Abstract
Background:
The number of patients with obesity undergoing various surgeries is increasing annually, and ventilation problems are highly prevalent in these patients.Objectives:
We aimed to evaluate ventilation effectiveness with pressure-controlled (PC) and volume-controlled (VC) ventilation modes during laparoscopic bariatric surgery.Methods:
In this open-label randomized crossover clinical trial, 40 adult patients with morbid obesity candidates for laparoscopic bariatric surgery were assigned to VC-PC or PC-VC groups. Each patient received both ventilation modes sequentially for 15 min during laparoscopic surgery in a random sequence. Every 5 min, exhaled tidal volume, peak and mean airway pressure, oxygen saturation, heart rate, mean arterial pressure, and end-tidal CO2 were recorded. Blood gas analysis was done at the end of 15 min. Dynamic compliance, PaO2/FiO2 ratio, P (A-a) O2 gradient, respiratory dead space, and PaCO2-ETCO2 gradient were calculated according to the obtained results.Results:
The study included 40 patients with a mean age of 35.13 ± 9.06 years. There were no significant differences in peak and mean airway pressure, dynamic compliance, and hemodynamic parameters (P > 0.05). There was no significant difference between the two ventilation modes in pH, PaCO2, PaO2, PaO2/FIO2, dead space volume, and D (A-a) O2 at different time intervals (P > 0.05).Conclusions:
If low tidal volumes are used during adult laparoscopic bariatric surgery, mechanical ventilation with PC mode is not superior to VC mode.Keywords
Morbid Obesity Bariatric Surgery Volume-Controlled Ventilation Pressure-Controlled Ventilation
1. Background
The prevalence of obesity as a significant public health problem is increasing worldwide (1-3). Today various medical and surgical treatments are used to lose weight, and the number of patients with obesity undergoing bariatric or non-bariatric surgery is increasing annually. Obesity predisposes to various perioperative complications and changes in the respiratory system that eventually lead to increased airway resistance, decreased compliance, and impaired gas exchange (4). In anesthetized patients, functional residual capacity (FRC), partial pressure of oxygen (PaO2), and pulmonary compliance are inversely related to body mass index (BMI) (5). Finally, intraoperative respiratory changes can lead to postoperative complications, longer hospital stays, and mortality (6).
The traditional ventilation method in bariatric surgery is the volume-controlled ventilation (VCV) mode. The main disadvantage of this mode is increased airway pressure due to reduced compliance and increased resistance, potentially increasing the risk of lung barotrauma (7). Pressure-controlled ventilation (PCV) can be used in these patients as an alternative. The maximum airway pressure is limited in this mode, so the amount of tidal volume (TV) and minute ventilation is variable (8). Some studies have shown that the PCV mode can improve arterial and tissue oxygenation and increase alveolar recruitment (7-10). The optimal method of ventilation in these patients has not yet been determined. We compared ventilation effectiveness with PCV and VCV modes in patients with obesity undergoing laparoscopic bariatric surgery. Given the benefits of the PCV mode, we hypothesized that its use in these patients could improve gas exchange and improve the mechanical variables of the respiratory system.
2. Methods
This study is a prospective randomized open-label crossover trial with a per-protocol design in a university teaching hospital. The study protocol, data collection tool, and informed consent forms were approved by the Institutional Review Board (IR.IUMS.FMD.REC.1398.150). Also, the study was registered in the Iranian registry for clinical trials (IRCT20121107011398N14).
Study cases were screened from patients candidate for laparoscopic bariatric surgery. Inclusion criteria were as follows: BMI > 40 kg/m2, age over 18 years, no severe pulmonary disease (according to a clinical exam and the results of spirometry), and no advanced cardiovascular disease (functional class I and no abnormal echocardiographic and electrocardiographic findings). Exclusion criteria were as follows: Patient refusal, inability to maintain ventilator settings for 15 min, failure to maintain a proper ET-CO2 (30 - 40 mmHg), and change of laparoscopic surgery to laparotomy.
2.1. Randomization and Intervention
After taking informed consent, patients were divided into two groups using a random number table extracted from the computer. The study groups were group 1 (VC-PC) and group 2 (PC-VC). After anesthesia induction and endotracheal intubation in the VC-PC group, the patient was ventilated by VCV, which continued for 15 min after blowing CO2 in the abdomen and starting surgery. Then, the ventilation mode changed to PCV until the end of the surgery. The PCV was initiated in group 2 (PC-VC) and then switched to VCV 15 min after pneumoperitoneum. Anesthetic monitoring included standard American Society of Anesthesiologists monitors. The supine position with 25 degrees of head-up was used for all patients during the procedure. After 3 min preoxygenation with 100% oxygen and administration of premedication (2 µg/kg of fentanyl and 15 µg/kg of midazolam based on total body weight (TBW)), rapid-sequence induction of anesthesia was performed using intravenous propofol 1.5 - 2 mg/kg based on ideal body weight (IBW) and succinylcholine 1 mg/kg based on TBW. Tracheal intubation was performed using an appropriately sized PVC endotracheal tube. For the maintenance of anesthesia, an infusion of propofol at a dose of 100 µg/kg/min of IBW plus 0.6% of isoflurane was used. We adjusted the dose of these drugs using BIS monitoring (BISPECTRAL VISTA system, COVIDIEN, USA) and kept it in the range of 40 - 60. To provide analgesia and muscle relaxation, fentanyl 50 µg/h and atracurium 10 mg/30 min were repeated. An EDP-Neptune ventilator (MEDEK) was used for intraoperative ventilation. A tidal volume of 6 - 8 mL/kg was calculated for both modes of ventilation based on IBW. Then, patients were ventilated during VCV as follows: RR = 12/min, PEEP = 5 cm H2O, and FiO2 = 80% (80% O2 + 20% Air). The Respiratory Rate (RR) was adjusted every 5 min to optimum ET-CO2 (30 - 40 mmHg). In the PCV mode, patients were initially ventilated with P-Peak = 20 cmH2O, RR = 12/min, FiO2 = 80%, and PEEP = 5 cmH2O to reach the ideal TV (8 cc/kg). The airway pressure was adjusted at 2 cmH2O every 2 min until the maximum airway pressure of 40 cmH2O. The RR was adjusted to reach the optimal ET-CO2. The intra-abdominal pressure of CO2 in all patients was 15 cmH2O, which was gradually increased to 19 cm, if necessary. The formulas to calculate the IBW were: 50 + 0.91 [height (cm) - 152.4] for men and 45.5 + 0.91 [height (cm) - 152.4)] for women. All patients received intravenous crystalloid fluids according to the standard protocol, and the rate was adjusted to obtain an appropriate urinary output of 1 cc/kg/h.
2.2. Outcome Variables
The primary outcome of the study was peak inspiratory pressure (PIP) and dynamic compliance of the respiratory system, and secondary outcomes were expiratory TV, mean airway pressure, RR, oxygen saturation (SPO2), heart rate (HR), mean arterial pressure (MAP), and ET-CO2, all of which were recorded every 5 min during the intervention period. Also, at the end of 15 min, an arterial blood gas analysis was done. The results were finally recorded in a given form, and the amount of PaO2/FiO2 ratio, dead space volume, D (A-a) O2 gradient, and PaCO2-ETCO2 were calculated and recorded.
If PIP remained higher than 40 cmH2O after 10 min of abdominal insufflation despite the changes in the ventilator setting, it indicated ventilation failure by any of the methods used, and the patient were excluded from further study. With increasing RR up to 20/min in the presence of suitable TV and ET-CO2 still above 40, the ventilation mode was terminated, and the next mode was initiated.
2.3. Sample Size
According to previous studies, with standard VC ventilation in bariatric operations, the mean value for the primary outcome (PIP) was about 28 ± 3.8 cmH2O. Assuming a 20% decrease in this value by PC ventilation as significant, a power analysis was performed using an online calculator available from the University of British Columbia (Vancouver, BC, Canada) by setting alpha at 0.05 and beta at 80%. Regarding the crossover nature of the study, a group of 26 people was calculated (13 patients in each group). Finally, 40 people were studied (20 patients in each group) to increase the accuracy and study power.
2.4. Data Analysis
The obtained data were analyzed by SPSS statistical software version 25. Quantitative findings were reported as mean and standard deviation, and qualitative findings as frequency and percentage. For intra-group and between-group comparisons, appropriate statistical tests such as t test, paired t test, repeated measures, and chi-square were used depending on the type of variable (parametric and non-parametric and normal distribution). A P value of 0.05 was considered to be statistically significant.
3. Results
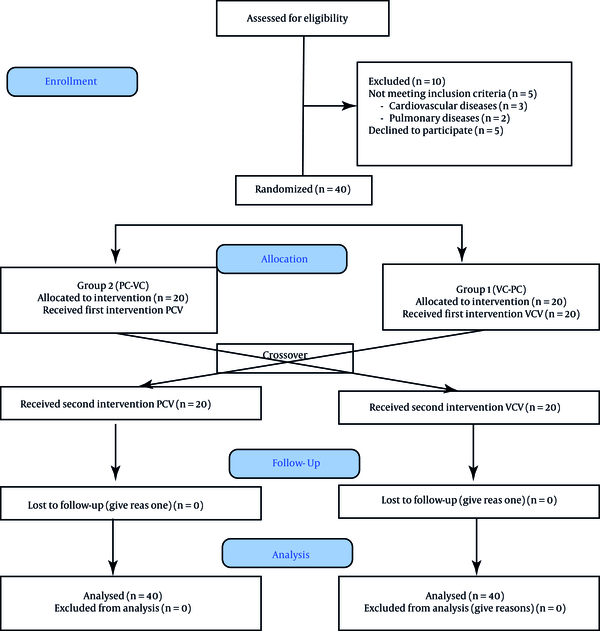
A total of 50 patients were screened for enrollment. After excluding 10 patients (Figure 1), 40 patients were assigned to the two study groups. Sleeve surgery was the most commonly offered surgery performed in 33 patients (82.5%). Demographic data are listed in Table 1. The mean intra-abdominal pressure (IAP) during surgery was 15.07 for PCV and 15.1 cmH2O for VCV, which were not found to be significantly different; also, the hemodynamic profile (MAP and HR) was comparable between the PCV and VCV groups (Table 2).
CONSORT flow chart of the study (PC, pressure control; VC, volume control; PCV, pressure-controlled ventilation; VCV, volume-controlled ventilation).
Demographic Characteristics of Patients Participating in the Study
| Variables | Number | Mean ± SD | Frequency |
|---|---|---|---|
| Age (y) | 40 | 35.13 ± 9.06 | |
| Gender (female/male) | 40 | - | 28/12 |
| Weight (kg) | 40 | 129.11 ± 23.54 | |
| Height (cm) | 40 | 164.85 ± 8.64 | |
| BMI (kg/m2) | 40 | 47.29 ± 5.74 | |
| IBW (kg) | 40 | 59.63 ± 9.21 | |
| Underlying disease (no/yes) | 40 | - | 18/22 |
| Type of surgery (sleeve/bypass) | 40 | - | 33/7 |
Comparison of Hemodynamic Variables and Intra-abdominal Pressure
| Variables | Case No. | VCV | PCV | P-Value |
|---|---|---|---|---|
| MAP (mmHg) | 40 | 94.19 ± 19.15 | 93.64 ± 20.5 | 0.08 |
| HR (beat/min) | 40 | 83.51 ± 11.7 | 84.48 ± 12.4 | 0.076 |
| RR (cycle/min) | 40 | 14.55 ± 2.82 | 14.84 ± 2.92 | 0.25 |
| IAP (cmH2O) | 40 | 15.1 | 15.07 | 0.09 |
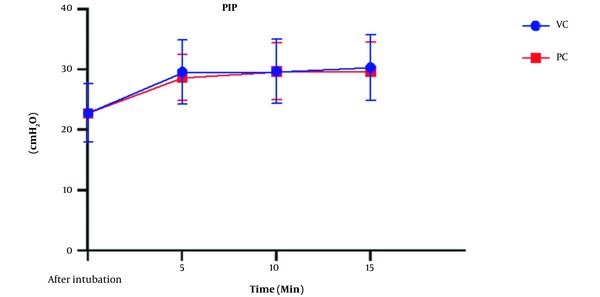
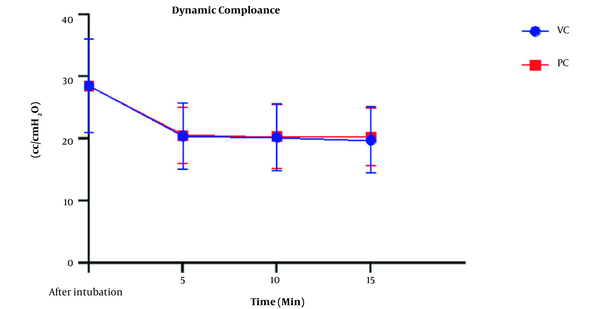
The peak airway pressure was compared, as shown in Figure 2. Airway pressure increased in both types of ventilation with insufflation of CO2 into the abdominal cavity. The ANOVA test showed a significant intra-group increase of this variable (P < 0.001); however, this difference was not significant between the VCV and PCV groups (P = 078). The mean dynamic compliance was 28.55 ± 7.54 cc/cmH2O before pneumoperitoneum but decreased to 20.15 ± 5.36 in the VCV group and 20.43 ± 4.77 in the PCV group after pneumoperitoneum. This decrease was significant in both groups compared to the baseline (P < 0.001), but there was no statistically significant difference between the two types of ventilation (P = 0.92) (Figure 3). Expiratory tidal volumes were 482.25 ± 67.2 and 483.02 ± 69.6 cc during VCV and PCV, which did not differ significantly (P = 0.812), almost equivalent to the ideal TV calculated for patients.
Comparison of peak inspiratory pressure between two modes of ventilation (PC, pressure control; VC, volume control).
Comparison of dynamic compliance changes in the study groups (PC, pressure control; VC, volume control).
Comparison of ET-CO2 levels using Mann-Whitney U and One-way ANOVA tests showed that with the onset of pneumoperitoneum, the mean of this variable increased in both types of ventilation. However, the rate of increase and mean ET-CO2 in the two groups were almost similar (P = 0.274). A comparison of the RR adjusted to maintain ET-CO2 in the ideal range also did not significantly differ between the two groups. However, a significant increase in the RR after pneumoperitoneum was needed in both groups (P < 0.001).
The comparison of oxygenation status and analysis of arterial gases are summarized in Table 3. No significant difference was found in the mean SPO2, PaO2, PaCO2, and pH between the two groups, where all patients had acceptable oxygenation during surgery. There were no differences in PaO2/FiO2 (P = 0.555) and P (A-a) O2 ratios (P = 0.585) between the two groups. The PaCO2-ETCO2 gradient was not significantly different between the two groups (P = 0.928).
| Ventilation Mode | Dead Space (mL) | D (a-ET) CO2 (mmHg) | P (A-a) O2 (mmHg) | PH | PaCO2 (mmHg) | PaO2/FiO2 | PaO2 (mmHg) |
|---|---|---|---|---|---|---|---|
| VCV | 83.95 ± 54.2 | 8.89 ± 6.21 | 253.67 ± 83.5 | 7.32 ± 0.06 | 46.32 ± 7.2 | 229.7 ± 116 | 183.8 ± 92.8 |
| PCV | 90.96 ± 49.85 | 8.76 ± 5.75 | 264.29 ± 79.34 | 7.32 ± 0.05 | 45.08 ± 6.9 | 214.3 ± 102 | 175.1 ± 80.5 |
| P-value | 0.573 | 0.928 | 0.585 | 1 | 0.462 | 0.555 | 0.678 |
4. Discussion
This study and our previous one (11), in line with multiple studies (5-7, 12-14), confirmed the undesirable effects of obesity and pneumoperitoneum on gas exchange and mechanical variables of respiration. Oxygenation indices such as PaO2/FiO2 ratio and P (A-a) O2 gradient indicate a right-to-left intrapulmonary shunt, possibly due to decreased pulmonary volumes and atelectasis. Nevertheless, corrective measures such as high FIO2, PEEP, head-up position, and intermittent recruitment maneuvers cannot completely prevent this complication. However, none of the patients suffered from hypoxemia of clinical significance. Furthermore, the dynamic and static compliance was significantly reduced compared to their normal values due to increased airway resistance and intra-abdominal pressure. These changes were present in both PCV and VCV modes.
Although several studies have determined the characteristics of optimal ventilation in these conditions, the desired results have not yet been obtained (14). High TV, which is traditionally common in VCV to maintain PaCO2 levels within the normal range during laparoscopic surgery, causes several complications such as increased airway pressure, volume trauma, and lung inflammation similar to that seen in acute respiratory distress syndrome (ARDS). Inflammatory mediators of the lungs are also released into the systemic circulation and cause inflammatory damage to distant organs (15). We used low tidal volume (8 cc/kg IBW) to tackle such issues in this study and maintained ET-CO2 at 30 to 40 mm Hg in both groups.
The results showed no significant difference between the two types of mechanical ventilation (VCV and PCV) in terms of oxygenation, ventilation, and mechanical variables of the respiratory system. In addition, the anesthesia profile and hemodynamic conditions did not differ significantly with the change of ventilation mode in the two groups. A review of the majority of previous studies comparing these two ventilation methods in patients with obesity confirms the present study results. In an earlier parallel study conducted in the same center by the authors of this article (11), similar results were obtained by VCV and PCV modes. In the mentioned study, both mechanical ventilation modes were over 95% successful in ventilating patients with obesity. The researchers concluded that the PCV, like VCV, could be used in intraoperative ventilation in patients with obesity. Although the PCV performed better in specific areas such as the PaO2/FiO2 ratio and the volume of respiratory dead space than the VCV, this difference was not statistically significant (11). The only difference between the present study and the previous one is the type of patient allocation to the research groups, parallel versus crossover allocation, to minimize the effect of individual differences of patients in the results.
In a crossover study by Hans et al. on 40 patients undergoing Roux-en-Y gastric bypass surgery, patients were classified into two groups after the first hour of surgery, including VC-PC and PC-VC. In both ventilation periods, patients' PaO2 and PaCO2 did not differ significantly. Therefore, they concluded that PCV mode did not improve gas exchange in patients with obesity compared to VCV, although the maximum inspiratory pressure in PCV ventilation was lower in PCV (16). Aldenkorrt et al. evaluated 13 studies (more than 500 patients) to compare ventilation with VCV and PCV modes and a combination of other interventions such as PEEP and recruitment maneuver in patients with obesity during surgery. They did not find any difference in PIP, oxygenation, and ventilation, but it further affirmed the positive effect of PEEP and recruitment maneuver on patients' oxygenation (17).
Furthermore, a study by Balick-Weber compared the respiratory and hemodynamic effects of ventilation with VCV and PCV modes during laparoscopic surgery, confirming the findings of our study (18). A survey by Movassagi et al. on patients undergoing laparoscopic cholecystectomy did not report a significant difference between the VCV and PCV modes, consistent with the present study (19). Finally, a meta-analysis published by Cousta Souza et al. reviewed 14 clinical trials with 574 patients. No evidence was found in favor of VCV and PCV ventilation, and both modes could be used in patients with obesity undergoing bariatric surgery without significant complications (20). De Baerdemaeker's study concluded that both VCV and PCV modes were equally suited for laparoscopy procedures in patients with morbid obesity, with CO2 elimination being more efficient when using VCV. These contradictory results may be associated with using a higher TV (10 cc/kg) (9).
In some previous studies, the most critical advantage of PCV ventilation has been the peak inspiratory pressure reduction and, consequently, the lower probability of barotrauma (21, 22). Dion et al. examined 20 patients undergoing laparoscopic bariatric surgery and used VCV, PCV, and pressure control-volume guaranteed (PCV-VG) modes; they found that PCV and PCV-VG caused less PIP compared to VCV (23). Our study did not show this difference between the two types of ventilation, which may be due to the use of low TV based on the IBW instead of the actual weight of patients in calculating TV.
Several studies inconsistent with the results of our research have concluded that PCV mode was capable of improving oxygenation in patients with obesity. For example, Gupta et al. showed that PCV was more effective than VCV concerning oxygenation in patients with obesity undergoing laparoscopic cholecystectomy (24). Cadi et al. reported a significant difference in oxygenation between PCV and VCV among patients with morbid obesity undergoing laparoscopic gastric banding surgery (25).
One of the limitations of this study was the lack of evaluation of patients with considerable cardiac and respiratory abnormalities, which could affect the clinical findings of the study. Therefore, these results cannot be generalized to patients with these problems.
4.1. Conclusions
Overall, this study showed no difference in the effectiveness of PCV and VCV for the ventilation of patients with obesity. However, our clinical experience has shown that it is easier to use and adjust the VCV mode because respiratory resistance and compliance during laparoscopic surgery are constantly changing following changes in intra-abdominal pressure. This issue causes a significant change in TV when applying the PCV mode, requiring frequent adjustment of PIP to ensure proper ventilation and prevent hypoventilation.
References
-
1.
Rashidi A, Mohammadpour-Ahranjani B, Vafa MR, Karandish M. Prevalence of obesity in Iran. Obes Rev. 2005;6(3):191-2. [PubMed ID: 16045632]. https://doi.org/10.1111/j.1467-789X.2005.00174.x.
-
2.
Esteghamati A, Khalilzadeh O, Mohammad K, Meysamie A, Rashidi A, Kamgar M, et al. Secular trends of obesity in Iran between 1999 and 2007: National Surveys of Risk Factors of Non-communicable Diseases. Metab Syndr Relat Disord. 2010;8(3):209-13. [PubMed ID: 20085488]. https://doi.org/10.1089/met.2009.0064.
-
3.
Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes (Lond). 2013;37(6):889-91. [PubMed ID: 22986681]. [PubMed Central ID: PMC3527647]. https://doi.org/10.1038/ijo.2012.159.
-
4.
Pelosi P, Croci M, Ravagnan I, Tredici S, Pedoto A, Lissoni A, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg. 1998;87(3):654-60. [PubMed ID: 9728848]. https://doi.org/10.1097/00000539-199809000-00031.
-
5.
Bamgbade OA, Rutter TW, Nafiu OO, Dorje P. Postoperative complications in obese and nonobese patients. World J Surg. 2007;31(3):556-61. [PubMed ID: 16957821]. https://doi.org/10.1007/s00268-006-0305-0.
-
6.
Jo YY, Kwak HJ. What is the proper ventilation strategy during laparoscopic surgery? Korean J Anesthesiol. 2017;70(6):596-600. [PubMed ID: 29225741]. [PubMed Central ID: PMC5716816]. https://doi.org/10.4097/kjae.2017.70.6.596.
-
7.
Campbell RS, Davis BR. Pressure-controlled versus volume-controlled ventilation: does it matter? Respir Care. 2002;47(4):416-26. [PubMed ID: 11929615].
-
8.
Dueck R. Alveolar recruitment versus hyperinflation: A balancing act. Curr Opin Anaesthesiol. 2006;19(6):650-4. [PubMed ID: 17093370]. https://doi.org/10.1097/ACO.0b013e328011015d.
-
9.
De Baerdemaeker LE, Van der Herten C, Gillardin JM, Pattyn P, Mortier EP, Szegedi LL. Comparison of volume-controlled and pressure-controlled ventilation during laparoscopic gastric banding in morbidly obese patients. Obes Surg. 2008;18(6):680-5. [PubMed ID: 18317856]. https://doi.org/10.1007/s11695-007-9376-8.
-
10.
Barash PG, Whitten CW. Clinical anesthesia. 5th ed. Philadelphia, USA: Lippincott Williams & Wilkins; 2006.
-
11.
Ghodraty MR, Pournajafian AR, Tavoosian SD, Khatibi A, Safari S, Motlagh SD, et al. A clinical trial of volume- versus pressure-controlled intraoperative ventilation during laparoscopic bariatric surgeries. Surg Obes Relat Dis. 2021;17(1):81-9. [PubMed ID: 33036946]. https://doi.org/10.1016/j.soard.2020.08.034.
-
12.
Sprung J, Whalley DG, Falcone T, Warner DO, Hubmayr RD, Hammel J. The impact of morbid obesity, pneumoperitoneum, and posture on respiratory system mechanics and oxygenation during laparoscopy. Anesth Analg. 2002;94(5):1345-50. [PubMed ID: 11973218]. https://doi.org/10.1097/00000539-200205000-00056.
-
13.
Morgan GE, Mikhail MS, Murray MJ, Larson CP. Anesthesia for patients with respiratory disease. Clinical Anesthesiology. New York, USA: Lange Medical Books; 2006. p. 511-24.
-
14.
Hu XY. Effective Ventilation Strategies for Obese Patients Undergoing Bariatric Surgery: A Literature Review. AANA J. 2016;84(1):35-45. [PubMed ID: 26939387].
-
15.
Koh SO. Mode of mechanical ventilation: volume controlled mode. Crit Care Clin. 2007;23(2):161-7. viii. [PubMed ID: 17368163]. https://doi.org/10.1016/j.ccc.2006.11.014.
-
16.
Hans GA, Pregaldien AA, Kaba A, Sottiaux TM, DeRoover A, Lamy ML, et al. Pressure-controlled ventilation does not improve gas exchange in morbidly obese patients undergoing abdominal surgery. Obes Surg. 2008;18(1):71-6. [PubMed ID: 18080725]. https://doi.org/10.1007/s11695-007-9300-2.
-
17.
Aldenkortt M, Lysakowski C, Elia N, Brochard L, Tramer MR. Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br J Anaesth. 2012;109(4):493-502. [PubMed ID: 22976857]. https://doi.org/10.1093/bja/aes338.
-
18.
Balick-Weber CC, Nicolas P, Hedreville-Montout M, Blanchet P, Stephan F. Respiratory and haemodynamic effects of volume-controlled vs pressure-controlled ventilation during laparoscopy: a cross-over study with echocardiographic assessment. Br J Anaesth. 2007;99(3):429-35. [PubMed ID: 17626027]. https://doi.org/10.1093/bja/aem166.
-
19.
Movassagi R, Montazer M, Mahmoodpoor A, Fattahi V, Iranpour A, Sanaie S. Comparison of pressure vs. volume controlled ventilation on oxygenation parameters of obese patients undergoing laparoscopic cholecystectomy. Pak J Med Sci. 2017;33(5):1117-22. [PubMed ID: 29142549]. [PubMed Central ID: PMC5673718]. https://doi.org/10.12669/pjms.335.13316.
-
20.
Costa Souza GM, Santos GM, Zimpel SA, Melnik T. Intraoperative ventilation strategies for obese patients undergoing bariatric surgery: systematic review and meta-analysis. BMC Anesthesiol. 2020;20(1):36. [PubMed ID: 32019491]. [PubMed Central ID: PMC7001296]. https://doi.org/10.1186/s12871-020-0936-y.
-
21.
Ozyurt E, Kavakli AS, Ozturk NK. [Comparison of volume-controlled and pressure-controlled ventilation on respiratory mechanics in laparoscopic bariatric surgery: randomized clinical trial]. Braz J Anesthesiol. 2019;69(6):546-52. [PubMed ID: 31806235]. https://doi.org/10.1016/j.bjan.2019.08.005.
-
22.
Shah U, Wong J, Wong DT, Chung F. Preoxygenation and intraoperative ventilation strategies in obese patients: a comprehensive review. Curr Opin Anaesthesiol. 2016;29(1):109-18. [PubMed ID: 26545146]. https://doi.org/10.1097/ACO.0000000000000267.
-
23.
Dion JM, McKee C, Tobias JD, Sohner P, Herz D, Teich S, et al. Ventilation during laparoscopic-assisted bariatric surgery: volume-controlled, pressure-controlled or volume-guaranteed pressure-regulated modes. Int J Clin Exp Med. 2014;7(8):2242-7. [PubMed ID: 25232415]. [PubMed Central ID: PMC4161575].
-
24.
Gupta SD, Kundu SB, Ghose T, Maji S, Mitra K, Mukherjee M, et al. A comparison between volume-controlled ventilation and pressure-controlled ventilation in providing better oxygenation in obese patients undergoing laparoscopic cholecystectomy. Indian J Anaesth. 2012;56(3):276-82. [PubMed ID: 22923828]. [PubMed Central ID: PMC3425289]. https://doi.org/10.4103/0019-5049.98777.
-
25.
Cadi P, Guenoun T, Journois D, Chevallier JM, Diehl JL, Safran D. Pressure-controlled ventilation improves oxygenation during laparoscopic obesity surgery compared with volume-controlled ventilation. Br J Anaesth. 2008;100(5):709-16. [PubMed ID: 18407943]. https://doi.org/10.1093/bja/aen067.