Abstract
Background:
The use of Propofol often results in pain upon injection, which is sometimes very distressing for patients. Many patients report some degree of pain or discomfort on injection with propofol. Injection-induced pain during induction of anesthesia can result in patient's discomfort.Objectives:
This study was performed to evaluate the effects of nitroglycerine on pain severity in patients undergoing propofol injection.Patients and Methods:
In this double-blind randomized clinical trial, 100 patients with ASA class I and II undergoing anesthesia with propofol injection were selected for the study from 2012 to 2013 in Imam Reza training hospital. Patients were randomly assigned to case and control groups and received either 20 μg of nitroglycerine or normal saline as placebo. The severity of injection pain was assessed using a four-point scale. An anesthesiologist observed hemodynamic and local adverse effects.Results:
The pain severity in nitroglycerine group was significantly lower compared with the placebo group (P < 0.0001). Moreover, the local adverse reactions were observed only in three patients in the placebo group while no patient in the drug group experienced adverse effects (P = 0.242). The systolic blood pressure showed no significant difference between two groups before and after the induction of anesthesia but the diastolic blood pressure and the heart rate was significantly different between study groups.Conclusions:
Nitroglycerine may be a safe and effective adjuvant therapeutic for pain reduction in patients under propofol injection. Hence, its use for reduction of propofol injection-induced pain is recommended.Keywords
1. Background
Use of propofol often results in pain upon injection, which can be distressing for patients (1-5). Many patients have reported some degree of pain or discomfort on propofol injection and several interventions have investigated using different drugs and methods to prevent this pain (6-10). Uses of lidocaine, alfentanil, cold saline, or cold propofol are among these methods. In addition, using a larger dorsal hand vein can reduce the pain; however, it might not be available in some patients (11).
Although several methods have been reported to nearly abolish the pain upon injection, further studies are needed to investigate effective and safe methods to reduce pain upon propofol injection. The nitrovasodilators are a various group of drugs that results in vascular relaxation by releasing nitric oxide (NO). These drugs imitate endothelium-derived NO; on the other hand, nitrates and sodium nitroprusside produce NO directly, independent of vascular endothelium (12). A few studies have been conducted to evaluate the use of nitroglycerine, as a single drug, for pain reduction in the patients undergoing propofol injection (13-16). This effect might be due to the pain modulating and anti-inflammatory characteristics of NO, which is a metabolite of nitroglycerine in smooth muscle cells of vessels (17-20).
2. Objectives
This study was performed to evaluate the effects of nitroglycerine on pain severity in patients undergoing propofol injection.
3. Patients and Methods
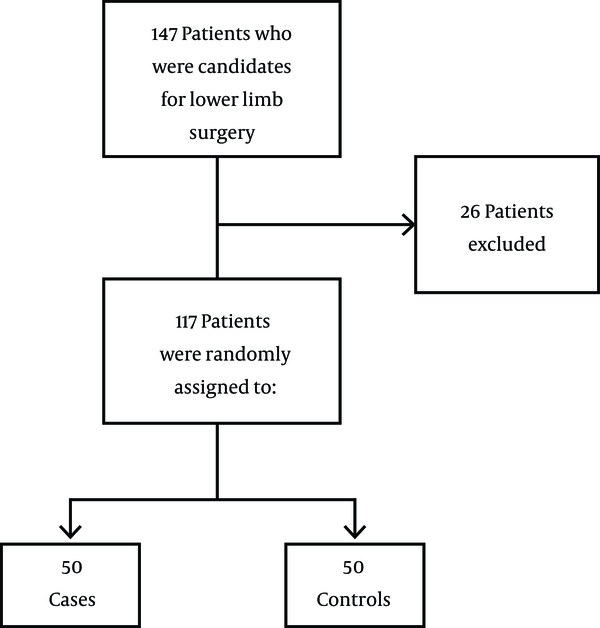
This double-blind randomized clinical trial was conducted in Imam Reza Hospital, Birjand University of Medical Sciences, Birjand City, Iran, 2011 - 2012. A total of 143 patients who were categorized as American Society of Anesthesiologist (ASA) class I and II, aged between 18 to 50 years, and were candidates for an open leg wound surgery were admitted to the hospital; 26 of these patients were excluded according to exclusion criteria and from the remaining 117, 100 patients were randomly selected. The sample size calculation formula was as follows (Equation 1):
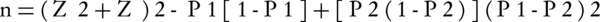
where n stands for sample size required in each group, P1 for expected proportion of subject to show no pain in case group, P2 for expected proportion of subject to show no pain in control group, (P1 - P2) for clinically significant difference, Zα /2 for 5% level of significance (1.96), and Zβ for 95% power (21). Based on the study of Nathanson, et al. (4), P1 and P2 were expected to be 0.7 and 0.03, respectively. Thus, n1 and n2 were calculated as 35 that gave us a total sample size of 70. To be more precise, the final sample size was decided to be 100 (50 in each group) (Figure 1).
The Study Participant’s Selection Flowchart
None of the participants had thin dorsal veins and any history of receiving analgesia or sedation within last 24 hours. In addition, none of the selected patients had contraindications for nitroglycerine use. Informed written consent was obtained from all participants and the Ethical Committee of Imam Reza hospital approved this study. Patients were randomly allocated to case and control groups using the random number table. Without any premedication after the institution of electrocardiogram, arterial blood pressure (systolic, diastolic, and mean arterial pressure) and pulse oximetry for monitoring (Saadat Alborz B7), two 20-G cannula was inserted into the dorsal vein of both hands. The right one was used for infusion of intravenous fluids and the left one was used for drug administration. Then, infusion of 3 mL/kg of 0.9% saline was started from right arm. Furthermore, patients in the case group received infusion of 20 μg of nitroglycerine, diluted in 5 mL of 0.9% saline from the left arm. We decided to choose 20 μg of nitroglycerine based on our goal, i.e., achieving the local effects of nitroglycerine without any sever hemodynamic effect such as sever tachycardia and hypotension. In many previous studies on nitroglycerine dosage, using 20 μg of nitroglycerine intravenously did not cause any severe hemodynamic effects. In addition, in previous studies on analgesic effects of nitroglycerine, the transdermal nitroglycerine patch was used, which was also used in congestive heart failure without any adverse effects and with a low bioavailability (22, 23). Patients in the control group received 5 mL of 0.9% saline from left arm. Administration time for both groups was ten seconds. Both the patient and the anesthesiologist were blinded to the type of administered fluid in the 5-mL syringes. The 5-mL syringes containing nitroglycerine or normal saline were prepared in the same appearance and color by a nurse who was also blinded to the purpose of the study. Twenty seconds later, 100-mg bolus dose of propofol (Lipuro, 10 mg/mL, B. Braun, Melsungen, Germany), which was kept at room temperature, was injected. Propofol was administered over a period of five seconds. Any behavioural signs such as facial grimacing, arm withdrawal, or tears were noted and recorded by the anesthesiologist. Then pain on injection was assessed using a four-point scale: “zero” for no pain, “one” for mild pain (pain only in response to questioning and without any behavioral signs), “two” for moderate pain (pain reported spontaneously without questioning), and “three” for severe pain (strong vocal response or response accompanied by facial grimacing, arm withdrawal, or tears). The induction of anesthesia was completed with the 1.5 mg/kg of propofol for each patient minus the initial 100-mg bolus dose; in addition, atracurium (0.5 mg/kg) and fentanyl (3 μg/kg) were administered and systolic and diastolic blood pressures and heart rate were recorded 30 seconds later. Oral intubation of the trachea was done three minutes after administration of atracurium. Anesthesia was continued with 100% oxygen and isoflurane. Within recovery period, the left hand was examined for pain, edema, or other reactions by the anesthesiologist who was blinded to the administered drug.
The age, sex, weight, homodynamic status (systolic and diastolic blood pressures and heart rate), drug adverse effects and pain severity were the study variables. Data was analyzed using SPSS 18.0 (SPSS Inc, Chicago, Illinois, the United States). Differences were tested by independent-samples t test, Fisher exact test, and Chi square test and were considered statistically significant at P values < 0.05.
4. Results
Table 1 illustrates the basic characteristics of the participants. The pain severity in nitroglycerine group was significantly less in comparison with the control group (P < 0.001) (Table 2). The local adverse reactions were only seen in three patients in control group while no patient in the case group showed any adverse reaction (P = 0.24). The systolic blood pressure showed no significant difference between two groups before and after the induction of anesthesia but the diastolic blood pressure and the heart rate were significantly different between the case and control groups (Table 3).
| Variables | Case | Control | P Valueb |
|---|---|---|---|
| Age, y | 34.1 ± 12.3 | 36.8 ± 11.9 | 0.16 |
| Weight, kg | 68.1 ± 10.8 | 68.5 ± 10.2 | 0.84 |
| Gender | |||
| Male | 30 (60) | 24 (48) | 0.12 |
| Female | 20 (40) | 26 (52) | - |
| Pain Severity | Case | Control | P Value b |
|---|---|---|---|
| None | 32 (64) | 9 (18) | < 0.001 |
| Mild | 13 (26) | 16 (32) | - |
| Moderate | 4 (8) | 12 (24) | - |
| Severe | 1 (2) | 13 (26) | - |
Comparison of Homodynamic Status Before and After the Induction of Anesthesia Between Case and Control Groups a,b
| Homodynamic Variables | Case | Control | P Value c |
|---|---|---|---|
| SBP before induction, mm Hg | 127.0 ± 15.1 | 123.8 ± 15.7 | 0.08 |
| SBP after induction, mm Hg | 100.5 ± 14.0 | 103.4 ± 13.7 | 0.07 |
| DBP before induction, mm Hg | 80.0 ± 8.46 | 77.9 ± 9.55 | 0.06 |
| DBP after induction, mm Hg | 57.5 ± 12.6 | 64.1 ± 12.3 | < 0.001 |
| Heart rate before induction, beats/min | 88.5 ± 17.2 | 77.2 ± 13.1 | < 0.001 |
| Heart rate after induction, beats/min | 84.3 ± 16.0 | 75.3 ± 9.69 | < 0.001 |
5. Discussion
To the best of our knowledge, this is the first study to investigate the effects of using intravenous nitroglycerine for reducing the severity of pain caused by propofol injection. This pain is a common problem with a higher frequency in young patients, patients with a thin peripheral vein, and female patients (11). In this study, the effect of applying nitroglycerin before injection of propofol was investigated in 100 patients of ASA classes I and II. The case group developed less pain during the propofol injection.
Nitroglycerin releases NO (24), which acts the same as endothelial NO, resulting in vasodilatation, decreased vascular resistance, lower blood pressure, inhibition of platelet aggregation and adhesion, inhibition of leukocyte adhesion and transmigration, and reduced vascular smooth muscle proliferation. On the other hand, nitrates and sodium nitroprusside directly produce NO, independent of vascular endothelium (24). Administration of nitrovasodilators results in the release of NO, which activates soluble guanylyl cyclase and produces cyclic GMP from guanosine triphosphate in smooth muscle cells (17, 18, 25, 26). Accumulation of cyclic GMP activates cyclic GMP-dependent protein kinase, which is involved in the opening of adenosine triphosphate (ATP)-sensitive K+ channel, to produce spinal or peripheral antinociception and in Na+/K+-ATPase activation (25, 27-29). Nonadrenergic noncholinergic inhibitory reactions to autonomic nerve stimulation are mostly mediated through NO (30). The sensory information processing is partly controlled by afferent nitrergic nerves (31). It has been shown that NO, which can be released from primary sensory nerves, can affect mesenteric vasodilatation (32). NO has an important role in afferent signaling of pain through the dorsal horn of the spinal cord and in autonomic control through nitrergic innervation. Release of NO from the peripheral endings of spinal afferents can stimulate many of their homeostatic actions (31, 33, 34). Some studies have stated that NO inhibitors attenuate the antinociceptive effects of morphine; on the other hand, others have concluded that NO inhibition promotes morphine-induced analgesia (24, 35). The NO formed by N-methyl-D-aspartate (NMDA)-receptor activation diffuses to adjacent nerve terminals to modulate neurotransmitter release (36). Moreover, NO generators have anti-inflammatory effects by blocking the neurogenic component of inflammatory edema when used topically (19, 37). We believe that our results were likely due to a relative dilution of the drug, resulting in a higher venous flow secondary to vasodilation.
In a study on 100 adults of ASA class I and II, scheduled for various elective surgical procedures under general anesthesia, Singh et al. concluded that granisetron, nitroglycerine, and magnesium sulfate were consecutively the most effective drugs in attenuating pain of intravenously injected propofol (38). Likewise, Turan et al. (39) suggested the application of transdermal nitroglycerin for reduction of pain severity of propofol injection. However, O’hara et al. (40) demonstrated that in comparison to nitroglycerine, lidocaine is associated with a decreased incidence of propofol-induced pain. In the current study, instead of topical nitroglycerine, intravenous nitroglycerine was used as a pain reduction agent; thus, the significant pain reduction effect of nitroglycerine can be due to its administration rout.
As a limitation, atracurium was used because we did not have access to cisatracurium. The hemodynamic effects of atracurium might have affected the hemodynamic results of our participants. However, use of a routine drug such as atracurium can be considered as an advantage because of its widespread use in Iran.
In conclusion, the use of nitroglycerine injection may improve analgesic effects without any sever hemodynamic consequences and additional adverse effects. Hence, its use to reduce the propofol injection-induced pain is recommended.
Acknowledgements
References
-
1.
Stark RD, Binks SM, Dutka VN, O'Connor KM, Arnstein MJ, Glen JB. A review of the safety and tolerance of propofol ('Diprivan'). Postgrad Med J. 1985;61 Suppl 3:152-6. [PubMed ID: 3877284].
-
2.
Bryson HM, Fulton BR, Faulds D. Propofol. An update of its use in anaesthesia and conscious sedation. Drugs. 1995;50(3):513-59. [PubMed ID: 8521772].
-
3.
Fulton B, Sorkin EM. Propofol. An overview of its pharmacology and a review of its clinical efficacy in intensive care sedation. Drugs. 1995;50(4):636-57. [PubMed ID: 8536552].
-
4.
Nathanson MH, Gajraj NM, Russell JA. Prevention of pain on injection of propofol: a comparison of lidocaine with alfentanil. Anesth Analg. 1996;82(3):469-71. [PubMed ID: 8623944].
-
5.
Tan CH, Onsiong MK. Pain on injection of propofol. Anaesthesia. 1998;53(5):468-76. [PubMed ID: 9659020].
-
6.
Brooker J, Hull CJ, Stafford M. Effect of lignocaine on pain caused by propofol injection. Anaesthesia. 1985;40(1):91-2. [PubMed ID: 3871594].
-
7.
McCrirrick A, Hunter S. Pain on injection of propofol: the effect of injectate temperature. Anaesthesia. 1990;45(6):443-4. [PubMed ID: 2200300].
-
8.
Barker P, Langton JA, Murphy P, Rowbotham DJ. Effect of prior administration of cold saline on pain during propofol injection. A comparison with cold propofol and propofol with lignocaine. Anaesthesia. 1991;46(12):1069-70. [PubMed ID: 1781537].
-
9.
Scott RP, Saunders DA, Norman J. Propofol: clinical strategies for preventing the pain of injection. Anaesthesia. 1988;43(6):492-4. [PubMed ID: 3261547].
-
10.
Golzari SE, Soleimanpour H, Mahmoodpoor A, Safari S, Ala A. Lidocaine and pain management in the emergency department: a review article. Anesth Pain Med. 2014;4(1). ee15444. [PubMed ID: 24660158]. https://doi.org/10.5812/aapm.15444.
-
11.
McCulloch MJ, Lees NW. Assessment and modification of pain on induction with propofol (Diprivan). Anaesthesia. 1985;40(11):1117-20. [PubMed ID: 3878103].
-
12.
Harrison DG, Bates JN. The nitrovasodilators. New ideas about old drugs. Circulation. 1993;87(5):1461-7. [PubMed ID: 8491000].
-
13.
Lohmann M, Moller P, Brynitz S, Bjerrum OW. Nitroglycerin ointment as aid to venepuncture. Lancet. 1984;1(8391):1416-7. [PubMed ID: 6145869].
-
14.
Wilkinson D, Anderson M, Gauntlett IS. Pain on injection of propofol: modification by nitroglycerin. Anesth Analg. 1993;77(6):1139-42. [PubMed ID: 8250304].
-
15.
Sen S, Ugur B, Aydin ON, Ogurlu M, Gursoy F, Savk O. The analgesic effect of nitroglycerin added to lidocaine on intravenous regional anesthesia. Anesth Analg. 2006;102(3):916-20. [PubMed ID: 16492852]. https://doi.org/10.1213/01.ane.0000195581.74190.48.
-
16.
Higa M, Takasu N, Tamanaha T, Nakamura K, Shimabukuro M, Sasara T, et al. Nitroglycerin spray rapidly improves pain in a patient with chronic painful diabetic neuropathy. Diabet Med. 2004;21(9):1053-4. [PubMed ID: 15317617].
-
17.
Lauretti GR, Oliveira AP, Juliao MC, Reis MP, Pereira NL. Transdermal nitroglycerine enhances spinal neostigmine postoperative analgesia following gynecological surgery. Anesthesiology. 2000;93(4):943-6. [PubMed ID: 11020743].
-
18.
Lauretti GR, Oliveira AP, Rodrigues AM, Paccola CA. The effect of transdermal nitroglycerin on spinal S(+)-ketamine antinociception following orthopedic surgery. J Clin Anesth. 2001;13(8):576-81. [PubMed ID: 11755327].
-
19.
Berrazueta JR, Losada A, Poveda J, Ochoteco A, Riestra A, Salas E, et al. Successful treatment of shoulder pain syndrome due to supraspinatus tendinitis with transdermal nitroglycerin. A double blind study. Pain. 1996;66(1):63-7. [PubMed ID: 8857632].
-
20.
Siamdoust SAR, Faiz SHR, Derakhshan P, Sakhayi M. Evaluation the Analgesic Effect of Nitroglycerin Added to Lidocaine in Intravenous Regional Anesthesia. Anesth Pain J. 2011;1(3):17-23.
-
21.
Sakpal TV. Sample size estimation in clinical trial. Perspect Clin Res. 2010;1(2):67-9. [PubMed ID: 21829786].
-
22.
den Uil CA, Brugts JJ. Impact of intravenous nitroglycerin in the management of acute decompensated heart failure. Curr Heart Fail Rep. 2015;12(1):87-93. [PubMed ID: 25301529]. https://doi.org/10.1007/s11897-014-0230-8.
-
23.
Varon J, Marik PE. Perioperative hypertension management. Vasc Health Risk Manag. 2008;4(3):615-27. [PubMed ID: 18827911].
-
24.
Toda N, Kishioka S, Hatano Y, Toda H. Modulation of opioid actions by nitric oxide signaling. Anesthesiology. 2009;110(1):166-81. [PubMed ID: 19104184]. https://doi.org/10.1097/ALN.0b013e31819146a9.
-
25.
Mixcoatl-Zecuatl T, Flores-Murrieta FJ, Granados-Soto V. The nitric oxide-cyclic GMP-protein kinase G-K+ channel pathway participates in the antiallodynic effect of spinal gabapentin. Eur J Pharmacol. 2006;531(1-3):87-95. [PubMed ID: 16438951]. https://doi.org/10.1016/j.ejphar.2005.12.006.
-
26.
Lauretti GR, Lima IC, Reis MP, Prado WA, Pereira NL. Oral ketamine and transdermal nitroglycerin as analgesic adjuvants to oral morphine therapy for cancer pain management. Anesthesiology. 1999;90(6):1528-33. [PubMed ID: 10360847].
-
27.
Scavone C, Munhoz CD, Kawamoto EM, Glezer I, de Sa Lima L, Marcourakis T, et al. Age-related changes in cyclic GMP and PKG-stimulated cerebellar Na,K-ATPase activity. Neurobiol Aging. 2005;26(6):907-16. [PubMed ID: 15718050]. https://doi.org/10.1016/j.neurobiolaging.2004.08.013.
-
28.
Garthwaite J, Southam E, Boulton CL, Nielsen EB, Schmidt K, Mayer B. Potent and selective inhibition of nitric oxide-sensitive guanylyl cyclase by 1H-[1,2,4]oxadiazolo[4,3-a]quinoxalin-1-one. Mol Pharmacol. 1995;48(2):184-8. [PubMed ID: 7544433].
-
29.
Brito GA, Sachs D, Cunha FQ, Vale ML, Lotufo CM, Ferreira SH, et al. Peripheral antinociceptive effect of pertussis toxin: activation of the arginine/NO/cGMP/PKG/ ATP-sensitive K channel pathway. Eur J Neurosci. 2006;24(4):1175-81. [PubMed ID: 16930443].
-
30.
Kiss JP, Vizi ES. Nitric oxide: a novel link between synaptic and nonsynaptic transmission. Trends Neurosci. 2001;24(4):211-5. [PubMed ID: 11250004].
-
31.
Riedel W, Neeck G. Nociception, pain, and antinociception: current concepts. Z Rheumatol. 2001;60(6):404-15. [PubMed ID: 11826734].
-
32.
Zheng Z, Shimamura K, Anthony TL, Travagli RA, Kreulen DL. Nitric oxide is a sensory nerve neurotransmitter in the mesenteric artery of guinea pig. J Auton Nerv Syst. 1997;67(3):137-44. [PubMed ID: 9479665].
-
33.
Zochodne DW, Levy D. Nitric oxide in damage, disease and repair of the peripheral nervous system. Cell Mol Biol (Noisy-le-grand). 2005;51(3):255-67. [PubMed ID: 16191393].
-
34.
Toda N, Okamura T. Possible role of nitric oxide in transmitting information from vasodilator nerve to cerebroarterial muscle. Biochem Biophys Res Commun. 1990;170(1):308-13. [PubMed ID: 2164808].
-
35.
Karbasy SH, Derakhshan P. Effects of Opium Addiction on Level of Sensory Block in Spinal Anesthesia With Bupivacaine for Lower Abdomen and Limb Surgery: a Case-Control Study. Anesth Pain Med J. 2014;4(5):e21571.
-
36.
Buccafusco JJ, Terry AJ, Shuster L. Spinal NMDA receptor--nitric oxide mediation of the expression of morphine withdrawal symptoms in the rat. Brain Res. 1995;679(2):189-99. [PubMed ID: 7633880].
-
37.
Faiz SH, Rahimzadeh P, Sakhaei M, Imani F, Derakhshan P. Anesthetic effects of adding intrathecal neostigmine or magnesium sulphate to bupivacaine in patients under lower extremities surgeries. J Res Med Sci. 2012;17(10):918-22. [PubMed ID: 23825989].
-
38.
Singh DK, Jindal P, Singh G. Comparative study of attenuation of the pain caused by propofol intravenous injection, by granisetron, magnesium sulfate and nitroglycerine. Saudi J Anaesth. 2011;5(1):50-4. [PubMed ID: 21655017].
-
39.
Turan A, Karamanlioglu B, Memis D, Pamukcu Z. Alternative application site of transdermal nitroglycerin and the reduction of pain on propofol injection. Eur J Anaesthesiol. 2003;20(2):170-2. [PubMed ID: 12622508].
-
40.
O'Hara JJ, Sprung J, Laseter JT, Maurer WG, Carpenter T, Beven M, et al. Effects of topical nitroglycerin and intravenous lidocaine on propofol-induced pain on injection. Anesth Analg. 1997;84(4):865-9. [PubMed ID: 9085972].