Abstract
Background:
Sacroiliac Joint Dysfunction (SIJD) is considered an origin of low-back pain. It can change the motor control strategy and postural control (PC).Objectives:
We aimed to find any probable differences in PC between subjects with and without SIJD and determine the effects of the pelvic belt (PB) on PC.Methods:
Thirty-eight subjects were assigned into two equal groups with and without SIJD. They started to walk from the place marked on a force plate for 10 seconds after hearing an auditory signal and performed three attempts for each foot. They repeated six more ones with PB. Raw data were imported to an excel software (version 2007) spreadsheet to calculate the reaction time (RT) and anticipatory postural adjustment (APA) as the components of PC.Results:
Our results showed a significant difference in RT between the SIJD-affected and non-affected sides (P = 0.035), but there was no significant difference in APA (P = 0.057). There were significant differences in RT and APAs between the control and SIJD-affected side groups (P = 0.001 and P = 0.010, respectively). The PB application showed a significant difference in RT and APAs of the SIJD-affected side (P = 0.001 and P = 0.047, respectively).Conclusions:
It seems pain could lead to the postural sway into instability and change the motor control strategy. The proprioception signals from the neuromuscular system of SIJ improved after PB. Therefore, PB, as a feasible tool, can be recommended for PC improvement.Keywords
Sacroiliac Joint Dysfunction Low-back Pain Postural Balance Pelvic Belt
1. Background
The sacroiliac joint (SIJ) is considered one of the main components involved in low-back, buttock, groin, or thigh pain in about 16 - 30% of patients who suffer from chronic low-back pain (LBP). It is also called non-specific low-back pain (1, 2). The SIJ has been proposed as the cause of mechanical LBP with a rate from 10% to 27% (1). However, systematic reviews on the prevalence and accuracy of SIJ interventions showed a variation from 10% to 60%, mainly due to variations in study designs (3). The two valid signs for labeling SIJ as a source of pain are unilateral tenderness and pain under the posterior superior iliac spine (PSIS) (2).
The SIJ is an important link between the upper and lower body segments. It transfers the whole upper extremity weight to lower limbs and also is a shock absorber during the heel strike (4). Another important role for SIJ is to transfer the ground reaction forces from lower limbs to the trunk (4). The integrated function and stability of SIJ are very crucial for playing a unique role in human body stability in daily activities, including walking. Form and force closures are two combined components to provide SIJ stability, also known as the self-locking mechanism. The former implies anatomical structure and function, while the latter represents the dynamic process. Force closure results from the muscular system that is reinforced by fascia and ligamentous structures (4-6). Based on many studies, inadequate muscular recruitment accompanied by sacroiliac joint dysfunction (SIJD) can result in SIJ instability (4, 7-9).
As known, SIJ instability triggers LBP, which can, in turn, change the motor control strategy. It is also introduced as one of the causes of motor control changes in CLBP (10). Therefore, all these consequences from SIJD can influence postural control. Postural control as part of motor control is described as “the ability to maintain the body’s center of gravity within the limits of stability as defined by the base of support” (11, 12). A reliable way for studying postural control is to quantify the movement of the center of pressure (COP) and then analyze the postural sway (12). Displacement of the center of mass (COM) and COP can cause postural adjustments (13). The integration of sensory information originating from visual, vestibular, and somatosensory systems is necessary for the accomplishment of postural control. The central nervous system (CNS) utilizes anticipatory postural adjustments (APAs) as a feedforward mechanism and compensatory postural adjustments as a feedback mechanism to overcome the effect of perturbations (13, 14). As known, APAs activate leg and trunk muscles before body perturbation. Thus, APAs control the position of COM and minimize the postural perturbations at the end (15). In other words, anticipatory reactions are launched by the individual, and then the CNS makes anticipatory corrections to predict postural perturbations. A group of studies suggested a complex relationship between LBP and APAs and decreased variability of APA onset latencies (16-18). Reaction time (RT) is the time interval from applying a stimulus to response, which could be increased in musculoskeletal disorders like LBP (19, 20).
Although many researchers have concentrated on restoring stability in LBP with physical therapy protocols, a handful of studies have dealt with SIJD (2, 21, 22). Some common effective interventions include mobilization, manipulation, modalities like ultrasound, transcutaneous electrical nerve stimulation, heat, orthoses like pelvic compression belt, and exercises (2, 4, 17). Among these procedures, mobilization, manipulation, and particularly the belt, among these procedures, can trigger the causes of SIJD, whereas the rest aims at relieving the symptoms (23, 24). Pelvic compression belt (PCB) plays as a pseudo-fascia and presses the underlying muscles (22). Besides, PCB increases the resultant force, facilitates neuromuscular function (25), and improves the self-locking mechanism. The positive effects of PCB have been shown on pain relief and improvement of the trunk and pelvic electromyographic activities (23, 24, 26).
2. Objectives
As mentioned earlier, there are scarce studies on analyzing the effects of PCB on postural control in SIJD as a subgroup of NLBP. Therefore, the objectives of this study, as part of our research to evaluate postural stability parameters, were: 1- To find any probable differences in postural responses between individuals with and without SIJD, 2- To investigate the effects of PCB on postural control variables, and 3- To compare the effects of PCB on the affected and non-affected sides in SIJD individuals.
3. Methods
3.1. Participants
All subjects were recruited from the outpatient physiotherapy clinics and the campus of Tehran University of Medical Sciences (TUMS). They were assigned into two groups. Group I contained 24 subjects with SIJD and pain for at least 12 weeks. The pain and tenderness were under the PSIS. However, five subjects were excluded from the study. Group II had 19 individuals (16 females, three males) without SIJD that were matched to the group I subjects for age, sex, weight, height, body mass index (BMI), physical activity scale (PAS), and the preferred leg. They were healthy according to their medical history, our examination, and clinical tests.
3.2. Inclusion and Exclusion Criteria
The inclusion criteria for the SIJD group included an age of 20 to 42 as the age range of physical activity, a pain around SIJ, buttock or groin lasting for at least 12 weeks, pain intensity of more than 30 on a 0 - 100 mm visual analog scale (VAS), tender SIJ on palpation, pelvic asymmetry, positive tests in four of six SIJ provocation tests, no severe residual back pain, no pregnancy, no history of more than two pregnancies, no other sacroiliac pathology, no ligament laxity, involving in no professional sports or exercises, and no lower limb malalignments. The provocation tests included a distraction test, compression test, FABER test, thigh thrust test, active straight leg raising, and Gaenslen’s maneuver.
The Ethics Committee of TUMS approved the study. Group II included 19 individuals with no history of SIJ pain, no pain during SIJ provocation tests, and no lumbar and pelvic region congenital abnormalities. The exclusion criteria for both groups were no tendency to continue the study at any stage. All subjects signed informed consent forms before the clinical examination. We asked each participant to fill out a general questionnaire with data on age, weight, height, gender, career, and education. A Persian version of the international physical activity questionnaire approved by Baghiani Moghaddam (27) was used to assess the PAS of all participants. We measured pain intensity by a 0 - 100 mm VAS for the SIJD group. Data were gathered at the Gait Laboratory, School of Rehabilitation, TUMS.
We applied two tests to find out the preferred leg (28). First, each participant stood in a steady position with feet approximately pelvic width apart. The examiner stood at the back while pushing forward gently the participant with both hands to step. Then, while the subject and the examiner were standing as described above, the participant walked after hearing the word “go”. The examiner monitored the initiating leg for walking. Each participant performed these two tests three times randomly. We counted the number of walking initiation for each leg to find out the preferred leg.
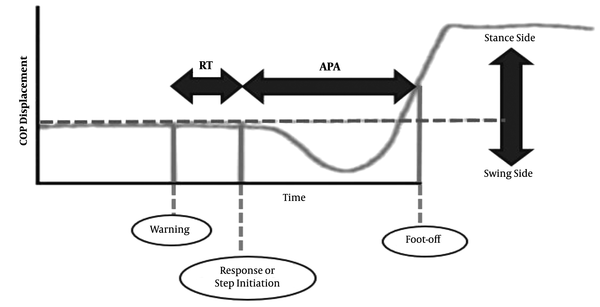
3.3. Procedures
Each participant stood barefoot on the marked places on a 9090 series Bertec force plate (90 × 90 cm dimension with 15.2 cm height) sampled and filtered on a frequency of 500 and 10 Hz, respectively. The examiner asked each participant to press the feet together and hang arms at sides with open eyes and straight head. Participants distributed their weights equally between their right and left feet. They looked at a red round marker (with a 2.5 cm radius) on the front wall with three meters distance leveled with their eyes. There were 10 s auditory signals with two beeps. The first one was a warning and the second one was a response for initiating walking, whereas the participant had no idea about the interval between these two beeps. Each beep lasted for 100 milliseconds (ms) with an intensity of 60 dB and a frequency of 2 kHz. The software programmed the sequence of these two beeps synchronizing with the recording force plate. The force plate started to record the data, and the participant heard the auditory signal 2000 ms later. We considered the 1500 ms period of that 2000 ms time to calculate the mean amplitude of the primary COP position before the auditory signal initiation (Figure 1). We used the COP trajectory to compute the timing of step initiation and foot-off. The first mediolateral shift of COP in the direction of the swing leg described step initiation (the mean amplitude during that 1500 ms was COP excursion > 3 SD away from the primary COP position). The end of the mediolateral shift of COP in the direction of the stance leg described foot-off (absolute COP slope < 100 mm/s in a row) (29, 30). We calculated the RT and APA phases from these two events (i.e., step initiation and foot-off). The duration from the first beep to step initiation was considered as RT. The duration from step initiation to foot-off was defined as APA (Figure 1).
The calculation of reaction time and anticipatory postural adjustments. The mediolateral shift of the center of pressure (COP) trajectory during gait initiation. The following items are shown in this figure: The first beep of the auditory signal as a warning, the first mediolateral shift of the COP in the direction of the swing leg (step initiation), and the end of the mediolateral shift of the COP in the direction of the stance leg (foot-off). RT: reaction time phase; APA: anticipatory postural adjustment phase.
All participants walked on their paces for 10 seconds with the selected foot. There was a one-minute rest after each attempt (31). They performed three attempts with each preferred and non-preferred leg randomly.
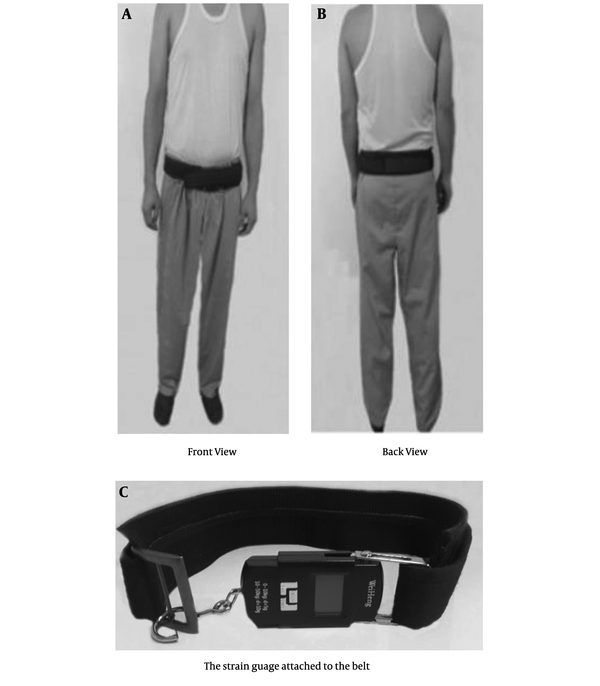
After a 15 min rest, the participants repeated six more attempts with a non-elastic, 10 centimeters width custom-made pelvic belt fastened with a load of 50 N positioning over two PSISs and under two anterior superior iliac spines while they felt comfortable or relieving pain (32). The load was measured with a strain gauge attached to the belt (Figure 2).
The pelvic belt and strain gauge position
3.4. Data Analysis
Raw data of each trial were imported to an excel software (version 2007) spreadsheet and converted into time points to calculate RT and APAs (Figure 1). We considered the mean value of three attempts for each leg for further analysis. The obtained data were analyzed statistically using the Statistical Package for Social Sciences (SPSS) version 17.00 software. The p values for statistical significance were set at 0.05. The Kolmogorov-Smirnov test showed a normal distribution for all data. An independent sample t-test was used to compare the demographic characteristics of the two groups. A paired-samples t-test was used to compare the mean values of RT and APAs within each group separately. For further analysis, one-way ANOVA was used for making comparisons between all groups.
4. Results
For more clarification, the results are presented in two sections.
4.1. Before Applying the Belt
4.1.1. Control Group
The mean values of the demographic characteristics of both groups are presented in Table 1. Table 2 represents the results of independent samples' t-test for age, weight, height, BMI, and PAS. There were no significant differences in all demographic characteristics and PAS between the two groups. Due to the presence of 12 individuals with right-preferred legs and seven individuals with left-preferred legs within the control group, a paired t-test was used to compare within the group. Table 3 indicates all the results obtained from paired samples t-test on RT and APAs of right, left, preferred, and non-preferred legs in the control group. There were no differences in RT and APAs between the right and left legs. The same was true for RT and APAS of the preferred and non-preferred legs in the control group. Therefore, we selected the preferred leg of the control group to compare with the affected and non-affected sides of SIJD.
Demographic Characteristics of Control and SIJD Groups
| Variables | SIJD Group (Mean ± SD) | Control Group (Mean ± SD) |
|---|---|---|
| Age (y) | 29.74 ± 7.62 | 28.74 ± 6.24 |
| Weight (kg) | 55.83 ± 7.17 | 60.73 ± 26.91 |
| Height (cm) | 163 ± 7.63 | 154 ± 25.91 |
| BMI | 20.98 ± 3.00 | 21.06 ± 2.42 |
| PAS | 2329.83 ± 1801.94 | 1526.30 ± 1214.95 |
| VAS (0-100 mm) | 50 ± 13.642 | 0 |
| Pain Duration (mo) | 14 ± 7.141 | 0 |
Independent t-Test of Demographic Characteristics of SIJD and Control Groups
| Variables | Independent Samples Test | ||||
|---|---|---|---|---|---|
| t | F | Std. Error Difference | Mean Difference | P-Value | |
| Age | -0.442 | 1.068 | 2.262 | -1.000 | 0.661 |
| Height | -1.443 | 1.155 | 6.198 | -8.9473 | 0.158 |
| Weight | 0.767 | 1.171 | 6.389 | 4.9000 | 0.448 |
| BMI | 0.949 | 0.088 | 0.885 | 0.0778 | 0.930 |
| PAS | -1.612 | 7.689 | 498.58 | -803.5326 | 0.116 |
Paired t-Test of Reaction Time and Anticipatory Postural Adjustments Before and After Belt in Control and SIJD Groups Separately
| Paired Variables | Std. Deviation | Std. Error Mean | t | Sig. (2-Tailed) |
|---|---|---|---|---|
| RTRm - RTLm | 0.041566 | 0.00953 | -1.897 | 0.074 |
| APARm - APALm | 0.093970 | 0.02155 | -0.761 | 0.457 |
| RTPm - RTNonPm | 0.042632 | 0.00978 | -1.591 | 0.129 |
| APAPm - APANonPm | 0.080646 | 0.01850 | -0.620 | 0.543 |
| RTAff - RTnonAff | 0.077265 | 0.017726 | 2.283 | 0.035 a |
| APAAff - APAnonAff | 0.086064 | 0.019744 | -2.034 | 0.057 |
| RTP - RTBP | 0.055253 | 0.012676 | 0.32018 | 0.753 |
| APAP - APABP | 0.069113 | 0.15856 | 0.26918 | 0.791 |
| RTBAff - RTBnonAff | 0.051982 | 0.011925 | -0.22918 | 0.821 |
| RTAff - RTBAff | 0.082805 | 0.018997 | 3.898 | 0.001a |
| RTnonAff - RTBnonAff | 0.083286 | 0.019107 | 1.614 | 0.124 |
| APABAff - APABnonAff | 0.099203 | 0.22759 | 0.167 | 0.870 |
| APAAff - APABAff | 0.112813 | 0.025881 | -2.129 | 0.047 a |
| APAnonAff - APABnonAff | 0.067293 | 0.015438 | -0.722 | 0.480 |
4.1.2. SIJD Group
Table 3 indicates all the results obtained from the paired samples t-test on RT and APAs of the affected and non-affected sides in the SIJD group. There was a significant difference in RT between the affected and non-affected sides. Although there was a difference in APAs between the affected and non-affected sides, it was not statistically significant.
4.1.3. Comparison Between Two Groups
The results of the ANOVA test for three control, SIJD affected side, and SIJD non-affected side groups are shown in Table 4. Our findings showed a significant difference in RT between the control and SIJD affected side groups, but there was no difference between the control and SIJD non-affected side groups. However, there was a difference in APAs between the control and SIJD affected side groups. We did not find any difference in APAs between the control and SIJD non-affected side groups.
The Analysis of Variance Test of Reaction Time and Anticipatory Postural Adjustments of Control Group, Sacroiliac Joint Dysfunction-affected Side Group, and Sacroiliac Joint Dysfunction-non-affected Side Group a
| Dependent Variables | Groups | Mean Difference | Std. Error | Sig. | |
|---|---|---|---|---|---|
| RT | Control | SIJD-non-affected side | -0.034368 | 0.020751 | 0.103 |
| SIJD-affected side | -0.074842 | 0.020751 | 0.001 | ||
| APA | Control | SIJD-non-affected side | 0.014305 | 0.020442 | 0.487 |
| SIJD-affected side | 0.054474 | 0.020442 | 0.010 | ||
| RTB | Control | SIJD-non-affected side | -0.004842 | 0.013254 | 0.716 |
| SIJD-affected side | -0.007579 | 0.013254 | 0.570 | ||
| APAB | Control | SIJD-non-affected side | -0.001105 | 0.018277 | 0.952 |
| SIJD-affected side | -0.004895 | 0.018277 | 0.790 | ||
4.2. After Applying Belt
Table 4 indicates all the results of paired t-test on RT and APAs for three control, SIJD affected side, and SIJD non-affected side groups after applying PCB
5. Discussion
There is a handful of evidence regarding the physical therapy protocols for the management of SIJD. To the best of our knowledge, the postural stability parameters such as RT and APAs had not been studied in SIJD patients in previous studies. Therefore, in the current research, we investigated the temporal domain of postural stability in normal and SIJD individuals and the plausible effects of the belt on the self-locking mechanism in SIJ individuals. We present our discussion in two parts, as follows:
5.1. Before Intervention
Following our results, SIJD individuals showed lower values of APAs at the affected side before any interventions. As there were no similar studies in the literature, we could only compare the current results with those studies reported for CLBP (12, 16, 20, 33-35). Some of these studies reported increased postural sway while a few ones showed smaller postural sway for the CLBP group. There were no methodological differences that could clarify these differences (34). Hence, our results are in line with those reporting lower values of APAs in CLBP individuals (33, 34). Many researchers have reported that any deficit in muscular and neural elements has been associated with reduced postural stability in the LBP group (20). This was due to taking the strategy of trunk stiffening as a protective mechanism for balance maintenance (26). Many bodies of research have shown the adverse effects of pain on muscles around the affected area. In turn, the affected postural stability changes the motor control strategy (10, 36-38). As it had been shown in CLBP, there were improper muscle recruitment and incorrect proprioception function (39-41). Therefore, one could conclude similar changes in SIJD individuals.
The specified innervation and unique structure of SIJ could confirm this suggestion (5, 25). In this respect, we suggest that any disturbances in proprioception (as one of the sources of gathering information) can affect motor control as one of the components of postural stability (37, 38). In turn, the impairment of the proprioception system could lead to the postural sway into instability (42, 43). Consequently, SIJD patients might compensate for the disturbance through increased stiffness of trunk muscles, resulting in changing APAs.
As mentioned, so far, no research has studied the RT in SIJD individuals. Therefore, similarly, we only compare our data with those for LBP. Our results showed longer RT at the affected side of SIJD individuals that is in line with LBP studies (12, 20, 44, 45) in which a longer RT was shown in LBP individuals. However, the present study was contrary to Macrae et al. (46). The reason for this difference was due to methodological variations in other studies (12). Once again, one might conclude that the resultant pain and impairment of the proprioception system may result in postural instability (37, 38, 42, 43).
5.2. After Intervention
Our results showed the positive effects of the pelvic belt on RT and APAs of the affected side in SIJD. In this regard, many studies have provided evidence regarding the positive effects of a belt on the relief of pain, improvement of muscle activity, and resultant neuromuscular function (4, 23, 24, 26, 47, 48). As known, the pain was among the most important factors impairing motor control. Furthermore, there is substantial evidence showing proprioception impairment in people with pains originating from the vertebrae (49). The severity of pain and thus proprioception signals from the neuromuscular system of SIJ improved with the belt (23, 24, 26).
Based on the current findings, the SIJD group showed reduced RT and increased APAs after the pelvic belt application. This result might represent the role of the pelvic belt as a feasible and cost-effective tool for the improvement of postural control parameters. The positive effects of the belt on postural stability in the SIJD group were consistent with Munoz et al., Boucher et al., and Ghofrani et al. (50-52) studies that used a lumbar belt for CLBP patients. In contrast with the SIJD group, we saw no changes in postural control parameters in the control group as a normal group.
In brief, the SIJD group represented more RT and fewer APA values than the control group. The pelvic belt reduced RT and increased APAs significantly. Therefore, SIJD individuals can use PB to benefit from the positive effects of the belt on pain relief and, thus, postural control improvement.
There were some limitations to this study. First, fewer males participated in our study. Then, we could not compare the differences between male and female subjects. Second, all SIJD individuals, except one, had pain at the preferred side. It is suggested that future studies include male individuals and SIJD at the non-preferred side.
5.3. Conclusion
According to the international association for the study of pain, the first step to relieve the SIJ pain is to use a conservative procedure (53). Therefore, using a pelvic belt, as a conservative procedure, can be recommended for both pain relief and postural control improvement.
Acknowledgements
References
-
1.
Simopoulos TT, Manchikanti L, Singh V, Gupta S, Hameed H, Diwan S, et al. A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions. Pain Physician. 2012;15(3):E305-44. [PubMed ID: 22622915].
-
2.
Al-Subahi M, Alayat M, Alshehri MA, Helal O, Alhasan H, Alalawi A, et al. The effectiveness of physiotherapy interventions for sacroiliac joint dysfunction: a systematic review. J Phys Ther Sci. 2017;29(9):1689-94. [PubMed ID: 28932014]. [PubMed Central ID: PMC5599847]. https://doi.org/10.1589/jpts.29.1689.
-
3.
Simopoulos TT, Manchikanti L, Gupta S, Aydin SM, Kim CH, Solanki D, et al. Systematic review of the diagnostic accuracy and therapeutic effectiveness of sacroiliac joint interventions. Pain Physician. 2015;18(5):E713-56. [PubMed ID: 26431129].
-
4.
Hamidi-Ravari B, Tafazoli S, Chen H, Perret D. Diagnosis and current treatments for sacroiliac joint dysfunction: A review. Curr Phys Med Rehabil Rep. 2014;2(1):48-54. https://doi.org/10.1007/s40141-013-0037-7.
-
5.
Vleeming A, Volkers AC, Snijders CJ, Stoeckart R. Relation between form and function in the sacroiliac joint. Part II: Biomechanical aspects. Spine (Phila Pa 1976). 1990;15(2):133-6. [PubMed ID: 2326707]. https://doi.org/10.1097/00007632-199002000-00017.
-
6.
Hossain M, Nokes LD. A model of dynamic sacro-iliac joint instability from malrecruitment of gluteus maximus and biceps femoris muscles resulting in low back pain. Med Hypotheses. 2005;65(2):278-81. [PubMed ID: 15922100]. https://doi.org/10.1016/j.mehy.2005.02.035.
-
7.
van Wingerden JP, Vleeming A, Snijders CJ, Stoeckart R. A functional-anatomical approach to the spine-pelvis mechanism: interaction between the biceps femoris muscle and the sacrotuberous ligament. Eur Spine J. 1993;2(3):140-4. [PubMed ID: 20058466]. https://doi.org/10.1007/BF00301411.
-
8.
Hungerford B, Gilleard W, Hodges P. Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine (Phila Pa 1976). 2003;28(14):1593-600. [PubMed ID: 12865851].
-
9.
Shadmehr A, Jafarian Z, Talebian S. Changes in recruitment of pelvic stabilizer muscles in people with and without sacroiliac joint pain during the active straight-leg-raise test. J Back Musculoskelet Rehabil. 2012;25(1):27-32. [PubMed ID: 22398264]. https://doi.org/10.3233/BMR-2012-0307.
-
10.
Hodges PW, Tucker K. Moving differently in pain: a new theory to explain the adaptation to pain. Pain. 2011;152(3 Suppl):S90-8. [PubMed ID: 21087823]. https://doi.org/10.1016/j.pain.2010.10.020.
-
11.
Thakkar H, E S. Static and dynamic postural stability in subjects with and without chronic low back pain. Int J Res Med Sci. 2015:2405-9. https://doi.org/10.18203/2320-6012.ijrms20150639.
-
12.
Kiers H, van Dieen JH, Brumagne S, Vanhees L. Postural sway and integration of proprioceptive signals in subjects with LBP. Hum Mov Sci. 2015;39:109-20. [PubMed ID: 25436915]. https://doi.org/10.1016/j.humov.2014.05.011.
-
13.
Santos MJ, Kanekar N, Aruin AS. The role of anticipatory postural adjustments in compensatory control of posture: 2. Biomechanical analysis. J Electromyogr Kinesiol. 2010;20(3):398-405. [PubMed ID: 20156693]. [PubMed Central ID: PMC2859839]. https://doi.org/10.1016/j.jelekin.2010.01.002.
-
14.
Aruin AS. Enhancing anticipatory postural adjustments: A novel approach to balance rehabilitation. J Nov Physiother. 2016;6(2). [PubMed ID: 27335705]. [PubMed Central ID: PMC4913780]. https://doi.org/10.4172/2165-7025.1000e144.
-
15.
Knox MF, Chipchase LS, Schabrun SM, Marshall PW. Anticipatory and compensatory postural adjustments in people with low back pain: a protocol for a systematic review and meta-analysis. Syst Rev. 2016;5:62. [PubMed ID: 27084681]. [PubMed Central ID: PMC4833897]. https://doi.org/10.1186/s13643-016-0242-4.
-
16.
Jacobs JV, Lyman CA, Hitt JR, Henry SM. Task-related and person-related variables influence the effect of low back pain on anticipatory postural adjustments. Hum Mov Sci. 2017;54:210-9. [PubMed ID: 28527423]. [PubMed Central ID: PMC5522366]. https://doi.org/10.1016/j.humov.2017.05.007.
-
17.
Shearar KA, Colloca CJ, White HL. A randomized clinical trial of manual versus mechanical force manipulation in the treatment of sacroiliac joint syndrome. J Manipulative Physiol Ther. 2005;28(7):493-501. [PubMed ID: 16182023]. https://doi.org/10.1016/j.jmpt.2005.07.006.
-
18.
Ferreira ML, Ferreira PH, Hodges PW. Changes in postural activity of the trunk muscles following spinal manipulative therapy. Man Ther. 2007;12(3):240-8. [PubMed ID: 17452118]. https://doi.org/10.1016/j.math.2006.06.015.
-
19.
Sung PS, Danial P. Trunk reaction time and kinematic changes following slip perturbations in subjects with recurrent low back pain. Ann Biomed Eng. 2018;46(3):488-97. [PubMed ID: 29372435]. https://doi.org/10.1007/s10439-017-1972-8.
-
20.
Etemadi Y, Salavati M, Arab AM, Ghanavati T. Balance recovery reactions in individuals with recurrent nonspecific low back pain: Effect of attention. Gait Posture. 2016;44:123-7. [PubMed ID: 27004644]. https://doi.org/10.1016/j.gaitpost.2015.11.017.
-
21.
Shipton EA. Physical therapy approaches in the treatment of low back pain. Pain Ther. 2018;7(2):127-37. [PubMed ID: 30229473]. [PubMed Central ID: PMC6251828]. https://doi.org/10.1007/s40122-018-0105-x.
-
22.
van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J. 2011;20(1):19-39. [PubMed ID: 20640863]. [PubMed Central ID: PMC3036018]. https://doi.org/10.1007/s00586-010-1518-3.
-
23.
Hammer N, Mobius R, Schleifenbaum S, Hammer KH, Klima S, Lange JS, et al. Pelvic belt effects on health outcomes and functional parameters of patients with sacroiliac joint pain. PLoS One. 2015;10(8). e0136375. [PubMed ID: 26305790]. [PubMed Central ID: PMC4549265]. https://doi.org/10.1371/journal.pone.0136375.
-
24.
Jung HS, Jeon HS, Oh DW, Kwon OY. Effect of the pelvic compression belt on the hip extensor activation patterns of sacroiliac joint pain patients during one-leg standing: a pilot study. Man Ther. 2013;18(2):143-8. [PubMed ID: 23111368]. https://doi.org/10.1016/j.math.2012.09.003.
-
25.
Arumugam A, Milosavljevic S, Woodley S, Sole G. Effects of external pelvic compression on form closure, force closure, and neuromotor control of the lumbopelvic spine--a systematic review. Man Ther. 2012;17(4):275-84. [PubMed ID: 22386280]. https://doi.org/10.1016/j.math.2012.01.010.
-
26.
Soisson O, Lube J, Germano A, Hammer KH, Josten C, Sichting F, et al. Pelvic belt effects on pelvic morphometry, muscle activity and body balance in patients with sacroiliac joint dysfunction. PLoS One. 2015;10(3). e0116739. [PubMed ID: 25781325]. [PubMed Central ID: PMC4364533]. https://doi.org/10.1371/journal.pone.0116739.
-
27.
Moghaddam MB, Aghdam FB, Jafarabadi MA, Allahverdipour H, Nikookheslat SD, Safarpour S. The Iranian Version of International Physical Activity Questionnaire (IPAQ) in Iran: content and construct validity, factor structure, internal consistency and stability. World Appl Sci J. 2012;18(8):1073-80.
-
28.
Claeys K, Brumagne S, Dankaerts W, Kiers H, Janssens L. Decreased variability in postural control strategies in young people with non-specific low back pain is associated with altered proprioceptive reweighting. Eur J Appl Physiol. 2011;111(1):115-23. [PubMed ID: 20824281]. https://doi.org/10.1007/s00421-010-1637-x.
-
29.
Martinez-Mendez R, Sekine M, Tamura T. Detection of anticipatory postural adjustments prior to gait initiation using inertial wearable sensors. J Neuroeng Rehabil. 2011;8:17. [PubMed ID: 21470394]. [PubMed Central ID: PMC3079618]. https://doi.org/10.1186/1743-0003-8-17.
-
30.
Uemura K, Yamada M, Nagai K, Tanaka B, Mori S, Ichihashi N. Fear of falling is associated with prolonged anticipatory postural adjustment during gait initiation under dual-task conditions in older adults. Gait Posture. 2012;35(2):282-6. [PubMed ID: 22024142]. https://doi.org/10.1016/j.gaitpost.2011.09.100.
-
31.
Salavati M, Hadian MR, Mazaheri M, Negahban H, Ebrahimi I, Talebian S, et al. Test-retest reliability [corrected] of center of pressure measures of postural stability during quiet standing in a group with musculoskeletal disorders consisting of low back pain, anterior cruciate ligament injury and functional ankle instability. Gait Posture. 2009;29(3):460-4. [PubMed ID: 19167891]. https://doi.org/10.1016/j.gaitpost.2008.11.016.
-
32.
Shadmehr A, Jafarian Z, Tavakol K, Talebian S. Effect of pelvic compression on the stability of pelvis and relief of sacroiliac joint pain in women: A case series. J Musculoskelet Pain. 2013;21(1):31-6. https://doi.org/10.3109/10582452.2013.763395.
-
33.
Brumagne S, Janssens L, Knapen S, Claeys K, Suuden-Johanson E. Persons with recurrent low back pain exhibit a rigid postural control strategy. Eur Spine J. 2008;17(9):1177-84. [PubMed ID: 18594876]. [PubMed Central ID: PMC2527415]. https://doi.org/10.1007/s00586-008-0709-7.
-
34.
Mazaheri M, Coenen P, Parnianpour M, Kiers H, van Dieen JH. Low back pain and postural sway during quiet standing with and without sensory manipulation: a systematic review. Gait Posture. 2013;37(1):12-22. [PubMed ID: 22796243]. https://doi.org/10.1016/j.gaitpost.2012.06.013.
-
35.
Lomond KV, Jacobs JV, Hitt JR, DeSarno MJ, Bunn JY, Henry SM. Effects of low back pain stabilization or movement system impairment treatments on voluntary postural adjustments: a randomized controlled trial. Spine J. 2015;15(4):596-606. [PubMed ID: 25452017]. [PubMed Central ID: PMC4375040]. https://doi.org/10.1016/j.spinee.2014.10.020.
-
36.
Yang J, Lee B, Kim C. Changes in proprioception and pain in patients with neck pain after upper thoracic manipulation. J Phys Ther Sci. 2015;27(3):795-8. [PubMed ID: 25931733]. [PubMed Central ID: PMC4395717]. https://doi.org/10.1589/jpts.27.795.
-
37.
Brumagne S, Cordo P, Verschueren S. Proprioceptive weighting changes in persons with low back pain and elderly persons during upright standing. Neurosci Lett. 2004;366(1):63-6. [PubMed ID: 15265591]. https://doi.org/10.1016/j.neulet.2004.05.013.
-
38.
Sung W, Abraham M, Plastaras C, Silfies SP. Trunk motor control deficits in acute and subacute low back pain are not associated with pain or fear of movement. Spine J. 2015;15(8):1772-82. [PubMed ID: 25862508]. [PubMed Central ID: PMC4516579]. https://doi.org/10.1016/j.spinee.2015.04.010.
-
39.
Gill KP, Callaghan MJ. The measurement of lumbar proprioception in individuals with and without low back pain. Spine (Phila Pa 1976). 1998;23(3):371-7. [PubMed ID: 9507628]. https://doi.org/10.1097/00007632-199802010-00017.
-
40.
della Volpe R, Popa T, Ginanneschi F, Spidalieri R, Mazzocchio R, Rossi A. Changes in coordination of postural control during dynamic stance in chronic low back pain patients. Gait Posture. 2006;24(3):349-55. [PubMed ID: 16311036]. https://doi.org/10.1016/j.gaitpost.2005.10.009.
-
41.
O'Sullivan PB, Burnett A, Floyd AN, Gadsdon K, Logiudice J, Miller D, et al. Lumbar repositioning deficit in a specific low back pain population. Spine (Phila Pa 1976). 2003;28(10):1074-9. [PubMed ID: 12768152]. https://doi.org/10.1097/01.BRS.0000061990.56113.6F.
-
42.
Craig CE, Goble DJ, Doumas M. Proprioceptive acuity predicts muscle co-contraction of the tibialis anterior and gastrocnemius medialis in older adults' dynamic postural control. Neuroscience. 2016;322:251-61. [PubMed ID: 26905952]. https://doi.org/10.1016/j.neuroscience.2016.02.036.
-
43.
Toosizadeh N, Ehsani H, Miramonte M, Mohler J. Proprioceptive impairments in high fall risk older adults: the effect of mechanical calf vibration on postural balance. Biomed Eng Online. 2018;17(1):51. [PubMed ID: 29716599]. [PubMed Central ID: PMC5930964]. https://doi.org/10.1186/s12938-018-0482-8.
-
44.
Henry SM, Hitt JR, Jones SL, Bunn JY. Decreased limits of stability in response to postural perturbations in subjects with low back pain. Clin Biomech (Bristol, Avon). 2006;21(9):881-92. [PubMed ID: 16806618]. https://doi.org/10.1016/j.clinbiomech.2006.04.016.
-
45.
Luoto S, Taimela S, Hurri H, Aalto H, Pyykko I, Alaranta H. Psychomotor speed and postural control in chronic low back pain patients A controlled follow-up study. Spine (Phila Pa 1976). 1996;21(22):2621-7. [PubMed ID: 8961450]. https://doi.org/10.1097/00007632-199611150-00012.
-
46.
MacRae CS, Critchley D, Lewis JS, Shortland A. Comparison of standing postural control and gait parameters in people with and without chronic low back pain: a cross-sectional case-control study. BMJ Open Sport Exerc Med. 2018;4(1). e000286. [PubMed ID: 29387444]. [PubMed Central ID: PMC5783032]. https://doi.org/10.1136/bmjsem-2017-000286.
-
47.
Park KM, Kim SY, Oh DW. Effects of the pelvic compression belt on gluteus medius, quadratus lumborum, and lumbar multifidus activities during side-lying hip abduction. J Electromyogr Kinesiol. 2010;20(6):1141-5. [PubMed ID: 20646935]. https://doi.org/10.1016/j.jelekin.2010.05.009.
-
48.
Pel JJ, Spoor CW, Goossens RH, Pool-Goudzwaard AL. Biomechanical model study of pelvic belt influence on muscle and ligament forces. J Biomech. 2008;41(9):1878-84. [PubMed ID: 18501363]. https://doi.org/10.1016/j.jbiomech.2008.04.002.
-
49.
Scheermesser M, Bachmann S, Schamann A, Oesch P, Kool J. A qualitative study on the role of cultural background in patients' perspectives on rehabilitation. BMC Musculoskelet Disord. 2012;13:5. [PubMed ID: 22269636]. [PubMed Central ID: PMC3398320]. https://doi.org/10.1186/1471-2474-13-5.
-
50.
Munoz F, Salmochi JF, Faouen P, Rougier P. Low back pain sufferers: is standing postural balance facilitated by a lordotic lumbar brace? Orthop Traumatol Surg Res. 2010;96(4):362-6. [PubMed ID: 20452305]. https://doi.org/10.1016/j.otsr.2010.01.003.
-
51.
Boucher JA, Roy N, Preuss R, Lariviere C. The effect of two lumbar belt designs on trunk repositioning sense in people with and without low back pain. Ann Phys Rehabil Med. 2017;60(5):306-11. [PubMed ID: 28461129]. https://doi.org/10.1016/j.rehab.2017.03.002.
-
52.
Masoud G, Gholamreza O, Saeed T, Hossein B, Kazem M, Shiva M. Research paper: Immediate effects of lumbosacral belt on postural control during challenging tasks in patients with chronic low back pain . J Mod Rehabil. 2017;11(2).
-
53.
Merskey H. Description of chronic pain syndromes and definitions of pain terms. Classification of Chronic Pain. 2nd ed. Seattle, WA: IASP Press; 1994.
