Abstract
Background:
Spinal fusion surgery is often associated with heavy bleeding. Labetalol is one of the most effective drugs used to control bleeding in surgery.Objectives:
Here, we measured the effect of two therapeutic doses of labetalol on the amount of bleeding.Methods:
This is a randomized clinical trial that was performed in 2020-2021 in Al-Zahra hospital in Isfahan, Iran, on patients that were candidates for posterior spinal fusion surgery under general anesthesia. A total number of 64 patients were entered and randomized into two groups, one receiving labetalol at the dose of 2 mg/min and another group at 4 mg/min during surgery. The amount of bleeding in patients, heart rate, blood pressure, blood oxygen saturation, hypotension or bradycardia, and the mean length of stay in the recovery room were measured and compared between the groups.Results:
Extubation time (14 ± 4) and recovery time (76 ± 17) were significantly lower in patients that received labetalol (2 mg/min) compared to another group (21 ± 7 for intubation time and 116 ± 32 for recovery time (P < 0.001 for both items). Patients that received labetalol (4 mg/min) had significantly lower amounts of hemorrhage compared to other group (P = 0.001), and the surgeon's satisfaction was significantly higher in the second group (P = 0.001). The frequency of hypotension and bradycardia during the surgery were significantly higher among patients that received labetalol at the dose of 4 mg/min (P = 0.002 and P = 0.001, respectively). The patients in the group labetalol at 4 mg/min had also significantly lower systolic and diastolic blood pressure and lower mean arterial pressure (MAP) compared to the other group (P < 0.05).Conclusions:
Administration of labetalol at the dose of 4 mg/min had significantly desirable effects on hemodynamics that resulted in reduced bleeding volume and blood pressures compared to labetalol at the dose of 2 mg/min.Keywords
Bleeding Controlled Hypotension Hemodynamics Labetalol Spinal Fusion
1. Background
Spinal fusion surgery is often associated with heavy bleeding. The surgical procedure that causes a permanent connection between two or more vertebrae is known as spinal fusion surgery (1). Spinal fusion surgery completely prevents movement or friction between the two vertebrae, and is often performed on the lumbar spine, but can also be used to treat cervical and thoracic spine problems (2, 3).
This surgical procedure is one of the most important and common neurosurgery procedures. However, at the same time, like all surgeries, this type of surgery is associated with some complications, including bleeding at the operation site, infection, damage to nerve roots, nerve root tearing, and spinal cord injury (4-7).
Bleeding is sometimes so severe that it requires transfusions of blood and blood products (8). Bleeding can be troublesome not only in major surgeries, such as correction of deformities, but also in smaller fusion surgeries (9, 10). Reducing bleeding is important to maintain the patient's hemodynamic stability and to create a blood-free field with good vision for the surgeon (6, 11).
The latter aspect, especially in spinal surgery, is particularly sensitive during times of proximity to important and very fragile nerve structures (12, 13). The convenience of the surgeon's work shortens the duration of the operation, which in turn reduces the amount of bleeding (14).
Moreover, controlled hypotension is one of the methods that reduce bleeding from the surgical incision site, thereby providing technical freedom and better vision for the surgeon in terms of performing the operation more accurately. To control the hypotension, drugs, such as trimetaphan and pentolinium, vascular wall muscle relaxants, such as hydralazine, sodium nitroprusside, and beta-blockers, including propranolol, can be used (15, 16).
Labetalol is an adrenergic receptor blocking agent, which has a limited effect on alpha1-adrenergic adrenergic receptor and has the predominant effect on the beta-adrenergic receptor. Labetalol has been used successfully for other procedures in anesthesia, such as stress induced by laryngoscopy and intubation. The effect of labetalol begins 2 to 5 minutes after administration and has a half-life of 5 - 15 minutes (17).
More recently, there has been a tendency to use short half-life beta-blockers. However, side effects, including a reduction in seizure duration for electroconvulsive therapy, prolonged cardiovascular depression, and excessive hypotension have been reported (18, 19).
Labetalol is one of the most effective drugs used to control bleeding in surgery. Labetalol is a drug that has strong antihypertensive effects. The mechanism of action of this drug is antagonizing alpha and beta receptors (20). The use of this drug to control bleeding during surgery has been growing (21). However, there is no definitive protocol for the dose of labetalol used to control bleeding, and there is still controversy about the use of this drug.
2. Objectives
Due to the importance of bleeding in spinal cord surgery and especially vertebral fusion and the need to use effective techniques and treatments to control bleeding, as well as the fact that labetalol is known to be an effective drug in controlling bleeding, we decided to measure the effect of two different therapeutic doses of labetalol on the amount of bleeding in lumbar spine fusion surgeries in patients and compare them in our study.
3. Methods
This is a randomized clinical trial that was performed in 2020 - 2021 in Al-Zahra hospital affiliated with the Isfahan University of Medical Sciences. The current study was conducted on patients that were candidates for posterior spinal fusion surgery under general anesthesia.
The age of over 18 years, being candidates for posterior spinal fusion surgery at 4 levels, American Society of Anesthesiologists (ASA) classification equal to 1 or 2, and signing the written informed consent were the inclusion criteria in this study. Also, patients with any history of allergies to labetalol and patients with a history of heart blocks and a history of lung diseases, such as asthma did not enter the study
Patients with the following criteria were also excluded: (1) Reluctance to continue cooperation during the study, (2) any allergies to the drugs, (3) and changing the method of surgery and anesthesia.
The study protocol was approved by the Research Committee of the Isfahan University of Medical Sciences (IR.MUI.MED.REC. 1399.526). This study was also registered in the Iranian Registry of Clinical Trials (IRCT) with an identification registration code of IRCT20160307026950N30.
The required sample size was calculated to be 34 patients in each group using the sample size estimation formula to compare the means considering the 95% confidence level, 80% test power, the standard deviation of the mean blood pressure in controlled hypotension, which was about 1.5 (21), and the effect size of 0.8. Also, the data collector and the statistical analyst were unaware of the dose of labetalol injected into the patients. After analyzing the data, the codes were opened, and comparisons were made between groups. The sampling method was convenient.
The names of the patients were entered into the SPSS software and were randomized into two groups. The blinding method was considered, and the patient and the researcher were unaware of the type of injectable drug to the patients. The drugs were prepared in the same coded syringes by one of the operating room staff who was not aware of the study and were given to the researcher for injection.
A total number of 68 patients were entered based on inclusion criteria and were randomized into two groups. At the initial examination, vital signs, such as non-invasive monitoring, including (MAP) mean arterial pressure, systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and blood oxygen saturation (SPO2), were measured and recorded. General patient information, including age, sex, type of operation, underlying diseases, and patients' weights, were recorded in the data collection form.
All patients were placed under general anesthesia after pre-oxygenation and premedication with 0.05 - 0.03 mg/kg of midazolam, 2 μg/kg of fentanyl, 2 mg/kg of propofol, and 0.5 mg/kg of atracurium. After induction of anesthesia, patients were intubated and subjected to mechanical ventilation.
The patient's head was held at 20 degrees high, and all surgeries were performed by the same surgeon. Before surgery, labetalol injection was started if the patient's mean blood pressure was above 65 mmHg. Also, to start labetalol, the patient's heart rate must have been above 65 bpm. The first group consisted of 32 patients for whom labetalol (Alhavi Pharmaceutical Co. Tehran, Iran) was started at a dose of 0.25 mg/kg in 10 s, and then, the infusion was continued at 2 mg/min. The second group included patients for whom labetalol was started at a dose of 0.25 mg/kg in 10 s, and then, the infusion continued at 4 mg/min. If the heart rate fell below 50 bpm, the injection of labetalol was stopped, and if this value fell below 45 bpm, in addition to stopping labetalol, 0.5 mg of intravenous atropine was injected.
If the MAP fell below 60 mmHg, the injection of labetalol was stopped, and if this value fell below 55 mmHg, in addition to stopping labetalol, 5 mg of intravenous ephedrine was injected.
The amount of bleeding in patients was measured by the amount of blood suctioned during the operation, as well as the number of blood gauzes used. It should be noted that if the bleeding was not controlled, remifentanil was used at a dose of 0.01 mcg/kg/min. Each gauze that was completely soaked in blood was considered to be about 10 ml of blood.
The patient’s HR, BP, and SPO2 were also monitored. Complications of surgery, such as hypotension or bradycardia, mean length of stay in the recovery room, time of recovery of spontaneous respiration, and drop of oxygen saturation to less than 90% were also measured and compared in the two groups. Based on the modified Aldrete score, patients were discharged from recovery with a score of 9 - 10.
Data related to the patient’s bleeding volume and HR, BP, and patient's SPO2 during surgery were collected and statistically analyzed. The obtained data were entered into the Statistical Package for Social Sciences (SPSS) version 24. We used an independent t-test and repeated measures ANOVA to compare data between different time points and also different groups. A P-value < 0.05 was considered as the significance level.
4. Results
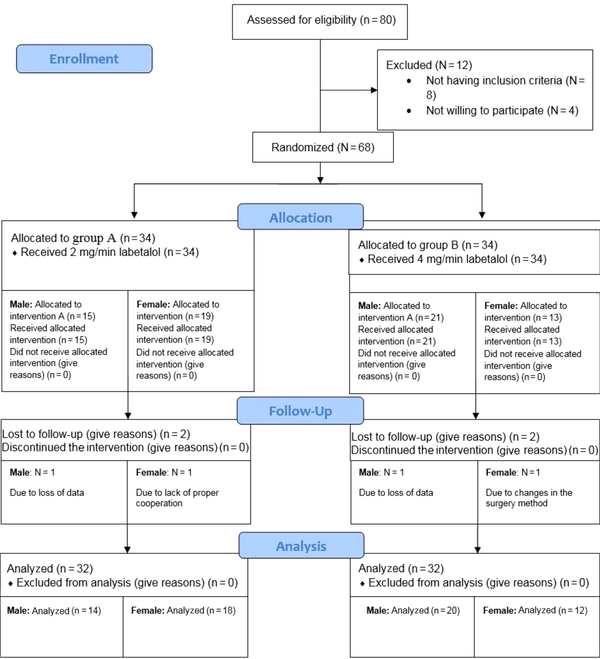
A total number of 68 patients were entered into the study and divided into two groups, each containing 34 patients. Two patients in each group were excluded due to changes in the surgery method (N = 3) and lack of proper cooperation (N = 1). The data of 64 patients were analyzed. The CONSORT flow diagram of patients is shown in Figure 1.
The CONSORT flow diagram of patients
The mean age of patients was 45 years in the first group that received labetalol at the dose of 2 mg/min and 46 years in the second group that received labetalol at the dose of 4 mg/min. There were no significant differences between the two groups of patients regarding age (P = 0.767) and gender (P = 0.133), but the mean body mass index (BMI) of patients in the second group was significantly higher than the first group (26.95 vs. 25.34, P = 0.029).
Also, extubation time (14 ± 4) and recovery time (76 ± 17) were significantly lower in patients that received labetalol at the dose of 2 mg/min compared to another group (21 ± 7 for extubation time and 116 ± 32 for recovery time (P < 0.001 for both items). Patients in the first group had also significantly lower amounts of ephedrine and higher amounts of remifentanil injections (P < 0.001 for both items). Based on our results, patients that received labetalol at the dose of 4 mg/min had significantly lower amounts of hemorrhage compared to the group that received labetalol at the dose of 2 mg/min (P = 0.001), and also the surgeon satisfaction was significantly higher in the second (labetalol at 2 mg/min) group (P = 0.001). These data are indicated in Table 1.
| Variable | Labetalol (2 mg/min) | Labetalol (4 mg/min) | P-Value |
|---|---|---|---|
| Age (y) | 45 ± 1.40 | 46 ± 1.36 | 0.767 |
| BMI (kg/m2) | 25.34 ± 4.1 | 26.95 ± 4.200 | 0.029 |
| Gender, No. (%) | 0.133 | ||
| Male | 14 (43.8) | 20 (62.5) | |
| Female | 18 (56.3) | 12 (37.5) | |
| Extubation time (min) | 14 ± 4.110 | 21 ± 7.140 | 0.000 |
| Recovery time (min) | 76 ± 17.010 | 116 ± 32.000 | 0.000 |
| Ephedrine (mg) | 1.3 ± 3.430 | 4.4 ± 3.840 | 0.000 |
| Remifentanil (mg) | 0.1 ± 0.200 | 0.0 ± 0.020 | 0.041 |
| Atropine (mg) | 0.1 ± 0.320 | 0.3 ± 0.910 | 0.751 |
| Hemorrhage volume (ml) | 668 ± 260 | 503 ± 342 | 0.001 |
| Surgeon satisfaction n (%) | 0.001 | ||
| Yes | 17 (53.1) | 30 (93.8) | |
| No | 4 (12.5) | 0 | |
| Null | 11 (34.4) | 2 (6.3) |
The frequency of hypotension and bradycardia during the surgery were significantly higher among patients that received labetalol at the dose of 4 mg/min (P = 0.002, P = 0.001 respectively). During recovery, the patients that received labetalol at the dose of 4 mg/min had significantly higher frequencies of nausea/vomiting (P = 0.006), total surgical complications (P < 0.001), and total complications during recovery (P < 0.001) (Table 2).
Comparison of Different Variables During Surgeries and Recovery Between Groups
| Variable | Group, No. (%) | P-Value | |
|---|---|---|---|
| A | B | ||
| Hypotension | 8 (25.0) | 20 (62.5) | 0.002 |
| Nausea and vomiting | 1 (3.1) | 1 (3.1) | 1.000 |
| Tachycardia | 1 (3.1) | 1 (3.1) | 1.000 |
| Bradycardia | 6 (18.8) | 19 (59.4) | 0.001 |
| Hypoxia | 0 (0.0) | 0 (0.0) | - |
| Hypotension recovery | 4 (12.5) | 7 (21.9) | 0.320 |
| N&V recovery | 10 (31.3) | 21 (65.6) | 0.006 |
| Tachycardia recovery | 2 (6.3) | 2 (6.3) | 1.000 |
| Bradycardia recovery | 4 (12.5) | 5 (15.6) | 1.000 |
| Hypoxia recovery | 0 (0.0) | 0 (0.0) | 0.000 |
| Total complications surgery | 0.000 | ||
| 0 | 18 (56.3) | 4 (12.5) | |
| 1 | 12 (37.5) | 15 (46.9) | |
| 2 | 2 (6.3) | 13 (40.6) | |
| Total complications recovery | 0.009 | ||
| 0 | 15 (46.9) | 4 (12.5) | |
| 1 | 14 (43.8) | 21 (65.6) | |
| 2 | 3 (9.4) | 7 (21.9) | |
The patients in the labetalol (4 mg/min) group had also significantly lower systolic and diastolic blood pressure and lower MAP compared to the labetalol (2 mg/min) group (P < 0.05) (Table 3).
Comparison of Systolic, Diastolic, and Mean Blood Pressure Between Patients
| Variable | Group | Z4 | P-Value** | Total P-Value*** | |
|---|---|---|---|---|---|
| A | B | ||||
| SBP (mmHg) | 0.000 | ||||
| Basal | 131 ± 14* | 130 ± 13 | -0.141 | 0.888 | |
| Before infusion | 131 ± 11 | 127 ± 11 | -1.512 | 0.130 | |
| After infusion | 115 ± 10 | 118 ± 11 | -1.151 | 0.250 | |
| 1st 15 minute | 109 ± 10 | 111 ± 10 | -1.056 | 0.291 | |
| 2nd 15 minute | 110 ± 11 | 107 ± 10 | -1.291 | 0.197 | |
| 3rd 15 minute | 109 ± 8 | 102 ± 9 | -2.55 | 0.011 | |
| 4th 15 minute | 111 ± 12 | 101 ± 10 | -3.051 | 0.002 | |
| 5th 15 minute | 111 ± 15 | 102 ± 10 | -2.533 | 0.011 | |
| 6th 15 minute | 113 ± 13 | 101 ± 11 | -3.575 | 0.000 | |
| 7th 15 minute | 112 ± 13 | 101 ± 13 | -3.036 | 0.002 | |
| 8th 15 minute | 113 ± 13 | 102 ± 13 | -2.984 | 0.003 | |
| P-value*** | 0.000 | 0.000 | |||
| DBP (mmHg) | 0.028 | ||||
| Basal | 85 ± 13 | 88 ± 11 | -1.317 | 0.188 | |
| Before infusion | 90 ± 22 | 87 ± 12 | -0.108 | 0.914 | |
| After infusion | 76 ± 12 | 79 ± 11 | -1.164 | 0.244 | |
| 1st 15 minute | 69 ± 8 | 71 ± 9 | -1.009 | 0.313 | |
| 2nd 15 minute | 69 ± 7 | 68 ± 11 | -0.283 | 0.777 | |
| 3rd 15 minute | 69 ± 9 | 66 ± 9 | -1.474 | 0.140 | |
| 4th 15 minute | 69 ± 10 | 65 ± 9 | -1.741 | 0.082 | |
| 5th 15 minute | 70 ± 13 | 66 ± 9 | -1.096 | 0.273 | |
| 6th 15 minute | 73 ± 12 | 65 ± 10 | -2.306 | 0.021 | |
| 7th 15 minute | 71 ± 11 | 66 ± 11 | -1.391 | 0.164 | |
| 8th 15 minute | 72 ± 11 | 67 ± 10 | -1.365 | 0.172 | |
| P-value | 0.000 | 0.000 | |||
| MAP (mmHg) | 0.015 | ||||
| Before infusion | 101 ± 12 | 101 ± 11 | -0.094 | 0.925 | |
| After infusion | 90 ± 11 | 93 ± 11 | -1.082 | 0.279 | |
| 1st 15 minute | 83 ± 9 | 87 ± 10 | -1.654 | 0.098 | |
| 2nd 15 minute | 84 ± 7 | 83 ± 10 | -0.437 | 0.662 | |
| 3rd 15 minute | 83 ± 8 | 81 ± 10 | -0.364 | 0.716 | |
| 4th 15 minute | 85 ± 10 | 80 ± 11 | -1.257 | 0.209 | |
| 5th 15 minute | 84 ± 13 | 81 ± 10 | -0.732 | 0.464 | |
| 6th 15 minute | 88 ± 11 | 80 ± 12 | -2.312 | 0.021 | |
| 7th 15 minute | 86 ± 11 | 81 ± 11 | -1.317 | 0.188 | |
| 8th 15 minute | 86 ± 11 | 83 ± 11 | -0.854 | 0.393 | |
| P-value | 0.000 | 0.000 | |||
5. Discussion
The effects of labetalol on reducing bleeding and other variables during spinal fusion were investigated in the current study. As mentioned earlier, labetalol has a significant effect on inducing hypotension leading to a reduction in the amount of bleeding; however, there is no definitive protocol for the effective dose of labetalol to control bleeding.
By comparing two distinctive dosages of labetalol, we showed that the amounts of bleeding and systolic and diastolic blood pressures were significantly lower in patients that received labetalol at the dose of 4 mg/min. We also showed that the frequency of bradycardia, hypotension, the duration of recovery, and surgeon satisfaction was significantly higher for the group of patients that received labetalol at the dose of 4 mg/min. These data support the effectiveness of labetalol (4 mg/min) in providing more desirable hypotension and reducing bleeding compared to labetalol at 2 mg/min.
Previous studies have also evaluated labetalol as an effective drug in providing hypotension during surgical procedures. Ortega-Gutierrez, in 2013 assessed the effects of labetalol infusion at a dose of 4 mg/min and nicardipine on bleeding volume of patients with intracerebral and subarachnoid hemorrhage. Based on their results, both drugs caused a significant reduction in blood pressure and bleeding volume, and labetalol at a dose of 4 mg/min could reduce bleeding (22). Another clinical trial was performed in 2020 by Ibrahim et al. on patients that were candidates of elective supratentorial craniotomy for tumor resection. They compared the infusion of 0.5 µg/kg/h of dexmedetomidine with equal volume and rate of normal saline 0.9% (control group). The results of their study showed that dexmedetomidine infusion without loading dose could be an efficacious and safe agent in achieving hemodynamic stability and could reduce bleeding (23). Another study was conducted by El-Shmaa et al. on patients undergoing sinus endoscopic surgery. In this report, it was indicated that the administration of labetalol at 2 - 5 mg/min resulted in a significant decrease in the amount of bleeding compared to nitroglycerin (24). However, in a study by JN et al., dexmedetomidine provided better hemodynamic stability and operative field visibility compared to labetalol during functional endoscopic sinus surgery (25). These data are in line with the findings of our study, showing that the injection of 4 mg/min of labetalol could be effective in reducing bleeding during surgical procedures. Another clinical trial was performed in 2016 by Sajedi et al on patients that were candidates for sinus endoscopy and compared the infusion of labetalol (2 mg/min) with remifentanil (0.25 - 0.5 μg/kg/min). The results of their study showed that the mean bleeding volume and the frequency of side effects were higher in the labetalol group (26). These can be indicative of the effectiveness of labetalol (2 mg/min) in reducing bleeding volume.
Based on our results, the administration of labetalol (4 mg/min) resulted in a reduction in blood pressures, bradycardia, and hypotension during surgical procedures compared to labetalol (2 mg/min). Attari et al. assessed patients undergoing craniotomy and showed that the administration of high-dose labetalol (4 mg/min) could result in a significant decrease in systolic and diastolic blood pressure and as a result, mean arterial blood pressure compared to labetalol at lower doses (27). Hecht and Richards showed that compared to nicardipine, the administration of labetalol (4 mg/min) caused significantly more bradycardia that required special care during surgical procedures (28). The frequency of hypotension was also indicated to be higher in patients treated with higher dosages of labetalol (28).
Based on our data, no significant differences were observed between groups of patients regarding the amount of pain and decreased oxygen saturation. Hoskins declared that labetalol was highly effective in reducing bleeding and blood pressure, but it had no significant effects on pain and other variables (29).
An important point of the current study was a significant increase in the surgeon satisfaction and recovery duration in patients that received labetalol at a dose of 4 mg/min. Ghodraty et al. compared the effects of labetalol at (4 mg/min) and nitroglycerine (1 mcg/kg/min) in patients undergoing rhinoplasty. This study showed that higher dosages of labetalol could reduce the bleeding volume during the surgical procedure leading to providing a better visual field for the surgeon and, as a result, increased surgeon satisfaction (30). On the other hand, Hadavi et al. reported shorter recovery durations for patients that were treated with labetalol (2 mg/min) compared to recovery duration with nitroglycerine (21). We believe that this observation can be due to a significant reduction in blood pressures in patients treated with higher doses of labetalol. Patients that received labetalol (4 mg/min) had significantly lower blood pressure compared to labetalol (2 mg/min); therefore, they required prolonged post-surgical care in the recovery room.
To date, no study has compared two different doses of labetalol, and this is the first clinical trial that compared the effects of labetalol at the doses of 2 mg/min and 4 mg/min on hemodynamic variables in patients.
5.1. Limitations
The sample size of our study was small; therefore, further studies are required for comparing different doses of labetalol and determining other adverse effects.
5.2. Conclusions
Overall, we showed that the administration of labetalol (4 mg/min) was significantly more effective on hemodynamics that resulted in reduced bleeding volume and blood pressures compared to labetalol at a dose of 2 mg/min. By comparison of various factors between these two dosages, we recommend that labetalol at a dose of 4 mg/min should be used in major surgical procedures that are associated with possible high bleeding volume in order to reduce the bleeding volume and increase surgeon satisfaction. These data were in line with previous studies.
Acknowledgements
References
-
1.
Sieberg CB, Simons LE, Edelstein MR, DeAngelis MR, Pielech M, Sethna N, et al. Pain prevalence and trajectories following pediatric spinal fusion surgery. J Pain. 2013;14(12):1694-702. [PubMed ID: 24290449]. [PubMed Central ID: PMC3873090]. https://doi.org/10.1016/j.jpain.2013.09.005.
-
2.
Postoperative Visual Loss Study Group. Risk factors associated with ischemic optic neuropathy after spinal fusion surgery. Anesthesiology. 2012;116(1):15-24. [PubMed ID: 22185873]. https://doi.org/10.1097/ALN.0b013e31823d012a.
-
3.
Harris IA, Dao AT. Trends of spinal fusion surgery in Australia: 1997 to 2006. ANZ J Surg. 2009;79(11):783-8. [PubMed ID: 20078526]. https://doi.org/10.1111/j.1445-2197.2009.05095.x.
-
4.
Rajaee SS, Kanim LE, Bae HW. National trends in revision spinal fusion in the USA: patient characteristics and complications. Bone Joint J. 2014;96-B(6):807-16. [PubMed ID: 24891583]. https://doi.org/10.1302/0301-620X.96B6.31149.
-
5.
Bohl DD, Webb ML, Lukasiewicz AM, Samuel AM, Basques BA, Ahn J, et al. Timing of Complications After Spinal Fusion Surgery. Spine (Phila Pa 1976). 2015;40(19):1527-35. [PubMed ID: 26230536]. https://doi.org/10.1097/BRS.0000000000001073.
-
6.
Janatmakan F, Nesioonpour S, Javaherforoosh Zadeh F, Teimouri A, Vaziri M. Comparing the Effect of Clonidine and Dexmedetomidine on Intraoperative Bleeding in Spine Surgery. Anesth Pain Med. 2019;9(1). e83967. [PubMed ID: 30881906]. [PubMed Central ID: PMC6408748]. https://doi.org/10.5812/aapm.83967.
-
7.
Moharari RS, Shahinpour S, Saeedi N, Sahraei E, Najafi A, Etezadi F, et al. Comparison of Intraoperative Infusion of Remifentanil Versus Fentanyl on Pain Management in Patients Undergoing Spine Surgery: A Double Blinded Randomized Clinical Trial. Anesth Pain Med. 2021;11(4). e115576. [PubMed ID: 34692435]. [PubMed Central ID: PMC8520674]. https://doi.org/10.5812/aapm.115576.
-
8.
Tarpada SP, Morris MT, Burton DA. Spinal fusion surgery: A historical perspective. J Orthop. 2017;14(1):134-6. [PubMed ID: 27872518]. [PubMed Central ID: PMC5107724]. https://doi.org/10.1016/j.jor.2016.10.029.
-
9.
Nagabhushan RM, Shetty AP, Dumpa SR, Subramanian B, Kanna RM, Shanmuganathan R. Effectiveness and Safety of Batroxobin, Tranexamic Acid and a Combination in Reduction of Blood Loss in Lumbar Spinal Fusion Surgery. Spine (Phila Pa 1976). 2018;43(5):E267-73. [PubMed ID: 28678111]. https://doi.org/10.1097/BRS.0000000000002315.
-
10.
Huang YH, Ou CY. Significant Blood Loss in Lumbar Fusion Surgery for Degenerative Spine. World Neurosurg. 2015;84(3):780-5. [PubMed ID: 25986203]. https://doi.org/10.1016/j.wneu.2015.05.007.
-
11.
Javaherforooshzadeh F, Monajemzadeh SA, Soltanzadeh M, Janatmakan F, Salari A, Saeed H. A Comparative Study of the Amount of Bleeding and Hemodynamic Changes between Dexmedetomidine Infusion and Remifentanil Infusion for Controlled Hypotensive Anesthesia in Lumbar Discopathy Surgery: A Double-Blind, Randomized, Clinical Trial. Anesth Pain Med. 2018;8(2). e66959. [PubMed ID: 30009153]. [PubMed Central ID: PMC6035495]. https://doi.org/10.5812/aapm.66959.
-
12.
Li G, Sun TW, Luo G, Zhang C. Efficacy of antifibrinolytic agents on surgical bleeding and transfusion requirements in spine surgery: a meta-analysis. Eur Spine J. 2017;26(1):140-54. [PubMed ID: 27671279]. https://doi.org/10.1007/s00586-016-4792-x.
-
13.
Taghipour Anvari Z, Afshar-Fereydouniyan N, Imani F, Sakhaei M, Alijani B, Mohseni M. Effect of clonidine premedication on blood loss in spine surgery. Anesth Pain Med. 2012;1(4):252-6. [PubMed ID: 24904810]. [PubMed Central ID: PMC4018704]. https://doi.org/10.5812/aapm.2197.
-
14.
Bosch P, Kenkre TS, Londino JA, Cassara A, Yang C, Waters JH. Coagulation Profile of Patients with Adolescent Idiopathic Scoliosis Undergoing Posterior Spinal Fusion. J Bone Joint Surg Am. 2016;98(20). e88. [PubMed ID: 27869629]. https://doi.org/10.2106/JBJS.16.00114.
-
15.
Jamaliya RH, Chinnachamy R, Maliwad J, Deshmukh VP, Shah BJ, Chadha IA. The efficacy and hemodynamic response to Dexmedetomidine as a hypotensive agent in posterior fixation surgery following traumatic spine injury. J Anaesthesiol Clin Pharmacol. 2014;30(2):203-7. [PubMed ID: 24803758]. [PubMed Central ID: PMC4009640]. https://doi.org/10.4103/0970-9185.130021.
-
16.
Qiu X, Tan Z, Tang W, Ye H, Lu X. Effects of controlled hypotension with restrictive transfusion on intraoperative blood loss and systemic oxygen metabolism in elderly patients who underwent lumbar fusion. Trials. 2021;22(1):1-9. [PubMed ID: 33509270]. [PubMed Central ID: PMC7841987]. https://doi.org/10.1186/s13063-020-05015-5.
-
17.
Ratnani E, Sanjeev OP, Singh A, Tripathi M, Chourasia HK. A Comparative Study of Intravenous Esmolol, Labetalol and Lignocaine in Low Doses for Attenuation of Sympathomimetic Responses to Laryngoscopy and Endotracheal Intubation. Anesth Essays Res. 2017;11(3):745-50. [PubMed ID: 28928581]. [PubMed Central ID: PMC5594800]. https://doi.org/10.4103/aer.AER_9_17.
-
18.
van den Broek WW, Leentjens AF, Mulder PG, Kusuma A, Bruijn JA. Low-dose esmolol bolus reduces seizure duration during electroconvulsive therapy: a double-blind, placebo-controlled study. Br J Anaesth. 1999;83(2):271-4. [PubMed ID: 10618942]. https://doi.org/10.1093/bja/83.2.271.
-
19.
Parikh DA, Garg SN, Dalvi NP, Surana PP, Sannakki D, Tendolkar BA. Outcome of four pretreatment regimes on hemodynamics during electroconvulsive therapy: A double-blind randomized controlled crossover trial. Ann Card Anaesth. 2017;20(1):93-9. [PubMed ID: 28074804]. [PubMed Central ID: PMC5290705]. https://doi.org/10.4103/0971-9784.197844.
-
20.
Peacock W, Hilleman DE, Levy PD, Rhoney DH, Varon J. A systematic review of nicardipine vs labetalol for the management of hypertensive crises. Am J Emerg Med. 2012;30(6):981-93. [PubMed ID: 21908132]. https://doi.org/10.1016/j.ajem.2011.06.040.
-
21.
Hadavi MR, Zarei Y, Tarogh S. Comparison of effects of labetalol and nitroglycerine on intraoperative blood loss and surgical field quality in rhinoplasty surgery. World J Plast Surg. 2015;4(1):60.
-
22.
Ortega-Gutierrez S, Thomas J, Reccius A, Agarwal S, Lantigua H, Li M, et al. Effectiveness and safety of nicardipine and labetalol infusion for blood pressure management in patients with intracerebral and subarachnoid hemorrhage. Neurocrit Care. 2013;18(1):13-9. [PubMed ID: 23055089]. https://doi.org/10.1007/s12028-012-9782-1.
-
23.
Ibrahim IM, Hassan R, Mostafa RH, Ibrahim MA. Efficacy of Dexmedetomidine Infusion Without Loading Dose on Hemodynamic Variables and Recovery Time During Craniotomy: A Randomized Double-blinded Controlled Study. Anesth Pain Med. 2021;11(2). e113410. [PubMed ID: 34336625]. [PubMed Central ID: PMC8314083]. https://doi.org/10.5812/aapm.113410.
-
24.
El-Shmaa NS, Ezz HAA, Younes A. The efficacy of Labetalol versus Nitroglycerin for induction of controlled hypotension during sinus endoscopic surgery. A prospective, double-blind and randomized study. J Clin Anesth. 2017;39:154-8. [PubMed ID: 28494895]. https://doi.org/10.1016/j.jclinane.2017.03.003.
-
25.
JN S, Kumar S, Vijay T. To Compare the Efficacy of Dexmedetomidine Versus Labetalol in Providing Controlled Hypotension in Functional Endoscopic Sinus Surgery. Anesth Pain Med. 2021;11(1). e108915. [PubMed ID: 34221935]. [PubMed Central ID: PMC8241463]. https://doi.org/10.5812/aapm.108915.
-
26.
Sajedi P, Rahimian A, Khalili G. Comparative evaluation between two methods of induced hypotension with infusion of Remifentanil and Labetalol during sinus endoscopy. J Res Pharm Pract. 2016;5(4):264-71. [PubMed ID: 27843963]. [PubMed Central ID: PMC5084484]. https://doi.org/10.4103/2279-042X.192463.
-
27.
Attari M, Tayyari F, Narimani N. Comparing the Effect of Labetalol versus Morphine on Controlling Blood Pressure and Pulse Rate during Emergence from Anesthesia after Craniotomy. Adv Biomed Res. 2017;6:127. [PubMed ID: 29142890]. [PubMed Central ID: PMC5672650]. https://doi.org/10.4103/2277-9175.216781.
-
28.
Hecht JP, Richards PG. Continuous-Infusion Labetalol vs Nicardipine for Hypertension Management in Stroke Patients. J Stroke Cerebrovasc Dis. 2018;27(2):460-5. [PubMed ID: 29092768]. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.09.023.
-
29.
Hoskins MH, Leleiko RM, Ramos JJ, Sola S, Caneer PM, Khan BV. Effects of labetalol on hemodynamic parameters and soluble biomarkers of inflammation in acute coronary syndrome in patients with active cocaine use. J Cardiovasc Pharmacol Ther. 2010;15(1):47-52. [PubMed ID: 20133495]. https://doi.org/10.1177/1074248409358409.
-
30.
Ghodraty M, Khatibi A, Rokhtabnak F, Maleki M, Parsa F. Comparing Labetalol and Nitroglycerine on Inducing Controlled Hypotension and Intraoperative Blood Loss in Rhinoplasty: A Single-Blinded Clinical Trial. Anesth Pain Med. 2017;7(5). https://doi.org/10.5812/aapm.13677.
