1. Background
Adolescent Idiopathic Scoliosis (AIS) is a 3-dimensional deformity occurring simultaneously in coronal, sagittal, and axial planes. Sagittal imbalance, in addition to coronal deviation and axial rotation, has been well-documented in patients with AIS (1, 2). As proposed in lenke classification, the thoracic sagittal profile can be grouped into three patterns of hypokyphosis (thoracic kyphosis (TK) < 10), hyperkyphosis (TK > 40), and thoracic kyphosis, in which a degree between 10 - 40 is considered normal (3). Several intraoperative maneuvers - each with its own merits and demerits - have been suggested by the literature for a surgical correction of AIS (4, 5). Since the introduction of posterior instrumentation and cotrel-dubousset (CD) techniques, major developments have occurred regarding the reconstruction of spine surgery, representing important medical milestones (6).
The reduction maneuvering techniques of AIS, direct vertebral rotation (DVR), and cantilever (CR) have been widely used by surgeons over the past decades due to their ease of use and widespread availabilities (7, 8). Although DVR and CR have produced satisfactory outcomes regarding the deformity correction of a coronal plane, some studies have documented their negative effects on the sagittal profile of, especially, patients with hypokyphosis (4, 9). The posteromedial translation technique, which is one of the earliest maneuvering techniques for correcting scoliosis, has proven to be an optimum intraoperative measure for improving the sagittal profile in patients with hypokyphosis while achieving favorable correction in the coronal plane (4, 10).
Since 2010, there has been exponential growth in scientific publications on spine deformity and sagittal balance (11). Researchers have demonstrated the correlation of sagittal profile with clinical outcomes, quality of life index, and even long-term respiratory impairment (12, 13). Therefore, it is of outmost importance to investigate these specific adolescent patients with idiopathic scoliosis and thoracic hypokyphosis. It is also necessary to precisely determine the outcomes of an intervention for these patients. In this study, a limited number of AIS cases with thoracic hypokyphosis and undergoing posterior instrumentation and posteromedial translation (PMT) for correction were examined. To our knowledge, only a handful of studies had explored the sagittal profile of patients with AIS before our study.
2. Objectives
This study aimed to present the results of the sagittal and coronal correction of the patients with AIS and hypokyphosis (TK < 10) using pedicle screw (PS) instrumentation and reduction by a specific technique, namely PMT.
3. Methods
3.1. Study Design and Patients
This was a retrospective study on patients having undergone surgery at our center by a single senior surgeon. The patients were already diagnosed with AIS (Lenke type 1 - 4) and thoracic hypokyphosis (T4-T12 Cobb angle < 10°) and were followed up for at least two years. An intervertebral fusion was performed for all patients by employing a posterior-only approach and using PS instrumentation. Patients with a history of previous spinal surgery were excluded from the study. The mean follow-up was 39 months (24 - 54 months). Clinical analysis was carried out using the Scoliosis Research Society 22-item questionnaire (SRS-22r) completed before surgery and during the 2-year follow-up after surgery (14).
3.2. Radiographic Measurements
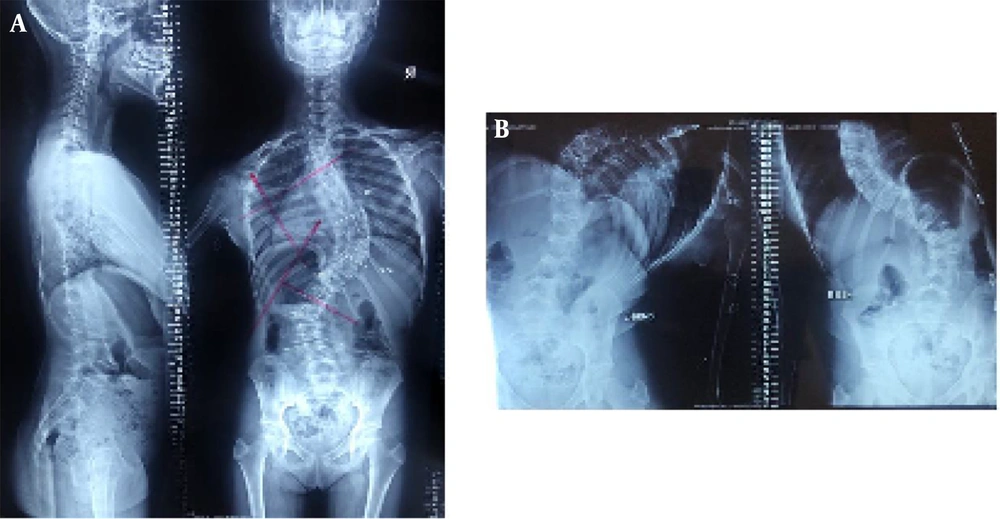
Standard, standing anteroposterior (AP) and lateral radiographies of the spine were performed before the surgery and one week, one month, one year, and then once a year after the surgery. Anteroposterior spine radiographs of the supine in lateral bending positions were obtained before the surgery. In addition, whole standing spine 36-inch radiographs were obtained in AP and lateral positions before and one month after the surgery and during 2-year follow-ups. All radiographic measurements were performed manually by the senior author/surgeon to examine the whole standing spine radiographs (Figures 1 and 2).
The Cobb’s angle was measured based on the AP standing view between the upper border of upper-end vertebrae and the lower border of lower-end vertebrae. The translation of the apex vertebra was measured as the distance between the center of the vertebral body and the central sacral line (CSL) of the main curve. Curve flexibility was measured based on AP supine radiographs in left and right lateral bending positions. Thoracic kyphosis was evaluated based on the lateral radiographs from the superior endplate of T4 to the inferior endplate of T12 (Figures 1 and 2).
3.3. Surgical Procedure
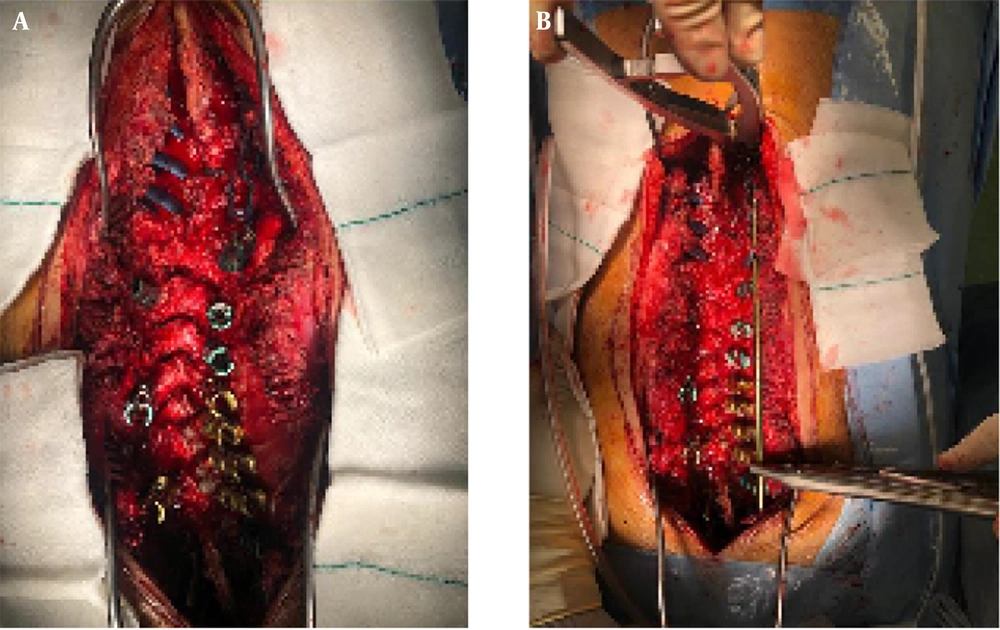
All surgeries were performed by the senior surgeon. The spine was subjected to a standard midline longitudinal incision, and the paraspinal muscles were reflected from the spinous processes and lamina laterally to the tips of transverse processes. Pedicle screws were inserted using a ‘‘free hand’’ technique, as described by Zenderick et al. (15), under an image intensifier; AP and lateral X-rays (C-arm) were taken after the placement of PSs. The employed instrumentation (all titanium construct) was suitable for implementing the PMT technique and relied on a stable anchoring of PS. All screws were polyaxial and included a threaded extension, which facilitated loading from the top and side connection to the rods with connecting clamps (Figure 3).
Grade-1 Schwab osteotomy, also known as Smith Peterson osteotomy (SPO), involving 5 - 6 levels (apex ± 3 levels), was performed prior to rod insertion (16-18). Beginning with bilateral superior and inferior facetectomy, the posterior column release continued through articular processes to the spino-laminar junction and adjacent spinous processes. Afterward, two 6.0 mm titanium rods were bent according to the sagittal profile and connected to the screws at the required distance without performing the reduction maneuver. First, the rod on the concave side was oriented towards the sagittal plane, and two nuts at the proximal end were tightened through the extensions in order to lock the rotation of the rod. Reduction of the deformity was achieved by the gradual tightening of all nuts on the threaded extensions, allowing a gradual approach of the vertebral column to the rod and, therefore, facilitating the translation maneuver. Then, the second rod was inserted in a similar fashion. No distraction/compression or in-situ bending of the rods was performed. Intraoperative neuromonitoring was used for all patients (Figure 3).
3.4. Statistical Analysis
Statistical analysis was conducted using the statistical package for the social sciences (SPSS) v22 for Windows. Two-tailed paired-samples t-tests with a 5% significance level (P < 0.05) were also performed. Distributions of the variables were presented as ranges mean, and standard deviations.
4. Results
4.1. Patient Demographics and Curve Characteristics
A total of 11 AIS patients (8 females and 3 males) with a mean age of 15.8 years (age range: 13 - 19 years) and diagnosed with hypokyphosis (TK < 10) underwent operations at our center between January 2000 and December 2020. The patients' demographic data and classification of the curve are presented in Table 1.
| Case | Age | Sex | Risser | Lenke | Pre-OP | Instrumentation | Post-OP (1 Month) | Post-OP (Final F/U) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cobb's Angle | Thoracic Kyphosis | Translation | Cobb's Angle | Thoracic Kyphosis | Translation | Cobb's Angle | Thoracic Kyphosis | Translation | ||||||
| 1 | 14 | F | 3 | 1A | 50 | 9 | 25 | T4-L2 | 2 | 33 | 0 | 8 | 35 | 0 |
| 2 | 16 | F | 4 | 3B | 120 | 9 | 75 | T2-L4 | 37 | 25 | 15 | 42 | 20 | 20 |
| 3 | 15 | M | 3 | 1A | 52 | 8 | 20 | T4-L1 | 3 | 25 | 0 | 5 | 25 | 0 |
| 4 | 14 | F | 2 | 3A | 72 | 3 | 40 | T4-L4 | 2 | 20 | 0 | 6 | 20 | 5 |
| 5 | 17 | F | 4 | 3A | 100 | 8 | 60 | T2-L4 | 40 | 30 | 20 | 43 | 28 | 20 |
| 6 | 13 | M | 3 | 1A | 57 | 9 | 30 | T4-L1 | 5 | 25 | 0 | 9 | 25 | 0 |
| 7 | 16 | F | 4 | 3C | 85 | 8 | 45 | T4-L4 | 8 | 29 | 5 | 11 | 26 | 10 |
| 8 | 15 | F | 3 | 1B | 64 | 3 | 35 | T4-L2 | 6 | 28 | 0 | 8 | 25 | 5 |
| 9 | 18 | F | 5 | 4C | 86 | 4 | 50 | T2-L5 | 15 | 25 | 10 | 22 | 20 | 15 |
| 10 | 17 | F | 4 | 2B | 66 | 6 | 30 | T1-L2 | 9 | 32 | 5 | 15 | 29 | 10 |
| 11 | 19 | M | 5 | 1A | 53 | 5 | 25 | T4-L1 | 5 | 30 | 5 | 5 | 25 | 5 |
a Risser grade: Classification used to grade skeletal maturity based on the level of ossification and fusion of the iliac crest apophyses. Lenke: Classification system organized according to the curve type (1-6) with a sagittal thoracic modifier (-, N, or +) and a lumbar spine modifier (A, B, C).
4.2. Surgical Data
The average number of instrumented levels was 11, the average operation time was 202.6, and the average blood loss was 310 mL (Table 1).
4.3. Coronal Plane Assessment
The results of preoperative and postoperative coronal plane measurements are presented in Table 1. Preoperative average Cobb’s angle of the major curve was corrected from 71.8° to 15.8° on the last follow-up visit (P < 0.001), suggesting an average correction of 78%. The median immediate post-operative correction was 59.7°, but it was 56.0° after two years, showing an average loss of 3.7° during follow-up, which was not significant and in line with the results reported by the literature (19). Preoperative average apex translation of the major curve decreased from 39.5 mm to 8.1 mm on the last follow-up visit (Table 2).
| Pre-OP | Imm. Post-OP | Last F/U | Correction Maintained | P-Value Pre/Last | |
|---|---|---|---|---|---|
| Cobb's angle | 71.82 | 12.18 | 15.81 | 56.0 (78%) | 0.001 |
| Translation (mm) | 39.5 | 5.4 | 8.1 | 31.4 (80%) | 0.004 |
| Thoracic kyphosis | 6.54 | 27.54 | 25.36 | 18.82 (75%) | 0.001 |
| SRS-22r (function) | 3.8 ± 0.7 | 4.2 ± 0.4 | 4.3 ± 0.6 | 0.5 | 0.508 |
| SRS-22r (pain) | 3.9 ± 0.4 | 3.8 ± 0.5 | 4.5 ± 0.3 | 0.6 | 0.067 |
| SRS-22r (self-image) | 3.1 ± 0.2 | 4.4 ± 0.6 | 4.6 ± 0.7 | 1.5 | 0.035 |
| SRS-22r (mental health) | 3.9 ± 0.6 | 4.3 ± 0.5 | 4.2 ± 0.8 | 0.3 | 0.192 |
| SRS-22r (satisfaction) | 3.3 ± 0.7 | 4.4 ± 0.2 | 4.5 ± 0.4 | 1.2 | 0.043 |
| SRS-22r (total) | 3.7 ± 0.3 | 4.1 ± 0.5 | 4.3 ± 0.7 | 0.6 | 0.077 |
Abbreviation: SRS-22r, Scoliosis Research Society 22-item questionnaire.
4.4. Sagittal Plane Assessment
Sagittal plane radiographic results for thoracic kyphosis are presented in Table 1. Preoperative average thoracic kyphosis significantly increased from 6.5° to 27.5° immediately after the operation and to 25.3° after two years of follow-up (P < 0.001). A mean correction of 18.8° (75%) was recorded on the last follow-up visit (Table 2).
4.5. Clinical Outcome
Scoliosis Research Society 22-item questionnaire revealed a trend of improvement in total scores from 3.7 to 4.3; however, the difference was not significant (P = 0.077) (Table 2). Scoliosis Research Society 22-item questionnaire subcategory analysis revealed a significant improvement in self-image (3.1 to 4.6, P = 0.035) and satisfaction (3.3 to 4.5, P = 0.043) (Table 2).
No perioperative complications were observed in our cohort, and no neurologic or vascular complications occurred due to the insertion of pedicle screws or the reduction maneuver deformity correction. No implant failures (e.g., screw or rod fractures) and no proximal junctional kyphosis (PJK) were observed in our cohort after two years of follow-up. One patient was readmitted due to the superficial wound infection and was treated successfully by administering intravenous (IV) antibiotics. No patient needed revision surgery.
5. Discussion
This study mainly investigated the sagittal profile of patients with AIS undergoing surgical correction. The majority of the patients presenting with AIS suffer from normal thoracic kyphosis (TK: 10 - 40) and a few from hyperkyphosis (TK > 40); these patients are separately classified and treated as a different entity 'kyphoscoliosis' (KS) (3, 20). The sagittal profile of the patients with KS is particularly highlighted, and a surgical technique is employed to ensure the restoration of a sagittal balance. However, insufficient attention is given to the sagittal profile in AIS patients presenting with hypokyphosis (TK < 10). In this study, the research attention focused on the surgical correction of both sagittal and coronal profiles in AIS hypokyphosis patients. In this study, moreover, the results of posterior spinal instrumentation and fusion to correct AIS with reduction by a posteromedial translation technique and focus on the sagittal plane were reported.
The surgical treatment of scoliosis largely aims at obtaining a balanced spine in both sagittal and coronal planes while preserving the mobility of the lumbar spine (if possible) with a mild residual curve and diminishing the neuro-vascular risk. To this end, a posterior spinal fusion (PSF) with all PS instrumentation is ideally employed since it provides a stable anchorage through all three columns of the spine and has an excellent potential for reducing maneuvers (21). Various rod insertion techniques and reduction maneuvers have been tested to improve the correction of the deformity, such as rotation of the rod (DVR), in situ rod bending (CR), and posteromedial translation (7, 8, 10). Each technique has advantages and disadvantages. In this study, the research attention was only directed at the translation maneuver of the rods in order to achieve the correction since describing each technique in detail was beyond our study scope and because other reduction techniques were already well-documented in the literature.
In DVR, the vertebral bodies are de-rotated and docked on the rods with the help of a specific de-rotation system. This technique facilitates an excellent correction in the axial plane, which in turn corrects the coronal deformity. However, such a method of reduction worsens the deformity in the sagittal plane. Watanabe et al. conducted a stimulation study on the data collected from 20 AIS patients and found that the de-rotation technique worsened hypokyphosis after a surgical correction of the coronal deformity using all pedicle screw construct (9).
In the CR technique, the vertebras are sequentially approximated or distracted using the in-situ method of rod bending. However, this technique has virtually little effect on the sagittal plane. Clement et al. carried out a comparative analysis between CR and translation technique while examining 44 patients with AIS (4). Accordingly, the technique of simultaneous translation was superior in restoring thoracic kyphosis. Few other studies reported similar results (22, 23).
In this study, 11 patients with AIS and severe hypokyphosis (TK < 10) were examined. The mean coronal and sagittal corrections in our patients were 59.6° and 21.0°, respectively. The technique of posteromedial translation was adopted for correcting the deformity, and corrections of 78% and 75% were achieved in coronal and sagittal planes, respectively. Stable anchorages such as pedicle screws are required for implementing an effective translation technique, and the achieved reduction is a compromise between the rigidity of the rods and the stiffness of the spine. The translation technique aims at pulling back the vertebral column toward the rods and bringing it closer to CSVL.
The anchorages used in our study were PS that included polyaxial threaded extension, which enabled PS to connect to the rods prior to the reduction maneuver. The polyaxiality of PS was an essential part of the instrumentation, connecting all PS to the rods simultaneously. Then, the progressive tightening of all screw nuts facilitated the gradual pulling of each instrumented vertebra towards the rods and, thus, performing a simultaneous translation. The reduction force is distributed along the length of the rods simultaneously, which improves the correction potential and prevents exertion at 1 - 2 screws, leading to pull-out. Pre-bending the rods based on a desired sagittal profile facilitates the restoration of TK in accordance with the sagittal profile of the rods.
In our study, it was hypothesized that the improved correction in the sagittal plane in our cohort resulted from the implementation of the translation technique. Contrary to other reduction maneuvers such as DVR and CR that majorly focus on the coronal and axial planes, the posteromedial translation technique considers the sagittal profile as well during the correction procedure. Although our 6.0 mm titanium rods were more flexible than chrome-cobalt or stainless-steel rods of the same diameter, it was argued that the translation technique may have explained our result.
According to a recent review of the literature, the sagittal balance has taken an important place in clinical practice, and presently, both researchers and clinicians are striving to identify its hidden characteristics. There has been an exponential growth in publications regarding the sagittal balance since 2010 (11). Studies have indicated that a sagittal profile imbalance may have more serious effects on the patients' quality of life than the disorders such as visual disturbances, chronic lung disease, rheumatoid, and osteo-arthritis (11, 24). Therefore, it is important to consider the sagittal profile of the patients undergoing surgical correction for AIS, specifically if these patients suffer from thoracic hypokyphosis. It is also necessary to have a clear understanding of the correction techniques in AIS and their effects on different planes.
Recently, Bodendorfer et al. performed a large multi-center retrospective review on 1063 AIS patients with thoracic hypokyphosis (25). However, their study only compared the restorations of thoracic kyphosis over a period of time and did not compare the techniques. According to their results, an optimum sagittal correction was achieved in 1995 - 2000 when more frequent anterior releases were performed as part of the deformity correction. However, the kyphosis correction worsened when the posterior-only approach was adopted. After 2010, as our research team began to appreciate the importance of the sagittal balance and the effect of each reduction technique in different planes, the correction of thoracic kyphosis in AIS improved significantly. The authors also highlighted several factors responsible for such improvement, one of which was the simultaneous translation technique. The study, however, suggested that the surgical correction of AIS exhibited considerable variability in approach, implant choice, instrument configuration, and reduction methods. In the last few decades, there has been a rapid progression regarding how to approach AIS and achieve a balanced spine as the end result.
Kim et al. highlighted the importance of sagittal plane correction in AIS and its association with PJK (26). In their cohort, a postoperative decrease in thoracic kyphosis was found to increase the risk of developing PJK. In this study, it was argued that a residual hypokyphosis may have resulted in compensatory junctional hyper-kyphosis. Therefore, the restoration of the sagittal plane may have been as necessary as the coronal and axial corrections.
As a result of limited evidence on the sagittal profile in patients with AIS, the impact of thoracic kyphosis on physical function has remained unknown. According to the results of SRS-22r in our study, however, thoracic kyphosis was a significant factor contributing to the overall postoperative improvement, specifically to the satisfaction and self-image of the patients. The total score of SRS-22r improved after the operation; however, significant improvements were recorded for subscales of satisfaction and self-image. Furthermore, SRS-22r was not compared with other reduction techniques in our study, as was the case with other previously published studies. Our results demonstrate that the patients held a subjective view of the restoration of kyphosis and regarded it as a procedure providing higher self-image and satisfaction.
In the current study, a median gain of 21° was achieved for the posteromedial translation in terms of kyphosis. According to our results, moreover, the effectiveness of our technique in correcting the sagittal profile in AIS patients with hypokyphsis was confirmed.
Our study had a few limitations. For instance, it was a retrospective analysis of the prospectively collected data from patients undergoing operations at a single center and, therefore, was subjected to errors in data entry and interpretation.
5.1. Conclusions
In sum, the posteromedial translation technique facilitated the tri-planar correction of hypokyphotic spine in AIS patients. In addition to coronal plane correction, the translation technique was an effective maneuver for the correction of sagittal hypokyphosis. The mean gain of kyphosis in our cohort was 21°. Given the ease of use and widespread availabilities of these surgical instruments, it was recommended that the posteromedial translation technique should be used for correcting hypokyphosis in patients with adolescent idiopathic scoliosis.