Abstract
Keywords
1. Introduction
The conventional direct laryngoscope is a rigid scope with a light on the blade that provides a line of sight for viewing the larynx and the glottis. The failure of such devices to provide a view of the larynx has led to the generation of indirect viewing laryngoscopes. A video laryngoscope offers a clear view of the larynx and the glottis (1, 2). However, the lifting of the epiglottis can be difficult not only with a direct laryngoscope (3, 4), but also with a video laryngoscope due to the closeness of the posterior pharyngeal wall. This difficulty can result in problems with intubation. We believe that the use of a simple stylet can aid the lifting of the epiglottis, thus offering a clear view of the glottis. Here, we present a case series in which the use of a simple stylet resolved difficulties with lifting the epiglottis in patients undergoing intubation with a video laryngoscope under general anesthesia.
2. Case Presentation
2.1. The First Case of Elevation of the Epiglottis
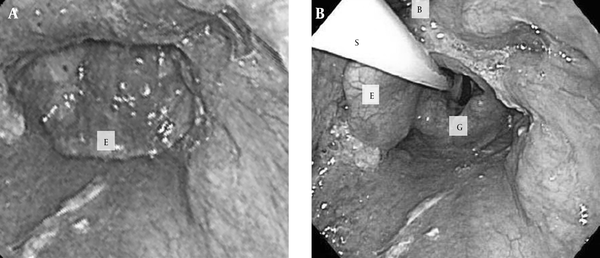
A 56-year-old male patient was presented for arthroplasty of the right shoulder. After the induction of 7% Sevoflurane, an attempt was made to insert a tracheal tube. A large, floppy epiglottis, lying in complete apposition with the posterior wall of the pharynx, blocked the view of the glottis. The use of the Pentax AWS and the Glide Scope®, combined with the jaw-thrust maneuver, proved fruitless (Figure 1A). However, elevation of the epiglottis with a stylet provided glottic exposure (Figure 1B). A nurse was asked to hold the stylet, thus allowing an anesthesiologist to spray lidocaine into the trachea and insert an endotracheal tube, while watching the image displayed on a high-resolution LCD monitor.
Visualized View of the Larynx Using the A, Glide Scope®; B, a Stylet
2.2. The Study Protocol
We hypothesized that a stylet could be a useful aid for intubation. In cases where the lifting of the epiglottis and exposure of the glottis were not achieved using a Glide Scope®, it was supposed that the stylet might help to lift the epiglottis, thus facilitating viewing of the glottis and allowing a tracheal tube to be inserted. During the experiment, the anesthesiologist performed the laryngoscopy by holding the Glide Scope® in his left hand and elevating the epiglottis with a stylet held in the right hand. This technique permitted viewing of the glottis on the LCD monitor. A nurse was then asked to hold the stylet in order to keep the view clear, while the anesthesiologist passed a regular tracheal tube into the trachea with his right hand. The method was simple and was performed easily, without any special equipment being required. After gaining approval from the IRB and oral, informed consent from the proposed participants, we examined the effectiveness of this method in the cases of 154 patients, in whom the epiglottis was visible but not lifted, thus preventing the viewing of the glottis with the Glide Scope®. The patients had a median age of 63 (range; 13 - 96), and consisted of 88 males and 66 females. In all cases, the views obtained were sufficient to allow the tube to be inserted into the trachea. However, in 7 patients (male =3, female =4) the method was not successful. The stylet blocked the tube from entering the trachea in 6 of these subjects. As the opening of the mouth was narrow in these cases, there was no room in the mouth to manipulate the tube, even with a clear vision of the glottis. In the 7th case, use of the stylet failed to offer a view of the glottis in a female subject. In all these 7 patients, fiberoptic intubation was chosen. No mechanical injury of the epiglottis with the stylet was observed in any of the 154 cases. Furthermore, none of the subjects complained of laryngeal disturbances postoperatively.
3. Discussion
The failure of a direct laryngoscope to provide a view of the larynx has led to the development of indirect viewing laryngoscopes. Video laryngoscopes allow a clear view of the larynx and the glottis to be obtained (1, 2).
When facilitating endotracheal intubation, we have found that there are some patients for whom neither a direct laryngoscope, nor a video laryngoscope lifts the epiglottis away from the posterior pharyngeal wall sufficiently, which results in a poor view of the glottis and difficulties with intubation. In anesthetized patients, there is a reduction in muscle tone that causes the soft palate, the base of the tongue, and the epiglottis to be closer to the posterior pharyngeal wall than usual (3-5). The jaw-thrust maneuver has been advocated by several investigators as a way of opening the airway and obtaining a view of the glottis (3, 6). However, the maneuver is useless in some cases, as reported in our first case. Since the lifting of the epiglottis with a simple stylet can be performed easily, without any special equipment, we determined that this method could be the simple and helpful aid required in such cases.
In conclusion, we used a basic stylet alongside a video laryngoscope to resolve the difficulties associated with lifting the epiglottis of patients undergoing intubation under general anesthesia. By using this method, we discovered that it is a simple and helpful solution.
Acknowledgements
References
-
1.
Agro F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization. Br J Anaesth. 2003;90(5):705-6. [PubMed ID: 12697606].
-
2.
Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The GlideScope Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005;94(3):381-4. [PubMed ID: 15567809]. https://doi.org/10.1093/bja/aei041.
-
3.
Aoyama K, Takenaka I, Nagaoka E, Kadoya T. Jaw thrust maneuver for endotracheal intubation using a fiberoptic stylet. Anesth Analg. 2000;90(6):1457-8. [PubMed ID: 10825343].
-
4.
Takenaka I, Aoyama K, Kadoya T, Sata T, Shigematsu A. Fibreoptic assessment of laryngeal aperture in patients with difficult laryngoscopy. Can J Anaesth. 1999;46(3):226-31. [PubMed ID: 10210045]. https://doi.org/10.1007/BF03012600.
-
5.
Rewari V, Ramachandran R, Trikha A. Lingual traction: a useful manoeuvre to lift the epiglottis in a difficult oral fibreoptic intubation. Acta Anaesthesiol Scand. 2009;53(5):695-6. [PubMed ID: 19419380]. https://doi.org/10.1111/j.1399-6576.2009.01934.x.
-
6.
Murashima K, Fukutome T. Effect of jaw-thrust manoeuvre on the laryngeal inlet. Anaesthesia. 1998;53(2):203-4. [PubMed ID: 9534652].