73.4 ± 9.1 | 77.7 ± 10.0 | 0.113 | -4.4 ± 2.7 | -9.8 to 1.1 |
Abbreviations: SE, standard error; CI, confidence interval; PENG, pericapsular nerve group; ESP, erector spinae plane.
a Values are expressed as mean ± SD.
4.6. Side Effects
Table 5 indicates no significant differences in side effects between groups A and B. Both groups had similar rates of hypotension, with no reported cases of bradycardia or anaphylaxis. Overall, side effect profiles were comparable between the groups.
Abbreviations: SE, standard error; CI, confidence interval; NA, not applicable.
a Values are expressed as No. (%).
b Relative effect: Effect in group A relative to that in group B.
c Fisher’s Exact test.
5. Discussion
Total hip arthroplasty serves as an economically viable solution for managing osteoarthritis, effectively alleviating pain and enhancing overall well-being (12). However, THA is associated with considerable postoperative discomfort, often resulting in extensive reliance on analgesics (13). The prevalence of opioid prescriptions following THA can reach up to 89.7% (14, 15).
This study aimed to compare the efficacy of two nerve block techniques in managing postoperative pain, analgesic requirements, range of motion, active hip flexion, time to ambulation, and hospital stay duration after THA. Our findings demonstrated that group A (PENG and LFCN blocks) experienced significantly lower pain scores than group B (ESP block) at 6, 12, and 24 hours postoperatively. Furthermore, group A had a longer duration before the first pethidine dose and required significantly lower total 48-hour doses of both pethidine and paracetamol.
Although multiple primary outcomes were evaluated, the sample size was calculated based on time to first analgesic request, deemed the most clinically relevant and sensitive indicator of nerve block effectiveness.
Group A also showed significantly earlier ambulation compared to group B. However, there were no statistically significant differences between the groups in terms of range of motion, active hip flexion, or hospital stay duration.
The PENG block, a relatively new regional analgesia technique for managing hip pain, was first introduced by Girón-Arango et al. (1). This technique involves ultrasound-guided anesthetic injection near the anterior inferior iliac spine, targeting the articular branches of the obturator, accessory obturator, and femoral nerves (16). Evidence from randomized controlled trials suggests that the PENG block improves pain relief while preserving motor function and quadriceps strength, thereby promoting early postoperative mobility and enhancing recovery quality (8, 17).
Early postoperative ambulation is a cornerstone of enhanced recovery after surgery (ERAS) protocols. Mobilizing patients within the first 24 hours postoperatively mitigates complications related to immobility, such as muscle deconditioning, insulin resistance, and pulmonary stasis (18). From a healthcare efficiency standpoint, ERAS implementation translates into substantial cost savings and improved throughput. For example, an enhanced short-stay ERAS model for hip and knee arthroplasty has been shown to reduce acute ward stays by an average of two days compared to standard care (19).
Consistent with our findings, Pascarella et al. (8) reported that patients receiving a PENG block delayed their first opioid dose to an average of 12 hours postoperatively, whereas those in the control group required opioids within six hours after THA. Ince and Kilicaslan (20) also demonstrated the efficacy of the PENG block in managing postoperative pain in elderly patients undergoing hip arthroplasty. They further noted that combining the PENG block with ESPB prolonged the analgesic effect.
In agreement with our results, Luftig et al. (21) emphasized the effectiveness of the PENG block in alleviating pain in trauma patients with acute pelvic fractures in emergency settings, attributing its utility to its rapid onset, potent analgesic effect, and ability to preserve motor function.
Short et al. (22) established that the sensory innervation of the anterior hip capsule is primarily derived from the superior branches of the femoral and obturator nerves. Their findings indicated that, unlike the posterior and inferior regions, the anterior capsule receives the majority of sensory input (23). Additionally, histological studies have shown that the anterior capsule contains a dense population of nociceptive fibers, whereas the posterior capsule contains more mechanoreceptors (24). These findings support the efficacy of the PENG block, which provides comprehensive sensory nerve coverage without affecting motor function, thus facilitating early mobilization and rehabilitation compared to the ESP block.
Conversely, in a multicenter randomized trial, Lin et al. (25) compared the PENG block combined with local infiltration analgesia (LIA) to a placebo with LIA. They found comparable opioid usage between the groups, despite differences in pain scores. These discrepancies may be attributed to the older age of participants and lower baseline opioid consumption in their study population.
5.1. Conclusions
In THA, the combination of PENG and LFCN blocks provides superior postoperative analgesia, reduces opioid consumption, and shortens the time to ambulation compared to the ESP block.
5.2. Limitations
This study had several limitations, including a relatively small sample size and reliance on ultrasound-guided techniques, which require experienced operators. Additionally, the absence of a control group with no intervention limited the ability to establish a baseline for comparison. The sample size was also powered only for one primary outcome, so interpretations of secondary outcomes should be considered exploratory.