Abstract
Background:
Daily clinical practice shows us how diametrically different surgical outcomes can occur in particular groups of patients sharing the same diagnosis and being subjected to the same treatment. Patient-reported outcomes appear to be significantly influenced by social factors and patients’ emotional status. Data on such variables were collated and analyzed statistically with the aim of confirming our clinical observations.Methods:
We analyzed a group of 100 patients following cervical disc surgery. The clinical evaluation was based on a visual analog scale (VAS) for pain and the neck disability index (NDI). Non-clinical data comprised education status, employment status, body mass index (BMI), and history of depressive episodes in the period immediately preceding the surgery, which was investigated using the Beck Depression Inventory (BDI).Results:
Patients who had completed university or secondary school education had a significantly lower BMI and lower BDI scores and they reported less pain at 12 months postoperatively than patients with vocational or elementary school education only. Patients who were employed at the time of the study or were retired demonstrated significantly lower NDI scores both before the surgery and at 12 months postoperatively, as well as lower BDI scores compared to those who were unemployed or drew disability pensions. Factors such as age or BMI score did not exert a direct effect on treatment outcomes assessed as changes in the VAS and NDI scores.Conclusions:
Surgical treatment for the cervical disc disease decreases pain and improves patients’ quality of life. Treatment outcomes are also influenced by social factors and patients’ emotional status.Keywords
1. Background
The stimulus to carry out the present study came from daily observations of diametrically different responses of particular groups of patients to surgical treatment despite the patients sharing a diagnosis and having been subjected to the same treatment, including postoperative care. Patient-reported outcomes appear to be significantly influenced by social factors and patients’ emotional status. In this paper, data on such variables were collated and analyzed statistically with the aim of confirming our daily clinical observations. Anterior cervical discectomy and fusion (ACDF) is the established gold standard for the degenerative cervical spine disease. Interbody fusion is preferably performed with various types of cages, mostly made of titanium or polyetheretherketone (PEEK). PEEK cages have a modulus of elasticity closely resembling that of cortical bone, which might lead to advantages in load sharing and stress distribution (1).
2. Methods
We analyzed a group of 100 patients following cervical discectomy from an anterior approach with interbody PEEK cages stabilization. All patients were operated on by the same surgeon with the same technique and all received implants of the same type. The clinical evaluation was based on a visual analog scale (VAS) for pain and the neck disability index (NDI). Patients completed questionnaires before surgery and at 1, 6, and 12 months after the surgery. The NDI is a standard instrument for measuring self-rated disability due to neck pain. It is a condition-specific functional status questionnaire with 10 items including pain, personal care, lifting, reading, headaches, concentration, work, driving, sleeping, and recreation. Non-clinical data comprised education status, employment status, body mass index (BMI), and a history of depressive episodes in the period immediately preceding the surgery, which was investigated using the Beck Depression Inventory (BDI). The BDI is one of the most widely used screening instruments for measuring the severity of depression. The inventory is composed of items related to depressive symptoms, cognition, and physical symptoms. The data were analyzed statistically. To all calculations, we used Statistica StatSoft V. 10 program. Descriptive statistics included frequency distribution for categorical variables and means and standard deviations for continuous variables. The Student’s t-test (BMI) or Mann-Whitney U (BDI) test was used for the Quantitative and Chi-square test for the qualitative variables. The distribution of the group was analyzed with the Kolmogorov-Smirnov test. The significance level was set at P ≤ 0.05. The correlations between the parameters were analyzed with Pearson and Kendall’s tau or rho-Spearman Correlation tests.
3. Results
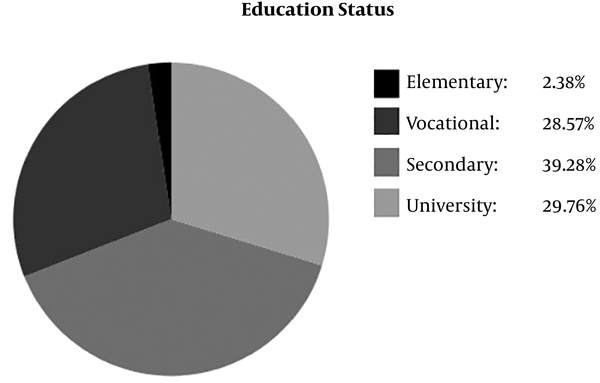
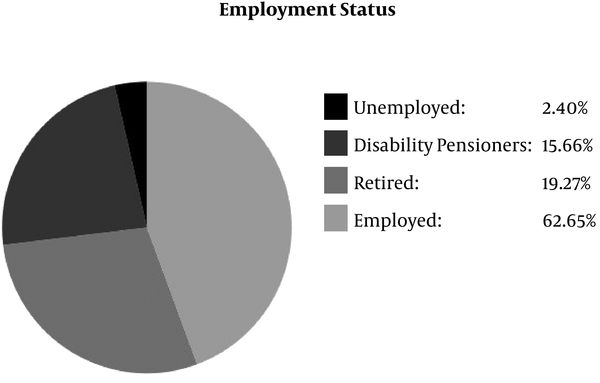
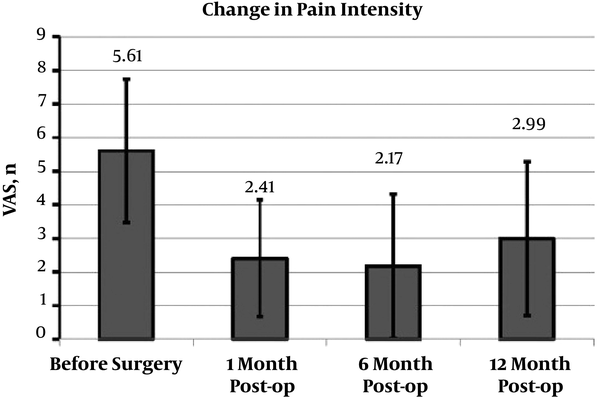
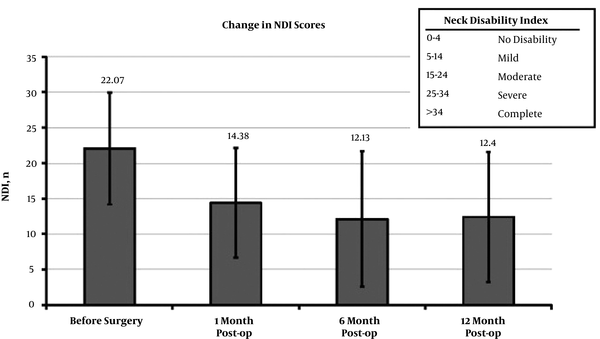
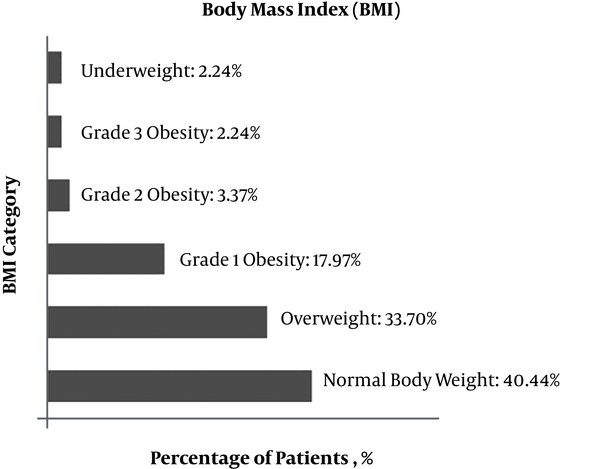
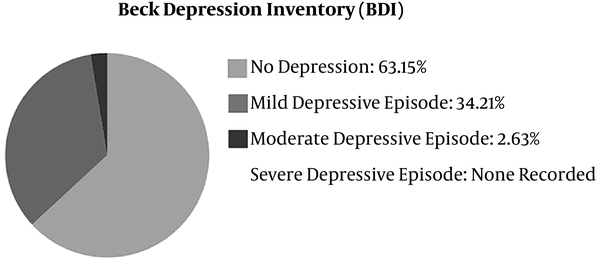
Pain intensity (VAS) changed from a mean of 5.61 ± 2.22 before surgery to 2.99 ± 2.14 at 12 months (change: 2.84 ± 2.77). NDI scores changed from a mean of 22.07 ± 8.22 before surgery to 12.40 ± 8.87 at 12 months (change: 11.16 ± 9.52). Changes in VAS score were correlated with changes in NDI score (P < 0.01, r = 0.49). Patients’ mean age was 49.61 ± 10.76 years, with women accounting for 76% of the group and men accounting for 24%. Education and employment status data are presented in Figures 1 and 2. The mean VAS and NDI scores at specific time points, information about body mass index, and history of depressive episodes are presented in Figures 3 - 6. Pain reported before surgery by women was significantly more intensive than that reported by men (VAS of 5.98 ± 2.18 vs. VAS of 4.53 ± 1.98, P < 0.01). The NDI score before surgery was significantly higher in women than in men (NDI of 23.17 ± 8.12 vs. 18.92 ± 7.77, P = 0.02). The BDI score was also significantly higher in women (BDI of 10.5 ± 6.03 vs. 7.1 ± 4.68, P = 0.02). Table 1 shows statistically significant differences between patients with university or secondary school education and those who had completed vocational training or elementary school education only. Patients who had completed university or secondary school education had a significantly lower BMI and lower BDI scores and they reported less pain at 12 months postoperatively than patients with vocational or elementary school education only. Table 2 presents significant differences between those patients who were employed at the time of the study or were retired and those unemployed or drawing a disability pension. Patients who were employed at the time of the study or were retired demonstrated significantly lower NDI scores both before surgery and at 12 months postoperatively, as well as lower BDI scores compared to those who were unemployed or drew disability pensions. Factors such as age or BMI score did not exert a direct effect on treatment outcomes assessed as changes in the VAS and NDI scores in our study.
Statistically Significant Differences Between Employees Who Completed University or Secondary Education and Those Who Completed Vocational Training or Elementary School
| Variables | University or Secondary Education | Vocational Training or Elementary Education | P Value |
|---|---|---|---|
| VAS at 12 months | 2.05 ± 1.74 | 3.41 ± 2.31 | 0.02 |
| BMI | 24.29 ± 3.63 | 28.05 ± 5.22 | < 0.01 |
| Beck Depression Inventory | 7.47 ± 3.72 | 11.08 ± 6.36 | 0.02 |
Statistically Significant Differences Between Patients Who Were Employed or Retired and Those Who Were Unemployed or Drew a Disability Pension
| Variables | Employed or Retired | On Disability Pension or Unemployed | P Value |
|---|---|---|---|
| NDI before surgery | 21.01 ± 8.27 | 28.06 ± 6.95 | < 0.01 |
| NDI at 12 months | 11.57 ± 8.38 | 17.46 ± 10.46 | 0.02 |
| Beck Depression Inventory | 9.34 ± 5.37 | 13.18 ± 7.65 | 0.05 |
Education status of study group patients
Employment status of study group patients
The mean VAS scores at specific follow-up time points. The mean change after 12 months was 2.84 ± 2.77, median: 3
The mean NDI scores at specific follow-up time points. The mean NDI change after 12 months was 11.16 ± 9.52, median: 11
BMI of study group patients
History of depressive episodes within one month preceding the surgery in the study group
4. Discussion
Surgical treatment of cervical spine disc disease reduces pain and improves the quality of life (1). The result of treatment is not only dependent on technical issues and postoperative care. Comorbidities, social factors, pre-operative pain intensity, and the presence of worker compensation claims can all potentially affect the clinical outcomes (2-7). There are several large, multicenter studies investigating preoperative factors affecting the outcome in patients having anterior cervical discectomy and fusion. To find out which patients will most likely have a favorable response to surgery, it is important to know which preoperative factors influence the good treatment results. In our daily practice, we work with a diverse patient population and encounter a variety of responses to treatment. Most patients are operated on according to the same procedure and their postoperative care is conducted in the same manner. At the same time, treatment outcomes and patient-reported symptoms can vary widely. Not uncommonly, self-employed university graduates who want to resume their work quickly after the hiatus due to their illness recover very rapidly to a level where they are able to resume the work. During follow-up visits, such patients report improved quality of life and less pain. On the other hand, patients receiving or seeking to receive a disability pension report persistent pain and other symptoms adversely affecting their quality of life, despite objective evidence of a good treatment outcome, hoping to prolong their medical leave of absence from work and/or to obtain from their doctors various certificates confirming their health condition with a view to obtaining or extending the duration of their state-paid disability pensions. There are also patients who press for surgery at all costs despite the absence of clear indications for operative intervention. Their motivation is that undergoing surgery will boost their chances of obtaining a disability pension. These patients have often completed only the basic education and are not in stable employment. In this paper, data related to non-clinical variables were collated and analyzed statistically with the aim of confirming our daily clinical observations. Patients who had completed university or secondary school had a significantly lower BMI and lower BDI scores and reported less pain at 12 months postoperatively than patients with vocational or elementary school education only. Patients employed at the time of the study or retired demonstrated significantly lower NDI scores both before surgery and at 12 months postoperatively, as well as lower BDI scores compared to those who were unemployed or drew disability pensions. Factors such as age or BMI score did not exert a direct effect on treatment outcomes assessed as changes in the VAS and NDI scores. A literature review on lumbar spine surgery indicated that patients with worker compensation claims have less successful clinical results (8-13). Regarding the cervical spine, different conclusions were obtained (14-18). Anderson et al. (19) found that the presence of worker compensation claims and a history of using weak narcotics were negative predictors of clinical success. A higher preoperative NDI score, indicating a greater disability, was a positive predicting factor. In stepwise regression analysis, significant positive factors for NDI success were older age, higher initial NDI, and gainful employment whereas negative factors were litigation and employee compensation. Goldberg et al. (14), however, reported that employee compensation claims did not adversely influence the functional outcome of ACDF. At the same time, they emphasized that the right choice of patients is a key factor in determining functional outcomes, with over 80% of good to excellent results if the pathology, radiological changes, and clinical presentation correlated. Peolsson et al. (20) performed an analysis of over 100 patients with radiculopathy treated by ACDF. Among many elements examined, they stated that older patient age was a predictor of good pain relief. However, Bhandari et al. (6) found that advanced age was a negative factor for return to work after cervical stabilization. Shiban et al. (21) reported that younger age was the most influential factor associated with a better outcome after ACDF. This result remains in line with others’ results that also found younger patients have advantageous clinical outcomes (22-24). Unlike other studies, in their study, they found no association between gender and clinical outcomes. Other studies have found being male is associated with better outcomes after ACDF (5, 25). This was related to the greater endurance of the neck muscles in men (26). Peolsson et al. (4) evaluated 80 patients before cervical spine surgery with the distress and risk assessment instrument, which evaluates depression and somatization. They found that a normal distress and risk assessment result was the most important factor for a low NDI score at follow-up.
4.1. Conclusion
Cervical discectomy with interbody fusion for the cervical disc disease reduces pain and improves patients’ quality of life. Treatment outcomes are also influenced by social factors and patients’ emotional status. Understanding the importance of preoperative factors in functional outcomes can help establish realistic expectations. Patient selection is a key factor in determining functional outcomes, with good results if the pathology, clinical presentation, and radiological changes correlate.
References
-
1.
Godlewski B, Stachura MK, Czepko RA, Banach M, Czepko R. Analysis of changes in cervical spinal curvature and intervertebral disk space height following ACDF surgery in a group of 100 patients followed up for 12 months. J Clin Neurosci. 2018;52:92-9. [PubMed ID: 29656879]. https://doi.org/10.1016/j.jocn.2018.04.005.
-
2.
Hendriks EJ, Scholten-Peeters GG, van der Windt DA, Neeleman-van der Steen CW, Oostendorp RA, Verhagen AP. Prognostic factors for poor recovery in acute whiplash patients. Pain. 2005;114(3):408-16. [PubMed ID: 15777866]. https://doi.org/10.1016/j.pain.2005.01.006.
-
3.
Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Physical and psychological factors predict outcome following whiplash injury. Pain. 2005;114(1-2):141-8. [PubMed ID: 15733639]. https://doi.org/10.1016/j.pain.2004.12.005.
-
4.
Peolsson A, Vavruch L, Oberg B. Predictive factors for arm pain, neck pain, neck specific disability and health after anterior cervical decompression and fusion. Acta Neurochir (Wien). 2006;148(2):167-73. [PubMed ID: 16341632]. https://doi.org/10.1007/s00701-005-0660-x.
-
5.
Peolsson A, Peolsson M. Predictive factors for long-term outcome of anterior cervical decompression and fusion: A multivariate data analysis. Eur Spine J. 2008;17(3):406-14. [PubMed ID: 18084782]. [PubMed Central ID: PMC2270379]. https://doi.org/10.1007/s00586-007-0560-2.
-
6.
Bhandari M, Louw D, Reddy K. Predictors of return to work after anterior cervical discectomy. J Spinal Disord. 1999;12(2):94-8. [PubMed ID: 10229520].
-
7.
Jodicke A, Daentzer D, Kastner S, Asamoto S, Boker DK. Risk factors for outcome and complications of dorsal foraminotomy in cervical disc herniation. Surg Neurol. 2003;60(2):124-9. discussion 129-30. [PubMed ID: 12900115]. https://doi.org/10.1016/s0090-3019(03)00267-2.
-
8.
Bigos SJ, Spengler DM, Martin NA, Zeh J, Fisher L, Nachemson A. Back injuries in industry: A retrospective study. III. Employee-related factors. Spine (Phila Pa 1976). 1986;11(3):252-6. [PubMed ID: 2940709].
-
9.
Franklin GM, Haug J, Heyer NJ, McKeefrey SP, Picciano JF. Outcome of lumbar fusion in Washington State workers' compensation. Spine (Phila Pa 1976). 1994;19(17):1897-903. discussion 1904. [PubMed ID: 7997921]. https://doi.org/10.1097/00007632-199409000-00005.
-
10.
Greenough CG, Fraser RD. The effects of compensation on recovery from low-back injury. Spine (Phila Pa 1976). 1989;14(9):947-55. [PubMed ID: 2528824].
-
11.
Greenwood J Jr, McGuire TH, Kimbell F. A study of the causes of failure in the herniated intervertebral disc operation: An analysis of sixty-seven reoperated cases. J Neurosurg. 1952;9(1):15-20. [PubMed ID: 14908634]. https://doi.org/10.3171/jns.1952.9.1.0015.
-
12.
Junge A, Dvorak J, Ahrens S. Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine (Phila Pa 1976). 1995;20(4):460-8. [PubMed ID: 7747230].
-
13.
Young JN, Shaffrey CI, Laws ER Jr, Lovell LR. Lumbar disc surgery in a fixed compensation population: A model for influence of secondary gain on surgical outcome. Surg Neurol. 1997;48(6):552-8. discussion 558-9. [PubMed ID: 9400635].
-
14.
Goldberg EJ, Singh K, Van U, Garretson R, An HS. Comparing outcomes of anterior cervical discectomy and fusion in workman's versus non-workman's compensation population. Spine J. 2002;2(6):408-14. [PubMed ID: 14589262].
-
15.
Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75(9):1298-307. [PubMed ID: 8408151].
-
16.
Brodke DS, Zdeblick TA. Modified Smith-Robinson procedure for anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 1992;17(10 Suppl):S427-30. [PubMed ID: 1440038].
-
17.
White AA, Southwick WO, Deponte RJ, Gainor JW, Hardy R. Relief of pain by anterior cervical-spine fusion for spondylosis. A report of sixty-five patients. J Bone Joint Surg Am. 1973;55(3):525-34. [PubMed ID: 4703205]. https://doi.org/10.2106/00004623-197355030-00008.
-
18.
Davis RA. A long-term outcome study of 170 surgically treated patients with compressive cervical radiculopathy. Surg Neurol. 1996;46(6):523-30. discussion 530-3. [PubMed ID: 8956883].
-
19.
Anderson PA, Subach BR, Riew KD. Predictors of outcome after anterior cervical discectomy and fusion: A multivariate analysis. Spine (Phila Pa 1976). 2009;34(2):161-6. [PubMed ID: 19139666]. https://doi.org/10.1097/BRS.0b013e31819286ea.
-
20.
Peolsson A, Hedlund R, Vavruch L, Oberg B. Predictive factors for the outcome of anterior cervical decompression and fusion. Eur Spine J. 2003;12(3):274-80. [PubMed ID: 12687444]. [PubMed Central ID: PMC3615504]. https://doi.org/10.1007/s00586-003-0530-2.
-
21.
Shiban E, Gapon K, Wostrack M, Meyer B, Lehmberg J. Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir (Wien). 2016;158(2):349-55. [PubMed ID: 26620448]. https://doi.org/10.1007/s00701-015-2630-2.
-
22.
Chagas H, Domingues F, Aversa A, Vidal Fonseca AL, de Souza JM. Cervical spondylotic myelopathy: 10 years of prospective outcome analysis of anterior decompression and fusion. Surg Neurol. 2005;64 Suppl 1:S1:30-5. discussion S1:35-6. [PubMed ID: 15967227]. https://doi.org/10.1016/j.surneu.2005.02.016.
-
23.
Fujiwara K, Yonenobu K, Ebara S, Yamashita K, Ono K. The prognosis of surgery for cervical compression myelopathy. An analysis of the factors involved. J Bone Joint Surg Br. 1989;71(3):393-8. [PubMed ID: 2722928].
-
24.
Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C. Cervical spondylotic myelopathy: Surgical results and factors affecting prognosis. Neurosurgery. 1998;43(1):43-9. discussion 49-50. [PubMed ID: 9657187].
-
25.
Hermansen A, Hedlund R, Vavruch L, Peolsson A. Positive predictive factors and subgroup analysis of clinically relevant improvement after anterior cervical decompression and fusion for cervical disc disease: A 10- to 13-year follow-up of a prospective randomized study: Clinical article. J Neurosurg Spine. 2013;19(4):403-11. [PubMed ID: 23909550]. https://doi.org/10.3171/2013.7.SPINE12843.
-
26.
Peolsson A, Almkvist C, Dahlberg C, Lindqvist S, Pettersson S. Age-and sex-specific reference values of a test of neck muscle endurance. J Manipulative Physiol Ther. 2007;30(3):171-7. [PubMed ID: 17416270]. https://doi.org/10.1016/j.jmpt.2007.01.008.