Abstract
Background:
Peripheral nerve block is an accepted method in lower limb surgeries regarding its convenience and good tolerance by the patients. Quick performance and fast sensory and motor block are highly demanded in this method. The aim of the present study was to compare 2 different methods of sciatic and tibial-peroneal nerve block in lower limb surgeries in terms of block onset.Methods:
In this clinical trial, 52 candidates for elective lower limb surgery were randomly divided into 2 groups: sciatic nerve block before bifurcation (SG; n = 27) and separate tibial-peroneal nerve block (TPG; n = 25) under ultrasound plus nerve stimulator guidance. The mean duration of block performance, as well as complete sensory and motor block, was recorded and compared between the groups.Results:
The mean duration of complete sensory block in the SG and TPG groups was 35.4 ± 4.1 and 24.9 ± 4.2 minutes, respectively, which was significantly lower in the TPG group (P = 0.001). The mean duration of complete motor block in the SG and TPG groups was 63.3 ± 4.4 and 48.4 ± 4.6 minutes, respectively, which was significantly lower in the TPG group (P = 0.001). No nerve injuries, paresthesia, or other possible side effects were reported in patients.Conclusions:
According to the present study, it seems that TPG shows a faster sensory and motor block than SG.Keywords
Sciatic Nerve Block Tibial-Peroneal Nerve Block Ultrasound Lower Limb Surgeries
1. Background
Peripheral nerve block is a simple procedure used in lower limb surgeries, especially under the guidance of ultrasound and nerve stimulators. It is associated with a low risk of neurological and systemic complications (1, 2). In this procedure, quick performance and fast sensory and motor block are highly demanded. It is considered a suitable substitution for general anesthesia, protecting patients (especially patients with cardiopulmonary disorders) against the unwanted complications of general anesthesia.
Peripheral nerve block in combination with slight sedation facilitates many surgical procedures and provides better positioning for the patient. In the postoperative period, uncontrolled pain delays the onset of mobility and disrupts physiotherapy. Systemic narcotics, even in controlled patients, do not induce a pain-free state and may result in a high incidence of nausea and vomiting. On the other hand, spinal and epidural anesthesia may result in systemic complications, such as hypotension, urinary retention, and movement disorders in the lower extremities.
Compared to central nerve block, peripheral nerve block is more selective, with the lowest interference in bladder function and limb movements. Peripheral nerve catheter placement can be used in postoperative pain control, as well. Sciatic nerve is responsible for lower-extremity innervation and consists of 2 nerve trunks: tibial nerve (TN) and common peroneal nerve (CPN). These nerves separate at 5-7 cm above the popliteal fossa; TN lies medial and CPN lateral to the fossa (2-5).
Several studies have investigated the mechanism and effectiveness of blocking the sciatic nerve, as a major nerve of the lower limbs, and found that blocking might take 30 - 60 minutes to start when conducted before sciatic nerve bifurcation (3, 6-8). We hypothesized that block onset might vary with different approaches along the nerve pathway. The aim of this study was to determine and compare the onset of blockade between proximal and distal approaches, ie, sciatic nerve block before bifurcation (SG) and separate tibial and peroneal nerve block (TPG).
2. Methods
In this double-blind clinical trial, block randomization was applied as the sampling method. The sample size was calculated at 26 cases per group, using Cohen’s table (power, 80%; alpha, 0.05). This clinical trial was registered in the Iranian Registry of Clinical Trials (IRCT2015110212642N20).
The inclusion criteria were as follows: 1) willingness to participate in the study (informed consent); 2) ability to answer the verbal questions; 3) age range of 20 - 65 years; 4) being a candidate for unilateral debridement below the knee; and 5) ASA classification of I or II. On the other hand, the exclusion criteria were: 1) history of type II diabetes; 2) peripheral arterial disease; 3) coagulopathy; 4) peripheral neuropathy; and 5) incomplete sensory block after 45 minutes.
In the current study, based on the inclusion/exclusion criteria and block randomization, 52 patients were selected. After obtaining written informed consents from the patients, they were randomly categorized into 2 groups: SG, injection into the nerve 5 cm proximal to nerve bifurcation; and TPG, separate injections into TN and CPN at the popliteal fossa. All the patients received intravenous injections of midazolam (1 mg) and fentanyl (50 mcg) before nerve blocking.
Patients in both groups were positioned laterally and were monitored continuously via electrocardiography, SpO2 measurement, and noninvasive blood pressure monitoring during nerve blockade and surgery. Sciatic nerve block was performed under the guidance of both ultrasound and nerve stimulator using a posterior approach in a lateral decubitus position.
A linear probe (3 - 8 MHz, s-nerve, Sonosite, USA) with an in-plane approach and a 7-cm sonovisible needle (22-guage; Pajunk, Germany) was used to inject 15 cc of marcaine 0.5%, 15 cc of lidocaine 1%, and epinephrine 1:400,000 (30 cc in total). The needle tip was adjusted if necessary to achieve circumferential spread. In the TPG group, the patient was placed in a lateral position, and 15 cc of the solution was injected around CPN and 15 cc around TN while reaching circumferential spread. Sensory and motor block was assessed by a person blind to the experiment at 10 minutes after the injections. Then, the assessments were carried out every 5 minutes for 45 minutes.
Sensory block was assessed in TN and CPN regions, using the pinprick test with the following scorings system: 0, no change detected; 1, reduced sensation; and 2, complete absence of pinprick sensation. In addition, motor block was scored as follows: 0, no change compared to the baseline; 1, reduced force and movement; 2, complete absence of force and movement. Time of block onset was defined as reaching a sensory score of 2 during 45 minutes in both TN and CPN zones.
Duration of imaging was measured from the time of touching the ultrasound probe until obtaining a proper image. Duration of needling was measured from the moment the needle touched the skin until the end of local anesthetic injection. Moreover, duration of block was defined as the total time of imaging and needling. Frequency of needling and complications, including paresthesia and vascular puncture, was documented for each participant.
The data were analyzed using SPSS version 13. Kolmogorov-Smirnov test was used to assess the normal distribution of variables. The parametric variables were presented as mean ± standard deviation (SD) and analyzed by student t test. Nonparametric variables were analyzed using Chi square or Mann-Whitney U test. P value less than 0.05 was considered statistically significant
3. Results
In this study, 52 patients, who were candidates for selective surgery below the knee, were evaluated. Patients were randomly categorized into 2 groups: SG (n = 27) and TPG (n = 25). The baseline characteristics of the participants are presented in Table 1. Distribution of demographic variables was normal, and the groups showed no significant difference regarding age, sex, weight, or height (P > 0.05).
| Variables | Groups | P Valueb | |
|---|---|---|---|
| SG (n = 27) | TPG (n = 25) | ||
| Age, y | 49.03 ± 13.8 | 47.08 ± 14.5 | 0.6 |
| Sex | 0.73 | ||
| Male | 16 (59.2) | 15 (60) | |
| Female | 11 (40.7) | 10 (40) | |
| Height, cm | 176.6 ± 5.8 | 173.5 ± 21.1 | 0.4 |
| Weight, kg | 79.8 ± 7.5 | 89.8 ± 7.7 | 0.7 |
The mean duration of needling and imaging was not significantly different between the groups (P > 0.05). In all patients (except 6 cases), the first attempt of needling was successful. In 3 patients from each group, a second attempt was required, which was successful and showed no significant difference between the groups (P > 0.05). All subjects showed successful blockade and completed the study without general anesthesia induction. The success of sensory block was 100% and 22.2% in the TPG and SG groups at 35 minutes, respectively. At 45 minutes, successful sensory block was achieved in all patients (Table 2).
| Variables | Groups | P Valueb | |
|---|---|---|---|
| SG (n = 27) | TPG (n = 25) | ||
| Needling time, min | 2.4 ± 0.5 | 2.8 ± 1.06 | 0.1 |
| Imaging time, min | 4.3 ± 1.4 | 3.9 ± 1.07 | 0.2 |
| Blocking time, min | 6.8 ± 1.8 | 6.7 ± 1.09 | 0.8 |
| Complete sensory block time, min | 35.4 ± 4.1 | 24.9 ± 4.2 | < 0.001 |
| Complete motor block time, min | 63.3 ± 4.4 | 48.4 ± 4.6 | < 0.001 |
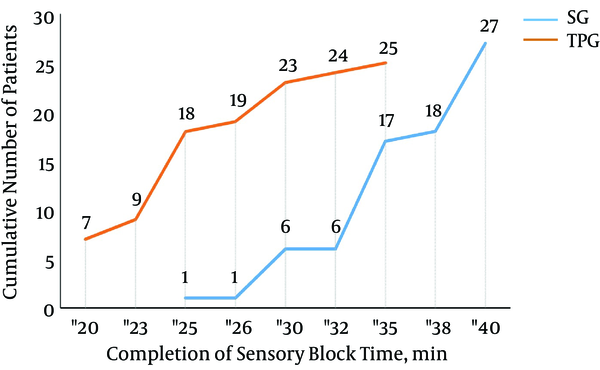
Distribution of the cumulative number of patients with respect to sensory and motor block success is illustrated in Figures 1 and 2. The fastest complete sensory block in the SG group was reported at 25 minutes (3.7%), while in this period, 18 (72%) patients in the TPG group showed complete block. All the patients in the TPG group reached complete sensory block at 35 minutes, while only 17 (62.9%) patients in the SG group showed complete block in this period (Figure 1).
The Cumulative Number of Patients According to Complete Sensory Block Time in the TPG and SG Groups
The Cumulative Number of Patients According to Complete Motor Block Time in the TPG and SG Groups
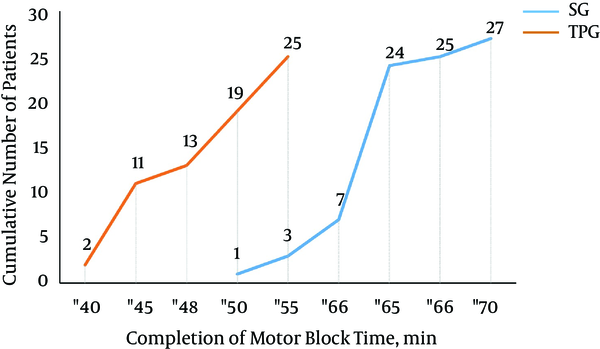
The first case of motor block in the SG group was reported at 50 minutes (3.7%), while in the TPG group, 19 (76%) patients had complete motor block at 50 minutes. After 55 minutes, all the patients in the TPG group (100%) showed complete motor block, while only 3 (11.1%) patients in the SG group had complete motor block (Figure 2). No cases of nerve injury, paresthesia, or other complications were reported in the patients.
4. Discussion
Recently, ultrasound imaging has gained popularity in regional anesthesia due to enhanced visibility of peripheral nerves during nerve block, reduced duration of the procedure, faster complete sensory block, reduced volume of needed drugs for successful block, and decreased incidence of complications or side effects. Moreover, integration of nerve stimulators and less needle puncture has revealed favorable results (6, 9-12).
Based on the results of this clinical trial, both sciatic and separate tibial-peroneal nerve block approaches are simple and quick methods under the guidance of ultrasound and neurostimulators, while in TPG, complete block can be achieved in a shorter period. In this regard, in a study by Prasad et al. 50 candidates of elective surgery below the knee were randomly selected and underwent ultrasound-guided sciatic nerve block at 5 cm distal and 3 cm proximal to the sciatic nerve bifurcation. In the distal group, the onset of sensory and motor block was 30% shorter than the proximal group; therefore, it is preferable to use the distal method if faster block is needed (3). Similar results were observed in the current study, indicating the faster onset of sensory block in the TPG group (20%), compared to the SG group.
In another study by Buys et al. 76 patients (candidates for foot or ankle surgery) underwent ultrasound-guided sciatic nerve block proximal and distal to nerve bifurcation. The used solution was mepivacaine plus clonidine and bicarbonate (30 cc in total). Patients in the TPG group reached complete nerve block significantly faster than the SG group (19.2 minutes vs. 26.1 minutes). They concluded that TN and CPN blockade in the popliteal fossa is a faster approach (4).
In the current study, none of the patients showed complete sensory block in less than 20 minutes (shortest time, 20 minutes in the TPG group). The differences in the block onset time between the present study and the one performed by Buys et al. might be attributed to the use of different solutions and approaches in these studies (posterior sciatic nerve approach with nerve stimulation versus a lateral approach without stimulation).
In another study, patients underwent ultrasound-guided sciatic nerve block in the popliteal fossa via subepineural sciatic nerve injection and showed a higher success rate and efficacy than TPG (5); these findings are not in agreement with the present results. Furthermore, Yamamoto performed ultrasound-guided subgluteal sciatic nerve block with multiple and single injections and concluded that multiple injections resulted in a higher rate of sensory and motor block due to a better drug spread (7).
Use of both TN and CPN responses with a double versus single injection-stimulation approach has been assessed in previous research. A double injection-stimulation strategy was not found to be similar to separate TN and CPN injections, especially since the procedure was performed upper than the level of sciatic nerve bifurcation, and the results were obtained without ultrasound guidance (8).
Based on the mentioned results, it can be concluded that solution volume and concentration, use of different additives, techniques, and approaches, point of needle entry along the nerve pathway, distance between the needle tip and the nerve, and even current intensity at which peripheral nerve stimulation is achieved can affect the results, leading to discrepancies in the findings (13-16).
In the current study, although both volume and concentration of anesthetic solution were similar in the groups, different needle entry points produced significantly different results. We found that ultrasound guidance for separate TN and CPN blockade distal to sciatic nerve bifurcation in the popliteal fossa leads to a more rapid complete block than a prebifurcation approach. Overall, further studies should be performed on this subject with different drugs and techniques and a larger sample size. Moreover, evaluation of satisfaction and pain severity during and after the procedure can be useful in this process.
4.1. Conclusions
The results of the current study showed that separate TN and CPN blockade is a faster method in below-knee surgeries. Further studies should be performed to determine the best and fastest technique and solution with fewer complications.
References
-
1.
Provenzano DA, Viscusi ER, Adams SJ, Kerner MB, Torjman MC, Abidi NA. Safety and efficacy of the popliteal fossa nerve block when utilized for foot and ankle surgery. Foot Ankle Int. 2002;23(5):394-9. [PubMed ID: 12043982]. https://doi.org/10.1177/107110070202300504.
-
2.
Kopka A, Serpell MG. Distal nerve blocks of the lower limb. Continuing Education in Anaesthesia, Critical Care & Pain. 2005;5(5):166-70. https://doi.org/10.1093/bjaceaccp/mki044.
-
3.
Prasad A, Perlas A, Ramlogan R, Brull R, Chan V. Ultrasound-guided popliteal block distal to sciatic nerve bifurcation shortens onset time: a prospective randomized double-blind study. Reg Anesth Pain Med. 2010;35(3):267-71. [PubMed ID: 20921838]. https://doi.org/10.1097/AAP.0b013e3181df2527.
-
4.
Buys MJ, Arndt CD, Vagh F, Hoard A, Gerstein N. Ultrasound-guided sciatic nerve block in the popliteal fossa using a lateral approach: onset time comparing separate tibial and common peroneal nerve injections versus injecting proximal to the bifurcation. Anesth Analg. 2010;110(2):635-7. [PubMed ID: 19996137]. https://doi.org/10.1213/ANE.0b013e3181c88f27.
-
5.
Tran DQ, Dugani S, Pham K, Al-Shaafi A, Finlayson RJ. A randomized comparison between subepineural and conventional ultrasound-guided popliteal sciatic nerve block. Reg Anesth Pain Med. 2011;36(6):548-52. [PubMed ID: 22005661]. https://doi.org/10.1097/AAP.0b013e318235f566.
-
6.
Sala-Blanch X, de Riva N, Carrera A, Lopez AM, Prats A, Hadzic A. Ultrasound-guided popliteal sciatic block with a single injection at the sciatic division results in faster block onset than the classical nerve stimulator technique. Anesth Analg. 2012;114(5):1121-7. [PubMed ID: 22366843]. https://doi.org/10.1213/ANE.0b013e318248e1b3.
-
7.
Yamamoto H, Sakura S, Wada M, Shido A. A prospective, randomized comparison between single- and multiple-injection techniques for ultrasound-guided subgluteal sciatic nerve block. Anesth Analg. 2014;119(6):1442-8. [PubMed ID: 25268398]. https://doi.org/10.1213/ANE.0000000000000462.
-
8.
Paqueron X, Bouaziz H, Macalou D, Labaille T, Merle M, Laxenaire MC, et al. The lateral approach to the sciatic nerve at the popliteal fossa: one or two injections? Anesth Analg. 1999;89(5):1221-5. [PubMed ID: 10553838].
-
9.
Rahimzadeh P, Faiz SH. Ultrasound a new paradigm in regional anesthesia and pain management. Anesth Pain Med. 2013;3(2):228-9. [PubMed ID: 24282772]. https://doi.org/10.5812/aapm.13363.
-
10.
Gorsewski G, Dinse-Lambracht A, Tugtekin I, Gauss A. [Ultrasound-guided peripheral regional anesthesia : placement and dosage of local anesthetics]. Anaesthesist. 2012;61(8):711-21. [PubMed ID: 22790475]. https://doi.org/10.1007/s00101-012-2045-x.
-
11.
Choquet O, Morau D, Biboulet P, Capdevila X. Where should the tip of the needle be located in ultrasound-guided peripheral nerve blocks? Curr Opin Anaesthesiol. 2012;25(5):596-602. [PubMed ID: 22821146]. https://doi.org/10.1097/ACO.0b013e328356bb40.
-
12.
Eldegwy MH, Ibrahim SM, Hanora S, Elkarta E, Elsily AS. Ultrasound-Guided Sciatic Politeal Nerve Block: A Comparison of Separate Tibial and Common Peroneal Nerve Injections Versus Injecting Proximal to the Bifurcation. Middle East J Anaesthesiol. 2015;23(2):171-6. [PubMed ID: 26442393].
-
13.
Tiyaprasertkul W, Bernucci F, Gonzalez AP, Leurcharusmee P, Yazer MS, Techasuk W, et al. A Randomized Comparison Between Single- and Triple-Injection Subparaneural Popliteal Sciatic Nerve Block. Reg Anesth Pain Med. 2015;40(4):315-20. [PubMed ID: 25923820]. https://doi.org/10.1097/AAP.0000000000000253.
-
14.
Safari S, Rahimzadeh P, Haghighi M. Local infiltration anesthesia: does it really work? Ann Transl Med. 2015;3(18):275. [PubMed ID: 26605321]. https://doi.org/10.3978/j.issn.2305-5839.2015.09.24.
-
15.
Germain G, Levesque S, Dion N, Nadeau MJ, Cote D, Nicole PC, et al. Brief reports: a comparison of an injection cephalad or caudad to the division of the sciatic nerve for ultrasound-guided popliteal block: a prospective randomized study. Anesth Analg. 2012;114(1):233-5. [PubMed ID: 22003214]. https://doi.org/10.1213/ANE.0b013e3182373887.
-
16.
Arcioni R, Palmisani S, Della Rocca M, Romano S, Mercieri M, De Blasi RA, et al. Lateral popliteal sciatic nerve block: a single injection targeting the tibial branch of the sciatic nerve is as effective as a double-injection technique. Acta Anaesthesiol Scand. 2007;51(1):115-21. [PubMed ID: 17073859]. https://doi.org/10.1111/j.1399-6576.2006.01164.x.