Abstract
Background:
Airway protection during anesthesia is often the primary concern of anesthetists when working with obese patients and always is a difficult task due to increased exposure to harmful effects of apnea, hypoxia, and impaired respiratory mechanics.Objectives:
The primary goal of this research was to determine the diagnostic accuracy of combined Mallampati and Wilson score in detecting difficult intubation in obese patients undergoing surgery by taking the Cormack-Lehane grading on direct laryngoscopy and intubation as the gold standard.Methods:
This descriptive cross-sectional study was done in 300 obese patients with BMI > 29.9 kg/m2. Modified Mallampati and Wilson score was recorded preoperatively for each patient in the sitting position by the primary investigator. Endotracheal intubation grades were also recorded, and grades IIb, III, and IV were regarded as difficult intubation according to the Cormack-Lehane intubation classification.Results:
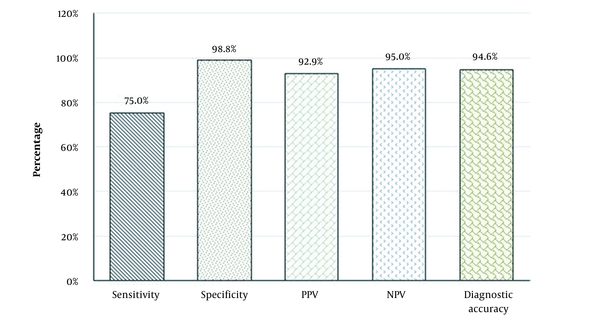
The mean age was 46.76 ± 15.57 years. The sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of the combined Mallampati and Wilson score for detecting difficult laryngoscopy and difficult intubation were 75.0, 98.8, 92.9, 95.0, and 94.6%, respectively.Conclusions:
Combined Mallampatti and Wilson score is highly accurate in the initial diagnostic workup of obese patients at risk of difficult intubation. It is easy to calculate and lower the risk of intubation-related complications and failure.Keywords
Combined Mallampatti and Wilson Score Cormack and Lehane Diagnostic Accuracy Difficult Intubation Difficult Laryngoscopy
1. Background
Obesity is a universal problem, with about 2.1 billion of the world’s population being overweight and obese. The age trend of overweight and obesity in developing countries is comparable to developed countries. According to the World Health Organization, BMI > 30 kg/m2 is categorized as obese, and that falling between 25 and 29.9 kg/m2 shows overweight (1). Airway management during anesthesia is always the primary concern of anesthetists when dealing with obese patients and often is a challenging task due to increased sensitivity to harmful effects of apnea, hypoxia, and impaired respiratory mechanics (2). About 30% of anesthesia-related mortalities can compromise airways (3). Operating a global scale, an estimated 600 people a year are killed by difficult or impossible intubation (4). The occurrence of difficult laryngoscopy and intubation in lean patients is 6.2%, while it varies 8.2 - 16.2% in obese people (5).
Many bedside tests are available to predict a difficult airway, including Mallampatti, Sternomental reach, and upper lip bite test (ULBT). However, no independent studies could predict the difficult airway with consistent precision (6). To evaluate the airway, several tests, which are a combination of independent measures, have been identified. These bedside tests did not gain attention because they were cumbersome to conduct. The degree of inter-observer variability in preoperative airway exams varies among studies.
2. Objectives
The Wilson score (7) is already an established test due to its subjective parameters. Therefore, our goal in this research was to determine the diagnostic accuracy of combined Mallampatti and Wilson score in detecting difficult intubation in obese patients undergoing surgery by taking Cormack-Lehane grading on direct laryngoscopy and intubation as the gold standard.
3. Methods
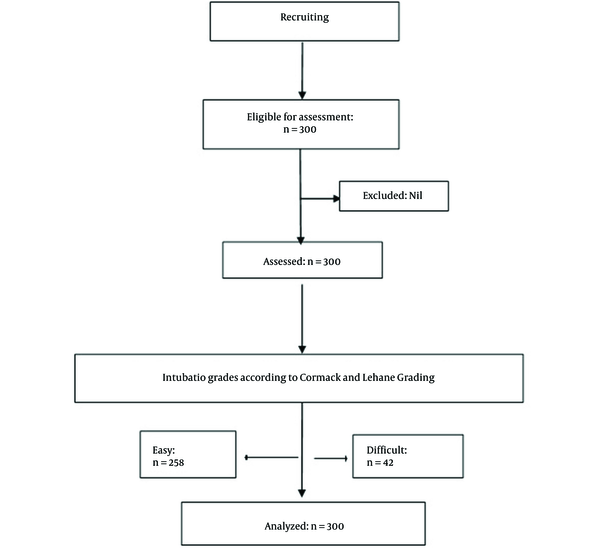
This descriptive cross-sectional study was conducted after approval from the hospital ethics review committee. Written informed consent was obtained from all patients enrolled in the study. A total of 300 patients from both genders aged 18 to 70 years with BMI > 29.9 kg/m2 were included in the study (Figure 1). Patients who were unable to sit up, had a distortion in anatomy (head and neck swellings, cancers, cervical spine diseases, previous surgery, and rheumatoid arthritis), used a cervical collar (cervical spondylosis, previous cervical spine surgery) and those candidates for obstetric and cardiac surgeries were excluded.
Flow chart of study patients
The modified Mallampati and Wilson score (Table 1) was recorded for each individual in preoperative evaluation. For this purpose, patients were asked to sit, and the primary investigator performed a combined Mallampatti and Wilson score examination. Blood pressure, ECG, and oxygen saturation of the patients were monitored using a Datex-Omheda AS-3 monitor (GE Healthcare, Finland). General anesthesia was provided using intravenous propofol 2 mg/kg as the induction agent, followed by a depolarizing or non-depolarizing muscle blocking agent (succinylcholine 1.5 mg/kg or atracurium 0.5 mg/kg) depending on the technique of induction chosen by the primary anesthetist. Upon completing the standard time of ideal muscle relaxation, direct laryngoscopy was proceeded by the primary anesthetist (with at least two years of anesthesia experience). The number of attempts, the type (straight or curved) and size of the blade (3 or 4), the type of muscle relaxant used, and the use of bougie were recorded. Intubation grades IIb, III, and IV were regarded as difficult intubation according to the Cormack-Lehane classification.
Wilson Score
| Risk Factor and Wilson Score | Level |
|---|---|
| Weight (kg) | |
| 0 | < 90 |
| 1 | 90 - 110 |
| 2 | > 110 |
| Head and neck movement (deg) | |
| 0 | Above 90 |
| 1 | About 90 |
| 2 | Below 90 |
| Jaw movement | |
| 0 | IG > 5cm or SLux > 0 |
| 1 | IG < 5cm and SLux = 0 |
| 2 | IG < 5cm and SLux < 0 |
| Receding mandible | |
| 0 | Normal |
| 1 | Moderate |
| 2 | Severe |
| Buck's teeth | |
| 0 | Normal |
| 1 | Moderate |
| 2 | Severe |
Sample size calculation was based on a previous study. De Jong et al. (5) reported that the incidence of difficult intubation in obese patients was 24.5% (16.3% in intensive care unit and 8.2% in operating room). We assumed that the expected (clinician experience) sensitivity for the combined Mallampati and Wilson score was 80%. Based on the formula [N Sen = (Zα/2)2 Sensitivity (1-Sensitivity)/d2x Prevalence (8)], 300 obese cases were needed to estimate expected sensitivity and prevalence within a 9% margin of error at a 95% confidence interval [Zα/2 = 1.96, sensitivity = 0.80, 1-sensitivity = 0.20, d2 = 0.03, prevalence = 24.5%, n = 3.17 round, n = 3.17].
Data were analyzed with SPSS Version 22. Frequency and percentage were for computed categorical data, such as gender, the level of the anesthetist performing laryngoscopy, use of bougie, number of attempts, and Cormack-Lehane grading. Means and standard deviations were computed for age, height, weight, BMI, and modified Mallampatti and Wilson Score. Sensitivity, specificity, PPV, NPV, and accuracy were computed for the combination of modified Mallampati score and Wilson risk score to predict difficult intubation, while Cormack-Lehane classification on direct laryngoscopy was taken as the gold standard.
4. Results
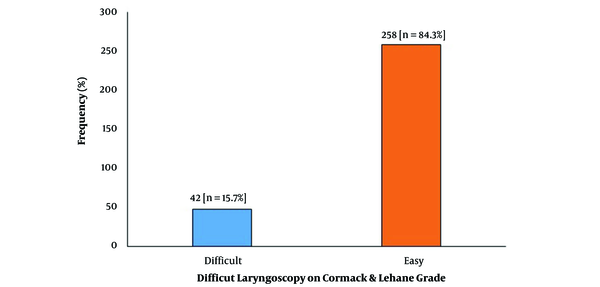
Three hundred obese adult patients planned for the surgical procedure under general anesthesia with tracheal intubation were analyzed. Of them, 156 (52%) were males, and 144 (48%) were females. Other demographic data of the study population are presented in Table 2. The outcomes of combined modified Mallampatti and Wilson score and Cormack-Lehane grading for predicting difficult intubation are shown in Table 3. Among 300 patients, 42 patients had difficult intubation with an overall incidence of 14%, shown in Figure 2. The sensitivity of the combined modified Mallampatti and Wilson score for predicting difficult intubation was 75%; however, specificity, positive predictive value, negative predictive value, and diagnostic accuracy were above 90%, as shown in Figure 3. Out of 300 obese patients, 213 (71%) had a BMI of 31 to 35 kg/m2, and 87 (29%) had a BMI of 35 to 39 kg/m2. Diagnostic accuracy of combined modified Mallampatti and Wilson score for predicting difficult intubation according to BMI is shown in Table 4.
Demographic Data of Patients
| Variables | Mean ± SD | Min - Max |
|---|---|---|
| Age (y) | 46.76 ± 15.57 | 18 - 70 |
| Height (cm) | 140.04 ± 14.51 | 120 - 180 |
| Weight (kg) | 102.84 ± 28.02 | 52 - 154 |
| NMI (kg/m2) | 36.21 ± 2.14 | 31 - 39 |
Results of Combined Mallampati and Wilson Scores
| Cormack-Lehane Grading | Combined Modified Mallampatti and Wilson Score | Total | |
|---|---|---|---|
| Difficult | Easy | ||
| Difficult (IIb, III and IV) | 39 (TP) | 13 (FN) | 52 |
| Easy (I and II) | 03 (FP) | 245 (TN) | 248 |
| Total | 42 | 258 | 300 |
Incidence of difficult intubation by Cormack-Lehane grading distribution
Diagnostic accuracy of combined modified Mallampatti and Wilson score for predicting difficult intubation by taking Cormack-Lehane grading as the gold standard (PPV, positive predictive value; NPV, negative predictive value).
Diagnostic Accuracy of Combined Modified Mallampatti and Wilson Score for Predicting Difficult Intubation According to BMI a
| Variables and Cutoff | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|
| BMI (kg/m2) | |||||
| 31 - 35 | 31/41 (75.6) | 170/172 (98.8) | 31/33 (93.8) | 170/180 (94.4) | 210/213 (98.5) |
| 35.1 - 39 | 8/11 (72.7) | 75/76 (98.7) | 8/9 (88.9) | 75/78 (96.2) | 83/87 (95.4) |
| P-value | 0.84 | 0.94 | 0.62 | 0.56 | 0.096 |
5. Discussion
Dealing with difficult airways with inappropriate preparation and improper management is the leading cause of complications in anesthetic practice. Endotracheal intubation can be connected with minor complications such as gashes of the lips or broken teeth. It can also be linked with possibly deadly complications such as aspiration pneumonia and respiratory distress or acute respiratory distress syndrome (ARDS). Aspiration pneumonia or obscure intubation of the esophagus can also lead to possible fetal anoxia (9). The presence of varied airway anatomy or other uncontrolled variables should be carefully evaluated before proceeding to tracheal intubation to prevent airway-related complications. The accurate preoperative evaluation and identification of possible difficult intubation may result in lower rates of anesthetic complications, predominantly in obese patients (10, 11).
To predict difficult airway, difficult mask ventilation, and tracheal intubation, several classification systems have been developed in addition to the Cormack-Lehane classification, including the Intubation Difficulty Scale (IDS) and the Mallampati score. Although these medical scoring systems can help with patient evaluation, no single or combination of scores can be trusted to classify all of them (12). Challenging endotracheal intubation can cause the failure of intubation, which may lead to hypoxia and hypoxemia (13-16). Benumof (17) reported difficult endotracheal intubation in 1 - 4% of cases with 0.05 - 0.35% of intubation failure.
Difficult endotracheal intubation is described as using three endotracheal intubation attempts with a standard laryngoscope or 10 minutes or more of endotracheal intubation (18). However, the concept of difficulty endotracheal intubation is very subjective, and the degree of difficulty is hard to measure. Therefore, Adnet et al. (19) developed the Intubation Difficulty Scale (IDS) classified based on objective categories of endotracheal intubation difficulty: (1) simple endotracheal intubation; (2) relatively difficult endotracheal intubation; and (3) very difficult endotracheal intubation.
Since the arrival of video laryngoscopes, the significance of Cormack-Lehane intubation grading is under debate and becoming common, primarily to support tracheal intubation in patients with difficult airways. Mines and Ahmad (20) are concerned about using the Cormack-Lehane grading system as a clinical knowledge input instrument during video laryngoscopy. When Cormack and Lehane developed their grading system, the goal was to promote training and assist in direct laryngoscopy decision-making. Since then, the system has been commonly used to support decision-making and preparation on anesthetic records. The Cormack-Lehane grading has served this function well for direct laryngoscopy while not intended as a knowledge-sharing method. Cormack-Lehane video laryngoscopy scoring can confuse the direct scoring of laryngoscopy and may potentially be hazardous if not applied to the proper device type. It is essential to have a grading system for video laryngoscopes that identifies the type of device used, ease of view, mechanism used to pass the endotracheal tube (e.g., bougie, stylet), and difficulty in the passing of the endotracheal tube.
The Wilson score is used for routine evaluation based on criteria for assessing the physical characteristics of predicting the difficult endotracheal intubation before anesthesia. Airway assessments are often used, depending on the individual, job scenario, and study method. However, researchers suggested that certain factors be included in airway assessment to predict challenging endotracheal intubation, including Wilson score, BMI, neck circumference (NC) to Thyromental (TM) distance ratio, and ULBT (21-23). There are numerous tests to predict difficult intubation. Several studies have shown low diagnostic accuracy of tests when used independently. Combinations of individual tests or risk factors may add to the diagnostic value when compared with the value of each test separately (24).
Different studies have predicted the value of screening tests to predict difficult intubation, which can vary from each other. This variation could be different based on the patient’s physical characteristics, as most of these studies were conducted in the Western world. There is a substantial difference in Asian and European anthropometric measures, which is also represented in the anatomical markers used to predict difficulty in intubation. It is necessary to determine whether the same parameters and cutoff values can predict difficult airways within the Asian population. Dhanger et al. (25) performed an Indian population analysis to assess the diagnostic accuracy of NC to TM distance ratio and performance of Mallampatti score, showing difficult intubation with an incidence of 13%. In our study, the rate of difficult intubation was 17.3%, Oates et al. (23) compared Mallampati and Wilson's score for predicting difficult laryngoscopy and assessing the inter-observer variations in performing these tests. They found that both tests had reduced predictive powers, although they preferred the Wilson score for airway assessment.
Obesity as a modern worldwide epidemic is increasingly met in anesthesia practice. In this view, Brodsky et al. (13) conducted a study to show if large NC and high Mallampati scores were the only reliable predictors of difficult intubation. That study was further supported by Ezri et al. (26), who showed that the magnitude of BMI had no relevance with difficulty laryngoscopy. The variety and independence of teeth design and mandibular movement have vital roles in promoting laryngoscopic intubation. A study by Khan et al. (27) compared the upper lip bite test (ULBT) with Modified Mallampati test (MMT). The ULBT showed significantly higher specificity and accuracy than the MMT (P < 0.001). The ULBT was visibly evaluated by Eberhart et al. (28), showing the better reliability of inter-observers compared with MMT. Nevertheless, both tests had low predictive capacity, suggesting that both tests are low predictors of difficult intubation when used alone.
A double-blind, prospective study was done on 426 ASA I-II adult patients undergoing urologic and general surgery with general anesthesia. They recorded Mallampati score, tyromental/sternomental distances, lower jaw protrusion, neck movement, BMI, teeth morphology, guidewire use, and Wilson score before anesthesia. Each parameter was calculated for sensitivity, specificity, positive predictive value, and negative predictive value. They found P values < 0.05 (5%) and concluded that the Wilson score was the best predictive test among all (29).
Parashar et al. (30) assessed 197 ASA grade I and II obese patients (BMI ≥ 25 kg/m2) for NC/TM ratio, Mallampatti grade, and Wilson score using the Intubation Difficulty Scale (IDS). They estimated the prevalence of difficult intubation in obese populations and concluded that the combination of tests increases the diagnostic value. Our study further endorsed this study and found that the combined Mallampati and Wilson score is the most accurate predictor of difficult intubation, especially in obese patients.
Our study has some limitations. They include no standardization of the induction technique and the type of muscle relaxant used. Another limitation was the airway assessment and labeling of intubation grades done by different persons, which may add to the matter of subjectivity. We also did not measure NC, which might be an essential factor in predicting difficult laryngoscopies.
5.1. Conclusions
The Mallampati and Wilson scores are good predictors of adverse tracheal intubation in adult obese patients of both genders. This study confirmed that BMI could be a reliable predictor of possible difficult tracheal intubation. Hence, adding the combined score can prevent potentially fatal effects of adverse tracheal intubation in patients with high BMI. Besides, it can contribute to improved patient care and enhanced patient safety.
References
-
1.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766-81. [PubMed ID: 24880830]. [PubMed Central ID: PMC4624264]. https://doi.org/10.1016/S0140-6736(14)60460-8.
-
2.
Abedini N, Parish M, Farzin H, Pourfathi H, Akhsham M. The Determination of an Appropriate Time for Placement of the Classic Laryngeal Mask Airway in Patients Undergoing General Anesthesia. Anesth Pain Med. 2018;8(2). e64427. [PubMed ID: 30009152]. [PubMed Central ID: PMC6035496]. https://doi.org/10.5812/aapm.64427.
-
3.
Salimi A, Farzanegan B, Rastegarpour A, Kolahi AA. Comparison of the upper lip bite test with measurement of thyromental distance for prediction of difficult intubations. Acta Anaesthesiol Taiwan. 2008;46(2):61-5. [PubMed ID: 18593650]. https://doi.org/10.1016/S1875-4597(08)60027-2.
-
4.
Naguib TM, Ahmed SA. Evaluation of Flexible Laryngeal Mask Airway((R)) in Tongue Trauma Repair: A Randomized Trial. Anesth Pain Med. 2019;9(4). e92929. [PubMed ID: 31750096]. [PubMed Central ID: PMC6820298]. https://doi.org/10.5812/aapm.92929.
-
5.
De Jong A, Molinari N, Pouzeratte Y, Verzilli D, Chanques G, Jung B, et al. Difficult intubation in obese patients: incidence, risk factors, and complications in the operating theatre and in intensive care units. Br J Anaesth. 2015;114(2):297-306. [PubMed ID: 25431308]. https://doi.org/10.1093/bja/aeu373.
-
6.
el-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82(6):1197-204. [PubMed ID: 8638791]. https://doi.org/10.1097/00000539-199606000-00017.
-
7.
Javaherforooshzadeh F, Gharacheh L. The Comparison of Direct Laryngoscopy and Video Laryngoscopy in Pediatric Airways Management for Congenital Heart Surgery: A Randomized Clinical Trial. Anesth Pain Med. 2020;10(3). e99827. [PubMed ID: 32944555]. [PubMed Central ID: PMC7472645]. https://doi.org/10.5812/aapm.99827.
-
8.
Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014;48:193-204. [PubMed ID: 24582925]. https://doi.org/10.1016/j.jbi.2014.02.013.
-
9.
Zhang GH, Xue FS, Li P, Sun HY, Liu KP, Xu YC, et al. Effect of fiberoptic bronchoscope compared with direct laryngoscope on hemodynamic responses to orotracheal intubation. Chin Med J (Engl). 2007;120(4):336-8. [PubMed ID: 17374287].
-
10.
Seyedhejazi M, Sheikhzade D, Aliakbari Sharabiani B, Abri R, Sadeghian M. Evaluating the Effects of Post-Intubation Endotracheal Suctioning Before Surgery on Respiratory Parameters in Children with Airway Secretion. Anesth Pain Med. 2019;9(3). e86486. [PubMed ID: 31497517]. [PubMed Central ID: PMC6712427]. https://doi.org/10.5812/aapm.86486.
-
11.
Xue FS, Liao X, Liu HP, Xiong J, Yuan YJ, Liu JH. Use of the gum elastic bougie during endotracheal intubation in emergent patients with difficult airways. J Emerg Med. 2015;48(4):472-3. [PubMed ID: 25836569]. https://doi.org/10.1016/j.jemermed.2011.11.003.
-
12.
Kalra P. Miller's Anesthesia, Volumes 1 and 2, 7th Edition. Anesthesiology. 2010;112(1):260-1. https://doi.org/10.1097/ALN.0b013e3181c5dc06.
-
13.
Brodsky JB, Lemmens HJ, Brock-Utne JG, Vierra M, Saidman LJ. Morbid obesity and tracheal intubation. Anesth Analg. 2002;94(3):732-6. [PubMed ID: 11867407]. https://doi.org/10.1097/00000539-200203000-00047.
-
14.
Karkouti K, Rose DK, Wigglesworth D, Cohen MM. Predicting difficult intubation: A multivariable analysis. Can J Anaesth. 2000;47(8):730-9. [PubMed ID: 10958088]. https://doi.org/10.1007/BF03019474.
-
15.
Hekiert AM, Mandel J, Mirza N. Laryngoscopies in the obese: Predicting problems and optimizing visualization. Ann Otol Rhinol Laryngol. 2007;116(4):312-6. [PubMed ID: 17491533]. https://doi.org/10.1177/000348940711600416.
-
16.
Kim JA, Lee JJ. Preoperative predictors of difficult intubation in patients with obstructive sleep apnea syndrome. Can J Anaesth. 2006;53(4):393-7. [PubMed ID: 16575040]. https://doi.org/10.1007/BF03022506.
-
17.
Hassani V, Amniati S, Ahmadi A, Mohseni M, Sehat-Kashani S, Nikoubakht N, et al. Emergency Tracheostomy in Two Airway Trauma Patients Suspected of COVID-19: A Case Report. Anesth Pain Med. 2020;10(4). e104648. [PubMed ID: 33134149]. [PubMed Central ID: PMC7539045]. https://doi.org/10.5812/aapm.104648.
-
18.
Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-70. [PubMed ID: 23364566]. https://doi.org/10.1097/ALN.0b013e31827773b2.
-
19.
Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, et al. The intubation difficulty scale (IDS): Proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87(6):1290-7. [PubMed ID: 9416711]. https://doi.org/10.1097/00000542-199712000-00005.
-
20.
Mines R, Ahmad I. Can you compare the views of videolaryngoscopes to the Macintosh laryngoscope? Anaesthesia. 2011;66(4):315-7. [PubMed ID: 21401552]. https://doi.org/10.1111/j.1365-2044.2011.06685.x.
-
21.
Amri P, Nikbakhsh N, Modaress SR, Nosrati R. Upper Airway Nerve Block for Rigid Bronchoscopy in the Patients with Tracheal Stenosis: A Case Serie. Anesth Pain Med. 2020;10(4). e99796. [PubMed ID: 33134141]. [PubMed Central ID: PMC7539043]. https://doi.org/10.5812/aapm.99796.
-
22.
Mohammadi M, Khafaee Pour Khamseh A, Varpaei HA. Invasive Airway "Intubation" in COVID-19 Patients; Statistics, Causes, and Recommendations: A Review Article. Anesth Pain Med. 2021;11(3). e115868. [PubMed ID: 34540642]. [PubMed Central ID: PMC8438719]. https://doi.org/10.5812/aapm.115868.
-
23.
Oates JD, Macleod AD, Oates PD, Pearsall FJ, Howie JC, Murray GD. Comparison of two methods for predicting difficult intubation. Br J Anaesth. 1991;66(3):305-9. [PubMed ID: 2015145]. https://doi.org/10.1093/bja/66.3.305.
-
24.
Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006;102(6):1867-78. [PubMed ID: 16717341]. https://doi.org/10.1213/01.ane.0000217211.12232.55.
-
25.
Dhanger S, Gupta SL, Vinayagam S, Bidkar PU, Elakkumanan LB, Badhe AS. Diagnostic accuracy of bedside tests for predicting difficult intubation in Indian population: An observational study. Anesth Essays Res. 2016;10(1):54-8. [PubMed ID: 26957691]. [PubMed Central ID: PMC4767095]. https://doi.org/10.4103/0259-1162.165503.
-
26.
Ezri T, Gewurtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58(11):1111-4. [PubMed ID: 14616599]. [PubMed Central ID: PMC1283106]. https://doi.org/10.1046/j.1365-2044.2003.03412.x.
-
27.
Khan ZH, Kashfi A, Ebrahimkhani E. A comparison of the upper lip bite test (a simple new technique) with modified Mallampati classification in predicting difficulty in endotracheal intubation: a prospective blinded study. Anesth Analg. 2003;96(2):595-9. [PubMed ID: 12538218]. https://doi.org/10.1097/00000539-200302000-00053.
-
28.
Eberhart LH, Arndt C, Cierpka T, Schwanekamp J, Wulf H, Putzke C. The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: An external prospective evaluation. Anesth Analg. 2005;101(1):284-9. [PubMed ID: 15976247]. https://doi.org/10.1213/01.ANE.0000154535.33429.36.
-
29.
Domi R. The best prediction test of difficult intubation. J Anaesthesiol Clin Pharmacol. 2010;26(2):193-6.
-
30.
Parashar S, Pathak A, Harjai M, Chandra G. Comparison of Ratio of The Neck Circumference To Thyromental Distance, Mallampati Score, wilson Score As Predictor of Difficult Intubation in Obese Patients. Age. 2017;43(13.54):16-76.