Abstract
Keywords
1. Introduction
The novel coronavirus can cause acute respiratory disease that was first identified in December 2019 in Wuhan. It has affected more than five million people worldwide (1, 2). Some COVID-19 patients have psychological diseases that require medical treatment or electroconvulsive therapy under general anesthesia. Electroconvulsive therapy (ECT) can be life-saving in patients with suicide history or catatonic schizophrenia.
Health workers are at the front line of the COVID-19 outbreak control and must follow health instructions. Aerosol-producing procedures such as suction in anesthesia for ECT may facilitate the transmission of infectious diseases such as COVID-19. Due to the high risk of these procedures, in terms of virus infection, the procedures should be performed with complete protective equipment.
2. Case Presentation
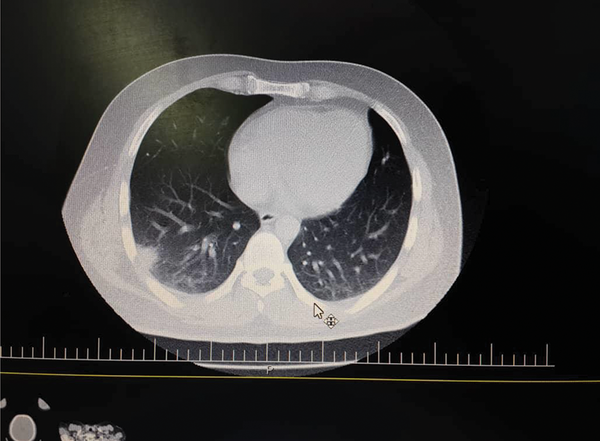
On March 30, a 25-year-old male patient, weighing 85 kg, without any past medical history, was admitted to the hospital with fever, cough, headache, and muscle pain symptoms. Chest CT scan revealing of pulmonary involvement led to a COVID-19 diagnosis, as shown in Figure 1. Thus, the patient was prescribed acetaminophen naproxen and hydroxychloroquine. The patient had the experience of irritable mood, increased self-esteem, reduced need for sleep, talkativeness, agitation, and psychotic symptoms like grandiosity delusion, auditory, and visual hallucination. Finally, he drank a small amount of bleach solution to disinfect his body. Then, he was transferred to the hospital by the emergency medical service. According to an interview with the patient and his family, the patient was diagnosed with bipolar I disorder and manic episodes with psychotic symptoms.
The patient had BP 100/60 mmHg, PR125, and SPO2 86% at the time of hospitalization. He had no fever but complained of mild coughs and dyspnea. He was prescribed coltra, azithromycin, and sodium valproate. During the hospitalization, to control the aggressive behaviors of the patient, 20 mg of haloperidol (IM), 10 mg of biperiden (IM), and 100 mg of chlorpromazine (IM) were administered daily. The patient was hospitalized for one week in the emergency department and then at the general ward. He was visited by an emergency medical service and ENT specialist, and the required radiographies were taken, which showed no damage to the airway due to the bleach. Due to the little volume of the fluid and normal results of CT scan and endoscopy, no treating action for the digestive system was conducted. Because of the poor patient's response to treatment, ECT was conducted in six steps on 4th, 8th, 10th, 12th, 14th, and 16th April.
Lung CT scan of the patient
Based on the procedure, ECT should be conducted in the Department of Psychiatry of a hospital; however, regarding the likelihood of the transmission of COVID-19 to other ECT patients, the therapy was conducted in a section devoted to patients with acute respiratory syndrome using proper personal protective equipment (PPE). Full PPE was provided for all medical personnel, including gloves, aprons, long-sleeved gowns, N95 masks, eye goggles, face visors, and shoe covers. For anesthesia, a circulation system with a manual ventilator was used. The patient was fully monitored while using a peripheral venous catheter. The patient received 20 mg succinylcholine chloride and 200 mg sodium thiopental. After the induction of anesthesia, a dental guard was inserted to protect the teeth, and then, electroshocks of 35, 50, 65, 80, and 100 volts were induced, in sequence, in the six steps. The ECT resulted in generalized seizures for 25 to 35 seconds. During the anesthesia and recovery, the patient received 500 cc of normal saline infusion serum. Masking, manual ventilation, and suction were all carried out under an appropriate plastic cover to avoid the spreading of the novel coronavirus. Relaxants and anesthetics were such dosed to minimize the requirement for manual ventilation. After 30 minutes of recovery at the end of each ECT step, the patient was transferred to the ward. After the simultaneous completion of COVID-19 treatment and improving the mood and psychotic symptoms, the patient was discharged from the hospital with good general conditions. The treatment was followed by oral haloperidol, oral sodium valproate, and oral bipyridine.
3. Discussion
Electroconvulsive therapy (ECT) was first experienced in 1938 and had been conducting without anesthesia for 30 years (3). The most common indication for ECT is mood disorder (major depressive disorder and bipolar I disorder). It should be considered for use in patients who do not tolerate medications, have severe or psychotic symptoms, are acutely suicidal or homicidal, or have marked symptoms of agitation or stupor (4). Electroconvulsive therapy is usually conducted three times per week and can be continued for two to four weeks. Patients usually show signs of improvement after receiving ECT three to five times (5). Using ECT with scalp electrodes results in a spike-and-wave pattern of the electroencephalogram (EEG) in the patient, which is accompanied by generalized seizure and cardiovascular stimulation, followed by increased cerebral blood flow (CBF) and intracranial pressure (ICP) (6). Hemodynamic responses to ECT can even cause myocardial ischemia (7). The seizures of EEG that last for 25 to 50 seconds can result in the optimal treatment (8). Most of the anesthetics have anti-seizure effects and can reduce the time of seizures based on the dosage. The overuse of anesthetics can weaken the response to ECT by reducing the time of seizure.
Methohexital is considered the gold standard for ECT (9). Other anesthetics used for these patients are sodium thiopental and etomidate. The latter can cause longer seizures in patients with short seizures (10). Thiopental is preferred over propofol for ECT anesthesia induction (11). Not taking a muscle relaxant before ECT may lead to more severe myalgia. Using relaxants is a common practice to reduce myalgia and prevent bone fracture and joint dislocation. To this end, succinylcholine is the most frequently used relaxant (12). Since ECT is conducted three to four times per week and takes a few minutes, tracheal intubation is not a common practice, except for patients in their late pregnancy or on a full stomach (13). Circulation or simple bag-mask is usually used for ventilation. In obese patients with obstructive sleep apnea, an airway can be used.
Most COVID-19 patients exhibit neurological manifestations. In a study, notably, 26 out of 40 patients (65%) hospitalized in the ICU showed agitation, and 69% of relaxant takers showed agitation after medication discontinuation (14). The novel coronavirus can be found in the brain or cerebrospinal fluid of patients. Even though the respiratory system is the most involved part in COVID-19, patients can show some neurological demonstrations such as paresthesia headache, mood disorder, and attention deficit (15). During the COVID-19 pandemic, some of the patients that go to the hospital for other reasons may be infected with the novel coronavirus. Also, some of the COVID-19 patients may require treatment under general anesthesia.
Electroconvulsive therapy can be life-saving in patients with suicide history or catatonic schizophrenia. Thus, ECT cannot always be postponed during the COVID-19 pandemic regarding that it is an elective service. Using proper PPE is mandatory during ECT for susceptible novel coronavirus patients, as the patients can spread the virus after ventilation by masks or manual bags via cough or discharges. Personnel should be equipped with two-layer gloves, long-sleeved gowns, and proper masks, and Ambu bags should be connected to antiviral filters if possible. It is suggested that the patients be effectively preoxygenated to decrease their requirement for ventilation by the manual bag. Also, a disposable bite block should be used. The distance between patients during recovery should be at least six feet. The number of the medical crew should be kept minimum, and, if possible, the procedure should be conducted in a negative pressure room (16, 17).
References
-
1.
Pergolizzi JJ, Magnusson P, LeQuang JA, Breve F, Paladini A, Rekatsina M, et al. The Current Clinically Relevant Findings on COVID-19 Pandemic. Anesth Pain Med. 2020;10(2). e103819. [PubMed ID: 32754437]. [PubMed Central ID: PMC7352949]. https://doi.org/10.5812/aapm.103819.
-
2.
Rahimzadeh P, Amniati S, Farahmandrad R, Faiz SHR, Hedayati Emami S, Habibi A. Clinical characteristics of critically Ill patients infected with COVID-19 in Rasoul Akram Hospital in Iran: A Single center study. Anesth Pain Med. 2020;10(5). e107211. https://doi.org/10.5812/aapm.107211.
-
3.
Khan A, Mirolo MH, Hughes D, Bierut L. Electroconvulsive Therapy. Psychiatr Clin North Am. 1993;16(3):497-513. https://doi.org/10.1016/s0193-953x(18)30162-x.
-
4.
Thompson JW, Weiner RD, Myers CP. Use of ECT in the United States in 1975, 1980, and 1986. Am J Psychiatry. 1994;151(11):1657-61. [PubMed ID: 7943457]. https://doi.org/10.1176/ajp.151.11.1657.
-
5.
Segman RH, Shapira B, Gorfine M, Lerer B. Onset and time course of antidepressant action: psychopharmacological implications of a controlled trial of electroconvulsive therapy. Psychopharmacology (Berl). 1995;119(4):440-8. [PubMed ID: 7480524]. https://doi.org/10.1007/BF02245860.
-
6.
Saito S, Miyoshi S, Yoshikawa D, Shimada H, Morita T, Kitani Y. Regional cerebral oxygen saturation during electroconvulsive therapy: monitoring by near-infrared spectrophotometry. Anesth Analg. 1996;83(4):726-30. [PubMed ID: 8831310]. https://doi.org/10.1097/00000539-199610000-00011.
-
7.
López-Gómez D, Sánchez-Corral MA, Jara F, Esplugas E, Cobo JV. Infarto agudo de miocardio tras terapia electroconvulsiva. Revista Española de Cardiol. 1999;52(7):536-8. https://doi.org/10.1016/s0300-8932(99)74966-3.
-
8.
Sackeim HA, Devanand DP, Prudic J. Stimulus intensity, seizure threshold, and seizure duration: impact on the efficacy and safety of electroconvulsive therapy. Psychiatr Clin North Am. 1991;14(4):803-43. [PubMed ID: 1771150].
-
9.
Avramov MN, Husain MM, White PF. The comparative effects of methohexital, propofol, and etomidate for electroconvulsive therapy. Anesth Analg. 1995;81(3):596-602. [PubMed ID: 7653829]. https://doi.org/10.1097/00000539-199509000-00031.
-
10.
Mokriski BK, Nagle SE, Papuchis GC, Cohen SM, Waxman GJ. Electroconvulsive therapy-induced cardiac arrhythmias during anesthesia with methohexital, thiamylal, or thiopental sodium. J Clin Anesth. 1992;4(3):208-12. [PubMed ID: 1610576]. https://doi.org/10.1016/0952-8180(92)90067-b.
-
11.
Nuzzi M, Delmonte D, Barbini B, Pasin L, Sottocorna O, Casiraghi GM, et al. Thiopental is better than propofol for electroconvulsive therapy. Acta Biomed. 2018;88(4):450-6. [PubMed ID: 29350659]. [PubMed Central ID: PMC6166177]. https://doi.org/10.23750/abm.v88i4.6094.
-
12.
Sarpel Y, Togrul E, Herdem M, Tan I, Baytok G. Central acetabular fracture-dislocation following electroconvulsive therapy: report of two similar cases. J Trauma. 1996;41(2):342-4. [PubMed ID: 8760548]. https://doi.org/10.1097/00005373-199608000-00025.
-
13.
Kadar AG, Ing CH, White PF, Wakefield CA, Kramer BA, Clark K. Anesthesia for electroconvulsive therapy in obese patients. Anesth Analg. 2002;94(2):360-1. table of contents. [PubMed ID: 11812699]. https://doi.org/10.1097/00000539-200202000-00024.
-
14.
Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N Engl J Med. 2020;382(23):2268-70. [PubMed ID: 32294339]. [PubMed Central ID: PMC7179967]. https://doi.org/10.1056/NEJMc2008597.
-
15.
Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18-22. [PubMed ID: 32240762]. [PubMed Central ID: PMC7146689]. https://doi.org/10.1016/j.bbi.2020.03.031.
-
16.
Hassani V, Amniati S, Ahmadi A, Mohseni M, Sehat-Kashani S, Nikoubakht N, et al. Emergency Tracheostomy in Two Airway Trauma Patients Suspected of COVID-19: A Case Report. Anesth Pain Med. 2020;10(4). e104648. [PubMed ID: 33134149]. [PubMed Central ID: PMC7539045]. https://doi.org/10.5812/aapm.104648.
-
17.
Papa A, Di Dato MT, Buonavolonta P, Saracco E, Salzano AM, Casale B. Clinical Management of Il-6 Driven Cytokine Storm Related to COVID-19 in a Patient with Recent Spinal Cord Stimulator Implants: A Case Report. Anesth Pain Med. 2020;10(4). e104151. [PubMed ID: 33134148]. [PubMed Central ID: PMC7539055]. https://doi.org/10.5812/aapm.104151.