Abstract
Background:
Lifestyle modification has a significant role in chronic daily headache (CDH) management. Participatory action research (PAR) can play an important role in managing chronic medical conditions. However, it has been scarcely used in CDH management.Objectives:
This study aimed to empower patients with CDH to modify their lifestyle in order to reduce both their headache and related psychiatric co-morbidities in a multidisciplinary headache clinic at Baqiyatallah hospital, Tehran, IR Iran.Methods:
In the PAR plan, 37 patients (27 females) diagnosed with CDH were selected using purposeful sampling. Along with face-to-face group sessions, all available communication means such as phone calls, emails, short message system (SMS), and social media (Telegram) were used to facilitate the process. Questionnaires of health promotion lifestyle profile (HPLPІІ), visual analog scale (VAS), and depression-anxiety-stress scale (DASS21) were used to collect data. The data were analyzed using SPSS software.Results:
Mean age of the patients was 38.33 (± 9.7) years. Both “general pain” and “the worst imaginable pain” reduced (mean of reduction: 2.56 ± 2.7 and 2.3 ± 2.9, respectively, P < 0.001). > 50% of pain reduction occurred in “the worst imaginable pain" category (-1.45 ± 2.02, P < 0.001) and mean VAS score reduced to 5.20 (± 2.3) compared to the start of the study (7.50 ± 1.9, P < 0.001). Mean DASS-21 score also reduced significantly for depression (P < 0.016), anxiety (P < 0.026), and stress (P < 0.008). HPLPІІ score significantly improved (118.17 ± 14.8 vs. 160.83 ± 16.4, P < 0.001) and the highest increase was seen in the subscale of "stress management" (17.73 ± 2.8 vs. 25.53 ± 3.9, P < 0.001).Conclusions:
The empowering PAR plan combined with new communication tools helped the CDH patients better handle their lifestyle, reduce their headache, and lower their symptoms. Further studies with better use of currently available communication tools and social media are recommended for action research to be more applicable.Keywords
Headache Disorder Patient Participation Life Style Psychiatry Communication
1. Introduction
Managing chronic daily headache (CDH) relies more on the modification of risk factors to make a tangible change in one’s lifestyle instead of paying attention to poorly understood pathophysiology of such a pain (1-4). Acceptance of pain by the patients and their effort to actively participate in empowering programs to manage their headache mainly by themselves may be the key point to achieve the goal (5-7). Based on reviewing the past medical histories (PMH) of patients referring for chronic primary headache (CDH) from 2010 to 2014 and during their monthly visits at the multidisciplinary headache clinic located at a referral hospital in Tehran, the capital of IR Iran, they were being advised to make a change in their lifestyle as a main part of CDH management. We were frequently hearing the response from the patients that “I want to but I can’t”. Previous studies have reported participatory action research (PAR) improving chronic medical conditions as better cope with chronic pain (8), enhancing life in patients with multiple sclerosis (9) and better live with diabetes (10). However, few studies have reported using PAR in patients with chronic daily headache (11, 12). Additionally, traffic-related provoking factors in large cities of the world like the cities in our country (13, 14) impose some more limitations on the patients to participate in several face-to-face sessions that are crucial in a PAR plan. Hence, using the country-wide available ways for easy communication may play an effective role in this setting. Thus, in this study, we employed PAR with the use of available and legally permitted means of communication such as E-mail, SMS (short message service), phone calls (Mobile) and social media (Telegram) along with formal meeting sessions to manage CDH patients through modifying their lifestyle.
2. Methods
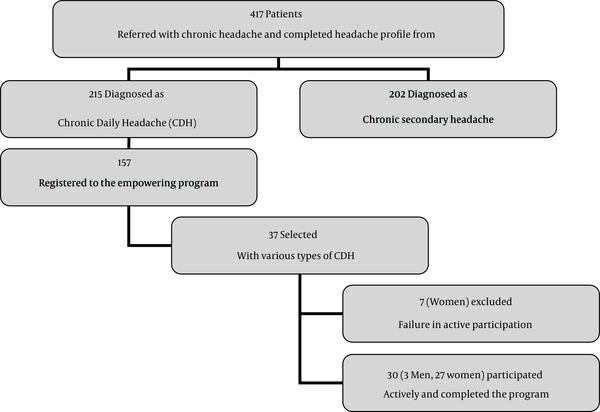
One-hundred and fifty-five out of 215 patients with CDH amongst 417 total patients who referred for chronic headache from all over the country were voluntarily enrolled in the study. Considering the participants’ convenience, 37 inhabitants (27 females) from Tehran (the capital) and Karaj (about 45 kilometers away from Tehran) were selected for the study. Patients suffering from different types of CDH were selected. Written informed consent was obtained from the participants for study enrollment. Inclusion criteria included: having diploma or higher education level, no major psychiatric co-morbidities that require hospitalization or emergency intervention, experiencing headache for more than 15 days a month for at least one year and being eager to participate actively in the group sessions. Seven women were excluded due to failure of active participation and refusal to return post-test (Figure 1).
The Study Flowchart and Participant Selection
The group was established at the multidisciplinary department of headache in early 2014 at Baqiyatallah Hospital located in Tehran. The group comprised a psychiatrist (A.T.), an expert in pain (M.S.), a nurse educator (A.R.), a PhD student in pain research and management (F.F.) along with 30 diverse CDH cases (15 with migraine, 1 with Mixed (tension-type and migraine), 1 with tension-type, 1 with indomethacine-sensitive, and 12 with undifferentiated CDH). Materials of the program were based on the recommendations of Gaul et al. (2011) and Rasmussen (1993) (15, 16). The group sessions were held at a 70-seat conference hall. The patients were asked to fill out questionnaires of visual analog scale (VAS), depression-anxiety-stress scale (DASS21), and health promotion lifestyle profile (HPLPІІ) before and after the lifestyle modification program. VAS is an 11-point tool that rates the severity of pain from 0 (no pain) to 10 (the worst imaginable pain) (17). DASS21 is a 21-item questionnaire used to assess psychiatric co-morbidities including depression, anxiety, and stress with 7 questions for each subscale (18). HPLPΙΙ is a self-reporting 52-item questionnaire that evaluates one’s lifestyle in 6 dimensions viz. spiritual growth, interpersonal relations, nutrition, physical activity, health responsibility, and stress management (19). Persian version of the questionnaires have been previously used and reported as valid and reliable tools for such studies from IR Iran (20-22). We used SPSS software applying Kolmogorov-Smirnov (K-S) test to analyze normality and K-S > 0.05 was assumed as normal distribution. We then performed paired t-test and Wilcoxon test to analyze data collected by the questionnaires and/or obtained from medical interviews. The entire process of the PAR study is shown in Table 1 based on Lewin’s (1947) model (23). The work was approved by the committee of research council and medical ethics at Baqiyatallah University of Medical Sciences (Code 7106).
| Lewin’s Model of Action Research | Study Steps |
|---|---|
| Stage 1: Problem Statement | Patients with CDH suffering from headache and unable to modify their unhealthy lifestyle |
| Stage 2: Data Collection | By reviewing their medical records, routine interviews and/or during their medical visits from 2010-2014 |
| Stage 3: Analysis and Feedback | A 7-step PAR plan was recommended by the expert panel based on the results of Patients PMHs, visits, and interviews, and their feedback was obtained |
| Stage 4: Action Planning | Participants agreed a 4-step PAR plan including: diet, exercising, stress reduction, and trigger management |
| Stage 5: Taking Action | Pre-test, implementing the plan (from Jun to Dec 2014) |
| Stage 6: Evaluation and Follow-up | Post-test (evaluation), and follow-up from Jan to Sep 2015 |
2.1. Stage 1 - 4: Problem Statements, Data Collection, Analysis and Feedback (Based on Patients PMHs and Interviews) and Action Planning
A 7-session action plan outlining: chronic daily headache: causes and management, stress reduction and relaxation training, recommended physical activities, nutrition and diet, environmental factors and healthy sleeping schedule based on the participants’ PMHs, interviews and their willingness to modify their lifestyle were presented by the expert panel. Taking the participants’ comments, the panel agreed to give them an opportunity (of one week) to think and read about the recommended plan and adjust their personal schedule before finalizing the plan. The final empowering program according to the patients’ comments was shortened to only four sessions to be held in four consecutive weeks outlining: 1. Diet & nutritional awareness, 2. Physical activity, 3. Stress management, and 4. Identifying environmental trigger factors based on the patients’ preferences (Table 2).
The Final PAR Plan Based on the Participants’ Willingness to Modify Their Lifestyle
| Session | Outline | Time, mina | Subtitles |
|---|---|---|---|
| 1 | Diet and nutritional awarness | 120 | Recommended diet in headaches, provoking nutritional triggers, old and fermented foods, traditional and cultural considerations |
| 2 | Physical activity | 120 | Type, duration and level of exercise; recommended activities, favorable heart beat |
| 3 | Stress reduction and relaxation training | 120 | Interaction between stress and CDH, how to manage stress, general considerations, PMR, diaphragmatic breathing, MBSR, ACT, passive muscle relaxation |
| 4 | Environmental factors | 120 | Traffic and air pollution, sounds, calls, crowdedness, altered family structure |
Each participant was requested to select a tele-communication route other than cell phone such as email, SMS, and/or social media (Telegram) according to their preference to send and/or receive the program materials and comments to/from them and the expert panel. They were also reassured to receive professional consultation through phone calls whenever they required during the period of action plan.
2.2. Stage 5: Taking Action (Implementation)
Each item of diet and nutritional awareness and physical activity in CDH management (4, 24-26) was presented for 2 hours during two consecutive weeks (Jun 2014). The patients requested more time (at least one month) to practice before evaluating the effectiveness of the program. Although that was discordant to both the preliminary and the final PAR plan, the expert panel accepted this change considering the flexibility of PAR methodology (27). Four frequently-used stress reduction techniques including: progressive muscle relaxation (PMR) (28), guided imagery (29), diaphragmatic breathing (30), and passive muscle relaxation (31) were presented in session 3 in August 2014. Each technique was presented for 30 minutes and practiced by the participants. Then, they were asked to practice the techniques individually at their home and choose the one that better relieves their stress. Most participants were familiar with the modalities but none had practiced the techniques effectively before.
Session 4 was supposed to be held in September. However, the patients had to spend the month in outdoor trips with their families and had to prepare their children to start school after summer vacations. Thereby, they confronted more crowdedness and traffic for commuting from their homes to the multidisciplinary clinic. Thus, the patients requested to have the last session by email or telegram instead of taking part in face-to-face group sessions. The teaching materials and requested information by the patients for the last session were emailed and shared with them through social media. For all the messages, the expert panel received delivery note. The last trimester of 2014 was the time allocated for the participants to practice the recommended guidelines, techniques, and precautions. The participants were free to ask any question anytime during 24 hours and they got professional support within maximum two hours delay.
To provide a permanent and accessible source of the program, an account of domestic SMS center (www.sms.ir) was also created for all the patients. This facility helped transmit long text messages and provide a convenient opportunity for the patients to have brief steps of the plan in their own mobile phones. The use of Telegram provided an easy way to share related animations, video clips, and other messages between the expert panel and the patients.
We received more positive feedbacks implying successful headache management just a few weeks after the last session (transcription 1).
2.3. Transcription 1
Now I feel better so I know how to manage my headache and reduce things that may result in headache. My sleep has gotten better and I may take a pill to sleep only 1 - 2 days a week (while I used to take them daily). I exercise with my friends in headache-free times. Now, I know which foods and conditions may leave me with a headache. I realized that nobody can relieve my pain other than me. My pain score generally has reduced to 2 or 3 maybe…
The participants were requested to fill out the questionnaires of DASS21, HPLPІІ and VAS after about nine months as post-test.
3. Results
3.1. Stage 6: Evaluation and Follow-Up
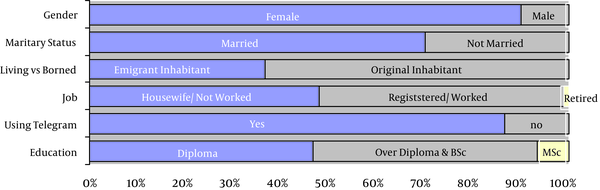
Seven female patients failed to participate actively in the sessions or did not return their post-test questionnaires and hence, they were excluded from the study. Mean age of the rest of the 30 participants (3 males and 27 females) was 38.33 (± 9.7) which ranged from 24 to 57 years. Other demographic characteristics are shown in Figure 2.
Demographic Characteristics of the Patticipants with CDH (n = 30)
Mean intensity of headache measured by VAS reduced to 5.20 (± 2.3) compared to the start of the study (7.50 ± 1.9, P < 0.001). Using paired t-test, both “general pain” and “the worst imaginable pain” reduced significantly (mean reduction of 2.56 ± 2.7 and 2.3 ± 2.9, respectively, P < 0.001). More than 50% of pain reduction was seen in "the worst imaginable pain” category (-1.45 ± 2.02, P < 0.001), as shown in Table 3.
| Headache Severity | Mean Reduction Pre- and Post-Intervention (n = 30) | t | P Value | > 50% Reduction | P Value |
|---|---|---|---|---|---|
| Right now (these days) | 1.9 ± 3.2 | 3.21 | 0.003 | 0.68 ± 2.44 | 0.137 |
| The worst imaginable pain | 2.3 ± 2.9 | 4.29 | 0.001 | -1.5 ± 2.02 | 0.001 |
| General head pain | 2.56 ± 2.6 | 5.2 | 0.001 | 0.35 ± 1.8 | 0.295 |
By the application of Wilcoxon test, the mean score of DASS-21 after the intervention significantly reduced in the all subscales of depression (P < 0.016), anxiety (P < 0.026), and stress (P < 0.008) (Table 4).
| DASS21 Subscales | Mean Score Negative/Positive (n = 30) | z | P Value |
|---|---|---|---|
| Depression | 13.11 / 6.79 | -2.41 | 0.016 |
| Anxiety | 12.53 / 12.42 | -2.23 | 0.026 |
| Stress | 13.33 / 10.0 | -2.67 | 0.008 |
Total score of “health promotion” after the plan, measured by HPLPІІ, showed a significant improvement (160.83 ± 16.4 vs. 118.17 ± 14.8, P < 0.001) compared to the baseline data. The most significant progression was seen in the subscale of “stress management” (mean: 25.53 ± 3.9 vs. 17.73 ± 2.8, P < 0.001). Details of the improvement in other subscales are presented in Table 5.
| HPLPІІ Subscales | Pre- and Post-Interventionb (n = 30) | t | P Value |
|---|---|---|---|
| Health Responsibility | -10.10 ± 4.4c | -12.65 | 0.001 |
| Physical Activity | -6.66 ± 6.3c | -5.83 | 0.001 |
| Nutrition | -3.80 ± 3.9c | -5.34 | 0.001 |
| Spiritual Growth | -6.66 ± 4.9c | -7.37 | 0.001 |
| Interpersonal Relationship | -7.40 ± 3.7c | -10.9 | 0.001 |
| Stress Management | -7.80 ± 4.1d | -10.47 | 0.001 |
| Total HPLPІІ | -42.66 ± 17.7c | -13.2 | 0.001 |
4. Discussion
In this study, we used PAR to manage patients with CDH. Overall, our results showed that in patients with CDH, a significant improvement occurs for various symptoms by the application of PAR. We believe that lifestyle modification, which is the cornerstone of PAR, plays an important role in the management of such patients. However, we faced several problems and limitations during this study.
Gathering patients with chronic condition and encouraging them to take part in several face-to-face group sessions in the crowded capital of Tehran was a particularly difficult task. Our preliminary PAR plan was shortened to final four steps, and the last session was also modified to be held without face-to-face interaction of participants. Interval of the sessions was also modified according to the participants’ requests. Various supportive modalities were added that helped us carry out sessions with better quality. Using country-wide communication tools and social media (Telegram) made the PAR plan more flexible. Our results were similar to those reported by Barton et al. (2014) indicating better patients’ outcome in a multidisciplinary headache management plan (32). PAR method is a new research paradigm in practice that provides better opportunity and more flexibility and open-handedness in order to empower patients to solve their problems on their own (33). We carried out only one cycle of PAR plan that lasted for 9 months. However, the cycle could be repeated to show more significant changes in the patients’ lifestyle as Maindal et al. (2014) reported a flexible pre-diabetes lifestyle modification through a 2-cycle action research on 64 patients, 8 GPs, and 10 nurses during one year that resulted in reductions in the patients’ BMI and HbA1c (34). Seemingly, Bell et al. carried out a 4-cycle action research on 614 hip-fracture inpatients and 30 clinicians, reporting the approach was more effective on patients and facilitated practical solutions such as nutrition care (35).
Our results showed more than 50% reduction in headache severity in "the worst imaginable pain" category which is similar to the results of Smith et al. (2010) reporting > 50% reduction of headache frequency in 46% of patients with chronic headache who participated in a migraine education program. The study also reported the quality of life improvement in the subscales of “worry about their headache”, “self-efficacy” and “satisfaction with headache care” in addition to the highest improvement occurred in the item of “more worry about their headache” (36).
Our results also showed the PAR plan made a significant reduction in anxiety, depression, and stress in patients with CDH. These results are similar to those of Tasdemir et al. (2011) that reported six weekly nursing home visits plus another visit 1 month later through action research significantly reduced anxiety and depression in patients with Alzheimer’s disease in Turkey (37). It seems that improving aerobic physical activity in our study has rendered better control of depression, anxiety, and stress according to the findings of Salmon (2001) who offered exercise training on anxiety, depression, and stress management as “a vehicle for nonspecific therapeutic social and psychological processes” (38).
Effective ways of lifestyle modification such as proper nutrition, modified physical activity, stress management and management of environmental triggers play significant roles in the management of several chronic disorders (26, 39). Patients with CDH are more susceptible to pain-evoking stimuli; they are less concerned about their diet, more sensitive to the environmental triggers, and have relatively simple life-styles (40, 41). In this study, the use of PAR was an effort on our part to motivate these patients to be able to choose the best way to change their personal lifestyles and adopt better. We honestly made an effort to stand by their sides to be easily accessible consultants and reliable healthcare professionals and provide them with reassurance. In this regard, Belam et al. (2005) reported that “handling the best” was the central metaphor of chronic headache management in patients suffering migraine (12). Furthermore, engaging and supporting participants and encouraging them to develop better solutions for their health problems may have significant effects on the relief of various symptoms (42).
We used all of the legally permissible communication means such as social media (telegram), email, phone calls, mobile calls, SMS, web-site, and open-medical visits to diminish any obstacle to the guidance and support of the patients. We think that this atmosphere made a positive sense of unity and integration that facilitated participation of patients and their communication with the expert panel. This was similar to the work by Angelin (2015) which reported that service user participation and patient empowerment resulted in better “collaboration between researchers, social work educators, and service users” (43). In this regard, Gallegos et al. (2014) also reported that sending a text message weekly can improve mothers’ breast feeding and their perception of coping and support provision (44). Despite the lack of time, funding, and expert trainers that are reported as restrictions of PAR (45), employing various available communication means to empower participants can certainly diminish expenditure and the high burden of chronic conditions by decreasing the need for direct medical visits and face-to-face para-clinical modalities. Generalization of the results needs some considerations in terms of available cultural sources. We were not legally eligible to use some of the social media (such as WhatsApp and Facebook) according to the country’s legal regulations since 2014.
4.1. Conclusions
Applying PAR plan to empower patients with CDH in order to modify their lifestyle resulted in better HPLP score, lower intensity of headache, and significantly less DASS score. Using the new communication technologies provided patients with better access to professional support. More research is recommended to investigate the possible application of PAR in other chronic conditions.
Acknowledgements
References
-
1.
Albers L, Ziebarth S, von Kries R. [Modifiable risk factors for primary headache. A systematic review]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2014;57(8):952-60. [PubMed ID: 25002234]. https://doi.org/10.1007/s00103-014-1997-1.
-
2.
Benoliel R, Eliav E. Primary headache disorders. Dent Clin North Am. 2013;57(3):513-39. [PubMed ID: 23809307]. https://doi.org/10.1016/j.cden.2013.04.005.
-
3.
Hale N, Paauw DS. Diagnosis and treatment of headache in the ambulatory care setting: a review of classic presentations and new considerations in diagnosis and management. Med Clin North Am. 2014;98(3):505-27. [PubMed ID: 24758958]. https://doi.org/10.1016/j.mcna.2014.01.006.
-
4.
Moschiano F, D'Amico D, Ramusino MC, Micieli G. The role of diet and lifestyle in adolescents with headache: a review. Neurol Sci. 2013;34 Suppl 1:S187-90. [PubMed ID: 23695077]. https://doi.org/10.1007/s10072-013-1414-9.
-
5.
Matchar DB, Harpole L, Samsa GP, Jurgelski A, Lipton RB, Silberstein SD, et al. The headache management trial: a randomized study of coordinated care. Headache. 2008;48(9):1294-310. [PubMed ID: 18547268]. https://doi.org/10.1111/j.1526-4610.2007.01148.x.
-
6.
Fradgley EA, Paul CL, Bryant J, Roos IA, Henskens FA, Paul DJ. Consumer participation in quality improvements for chronic disease care: development and evaluation of an interactive patient-centered survey to identify preferred service initiatives. J Med Internet Res. 2014;16(12). ee292. [PubMed ID: 25532217]. https://doi.org/10.2196/jmir.3545.
-
7.
Vahdat S, Hamzehgardeshi L, Hessam S, Hamzehgardeshi Z. Patient involvement in health care decision making: a review. Iran Red Crescent Med J. 2014;16(1). ee12454. [PubMed ID: 24719703]. https://doi.org/10.5812/ircmj.12454.
-
8.
Baker TA, Wang CC. Photovoice: use of a participatory action research method to explore the chronic pain experience in older adults. Qual Health Res. 2006;16(10):1405-13. [PubMed ID: 17079801]. https://doi.org/10.1177/1049732306294118.
-
9.
Koch T, Selim P, Kralik D. Enhancing lives through the development of a community-based participatory action research programme. J Clin Nurs. 2002;11(1):109-17. [PubMed ID: 11845746].
-
10.
Adili F, Higgins I, Koch T. Older women and chronic illness: Transitioning and learning to live with diabetes. Act Res. 2013;11(2):142-56.
-
11.
Seifert LS. Self-regulation in disability: Migraine management as action research. Act Res. 2012;10(4):336-55.
-
12.
Belam J, Harris G, Kernick D, Kline F, Lindley K, McWatt J, et al. A qualitative study of migraine involving patient researchers. Br J Gen Pract. 2005;55(511):87-93. [PubMed ID: 15720928].
-
13.
Tabraiz S, Ahmad S, Shehzadi I, Asif MB. Study of physio-psychological effects on traffic wardens due to traffic noise pollution; exposure-effect relation. J Environ Health Sci Eng. 2015;13:30. [PubMed ID: 25988003]. https://doi.org/10.1186/s40201-015-0187-x.
-
14.
Saeedi M, Li LY, Salmanzadeh M. Heavy metals and polycyclic aromatic hydrocarbons: pollution and ecological risk assessment in street dust of Tehran. J Hazard Mater. 2012;227-228:9-17. [PubMed ID: 22647232]. https://doi.org/10.1016/j.jhazmat.2012.04.047.
-
15.
Gaul C, van Doorn C, Webering N, Dlugaj M, Katsarava Z, Diener HC, et al. Clinical outcome of a headache-specific multidisciplinary treatment program and adherence to treatment recommendations in a tertiary headache center: an observational study. J Headache Pain. 2011;12(4):475-83. [PubMed ID: 21544647]. https://doi.org/10.1007/s10194-011-0348-y.
-
16.
Rasmussen BK. Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain. 1993;53(1):65-72. [PubMed ID: 8316392].
-
17.
Aicher B, Peil H, Peil B, Diener HC. Pain measurement: Visual Analogue Scale (VAS) and Verbal Rating Scale (VRS) in clinical trials with OTC analgesics in headache. Cephalalgia. 2012;32(3):185-97.
-
18.
Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44(Pt 2):227-39. [PubMed ID: 16004657]. https://doi.org/10.1348/014466505X29657.
-
19.
Walker SN, Hill-Polerecky DM. Psychometric evaluation of the health-promoting lifestyle profile II. Nebraska: University of Nebraska Medical Cente; 1996.
-
20.
Rakhshani T, Shojaiezadeh D, Bagheri Lankarani K, Rakhshani F, Kaveh MH, Zare N. The association of health-promoting lifestyle with quality of life among the Iranian elderly. Iran Red Crescent Med J. 2014;16(9).
-
21.
Jafarian S, Gorouhi F, Salimi S, Lotfi J. Low-dose gabapentin in treatment of high-altitude headache. Cephalalgia. 2007;27(11):1274-7. [PubMed ID: 17692105]. https://doi.org/10.1111/j.1468-2982.2007.01387.x.
-
22.
Asghari A, Saed F, Dibajnia P. Psychometric properties of the Depression Anxiety Stress Scales-21 (DASS-21) in a non-clinical Iranian sample. Int J Psychol. 2008;2(2):82-102.
-
23.
Tomal DR. Action research for educators. Rowman & Littlefield Publishers; 2010.
-
24.
Kafeshani O, Sarrafzadegan N, Nouri F, Mohammadifard N. Major dietary patterns in Iranian adolescents: Isfahan Healthy Heart Program, Iran. ARYA Atheroscler. 2015;11(Suppl 1):61-8. [PubMed ID: 26261451].
-
25.
Finkel AG, Yerry JA, Mann JD. Dietary considerations in migraine management: does a consistent diet improve migraine? Curr Pain Headache Rep. 2013;17(11):373. [PubMed ID: 24068338]. https://doi.org/10.1007/s11916-013-0373-4.
-
26.
Minich DM, Bland JS. Personalized lifestyle medicine: relevance for nutrition and lifestyle recommendations. ScientificWorldJournal. 2013;2013:129841. [PubMed ID: 23878520]. https://doi.org/10.1155/2013/129841.
-
27.
Conder J, Milner P, Mirfin-Veitch B. Reflections on a participatory project: the rewards and challenges for the lead researchers. J Intellect Dev Disabil. 2011;36(1):39-48. [PubMed ID: 21309660]. https://doi.org/10.3109/13668250.2010.548753.
-
28.
McCallie MS, Blum CM, Hood CJ. Progressive muscle relaxation. J Human Behav Soc Environ. 2006;13(3):51-66.
-
29.
Ilacqua GE. Migraine headaches: coping efficacy of guided imagery training. Headache. 1994;34(2):99-102. [PubMed ID: 8163375].
-
30.
Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984.
-
31.
Asai K, Hufschmidt HJ, Schaltenbrand G. The passive muscle relaxation in parkinsonism: myographic studies of the pathophysiology of the rigor. J Nerv Ment Dis. 1960;130:449-55. [PubMed ID: 13794630].
-
32.
Barton PM, Schultz GR, Jarrell JF, Becker WJ. A flexible format interdisciplinary treatment and rehabilitation program for chronic daily headache: patient clinical features, resource utilization and outcomes. Headache. 2014;54(8):1320-36. [PubMed ID: 24862836]. https://doi.org/10.1111/head.12376.
-
33.
Meyer JE. New paradigm research in practice: the trials and tribulations of action research. J Adv Nurs. 1993;18(7):1066-72. [PubMed ID: 8370895].
-
34.
Maindal HT, Bonde A, Aagaard-Hansen J. Action research led to a feasible lifestyle intervention in general practice for people with prediabetes. Prim Care Diabetes. 2014;8(1):23-9. [PubMed ID: 24361372]. https://doi.org/10.1016/j.pcd.2013.11.007.
-
35.
Bell JJ, Rossi T, Bauer JD, Capra S. Developing and evaluating interventions that are applicable and relevant to inpatients and those who care for them; a multiphase, pragmatic action research approach. BMC Med Res Methodol. 2014;14:98. [PubMed ID: 25135226]. https://doi.org/10.1186/1471-2288-14-98.
-
36.
Smith TR, Nicholson RA, Banks JW. Migraine education improves quality of life in a primary care setting. Headache. 2010;50(4):600-12. [PubMed ID: 20148982]. https://doi.org/10.1111/j.1526-4610.2010.01618.x.
-
37.
Tasdemir G, Oz F. Home follow-up of early- and mid-stage Alzheimer's patients. J Psychiatr Ment Health Nurs. 2011;18(9):767-75. [PubMed ID: 21985679]. https://doi.org/10.1111/j.1365-2850.2011.01724.x.
-
38.
Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21(1):33-61. [PubMed ID: 11148895].
-
39.
Sarris J, Nishi D, Xiang YT, Su KP, Bannatyne A, Oliver G, et al. Implementation of psychiatric-focused lifestyle medicine programs in Asia. Asia Pac Psychiatry. 2015;7(4):345-54. [PubMed ID: 26403310]. https://doi.org/10.1111/appy.12212.
-
40.
Lund N, Westergaard ML, Barloese M, Glumer C, Jensen RH. Epidemiology of concurrent headache and sleep problems in Denmark. Cephalalgia. 2014;34(10):833-45. [PubMed ID: 25078716]. https://doi.org/10.1177/0333102414543332.
-
41.
Winter AC, Hoffmann W, Meisinger C, Evers S, Vennemann M, Pfaffenrath V, et al. Association between lifestyle factors and headache. J Headache Pain. 2011;12(2):147-55. [PubMed ID: 21222138]. https://doi.org/10.1007/s10194-010-0286-0.
-
42.
White MA, Verhoef MJ. Toward a patient-centered approach: incorporating principles of participatory action research into clinical studies. Integr Cancer Ther. 2005;4(1):21-4. [PubMed ID: 15695474]. https://doi.org/10.1177/1534735404273727.
-
43.
Angelin A. Service user integration into social work education: lessons learned from nordic participatory action projects. J Evid Inf Soc Work. 2015;12(1):124-38. [PubMed ID: 25662088].
-
44.
Gallegos D, Russell-Bennett R, Previte J, Parkinson J. Can a text message a week improve breastfeeding? BMC Pregnancy Childbirth. 2014;14:374. [PubMed ID: 25369808]. https://doi.org/10.1186/s12884-014-0374-2.
-
45.
Macaulay AC. Promoting participatory research by family physicians. Ann Fam Med. 2007;5(6):557-60. [PubMed ID: 18025494]. https://doi.org/10.1370/afm.755.