Abstract
Background:
Due to advancements in technology, endovascular techniques (EVT) are considered a mainstay of treatment for intracranial aneurysms. However, for patients with anatomically complex aneurysms, associated intracranial hematomas requiring evacuation still need an open surgical clipping as the first line of treatment. Microsurgical clipping is an alternative for patients who cannot afford the high cost of EVT treatment.Objectives:
This paper presents our experience in surgical clipping of symptomatic intracranial aneurysms performed in our hospital from Jan 2010 to Dec 2013 on 170 patients. Based on the data, this study recommends microsurgical clipping as a viable and cost effective option for symptomatic intracranial aneurysms.Patients and Methods:
This study was a retrospective analysis of case records of patients who had been treated for symptomatic intracranial aneurysms, including both ruptured and unruptured intracranial aneurysms, at Krishna institute of medical sciences from January 2010 to December 2013. A total of 230 patients, who had clinical and radiological evidence of symptomatic intracranial aneurysms, were admitted into the study. Of the total number of patients, 170 had been managed with microsurgical clipping. The patient’s demographics, the features of the aneurysms, clinical grades, cost effectiveness, and outcomes were analyzed. Excluded from the study were 60 patients who had been treated with the endovascular technique.Results:
Of a total of 170 patients who underwent surgical clipping, 158 (93%) patients had an aneurysm in the anterior circulation and 12 (7%) in the posterior circulation. In the study group, 160 (94%) patients survived and 10 (6%) patients expired. One patient (0.58%) in the clipping group had a rebleed, and 4 (6.6%) patients from the coiling group eventually underwent clipping due to failed coiling. The average duration of hospital stay for the study group was 13 days and the cost for the treatment was Rs 2, 89, 238. The reasons for clipping in our patients were complex aneurysmal anatomy, difficulty accessing the aneurysm and MCA location in 60 (35%) patients, cost factor in 72 (42%) patients, non-availability of endovascular operator and hardware in 17 (10%) patients, associated hematoma requiring evacuation in 17 (10%) patients, and failure of the endovascular technique in 4 (2.5%) patients. Regarding outcomes, 83% of patients experienced a good outcome and 17% experienced a bad outcome.Conclusions:
These observations suggested that microsurgical clipping is a viable and cost effective alternative in the management of intracranial aneurysms in this endovascular era.Keywords
1. Background
Intracranial aneurysms are acquired cerebrovascular anomalies that develop throughout a patient’s lifetime (1). Intracranial aneurysms are arterial lesions defined by thinned and dilated regions of the cerebrovascular wall that exhibit loss of the internal elastic lamina, thinning of the tunica media, and subsequent remodeling and degradation of extracellular matrix proteins throughout the vessel wall. Most aneurysms occur at bifurcation sites along the circle of Willis, as these areas are prone to hemodynamic patterns that potentiate aneurysm development (2). The key to minimizing the risk of rebleeding, following aneurysmal rupture, is to isolate the aneurysm from its cerebral circulation, either by surgical clipping or endovascular techniques (EVT). In 2002, the international subarachnoid aneurysm trial (ISAT) caused a paradigm shift in the management of ruptured intracranial aneurysm towards a preference for endovascular coiling over surgical clipping (3). Furthermore, the recent barrow ruptured aneurysm trial (BRAT) conducted by McDougall et al. also concluded that patients who underwent surgical clipping were 1.68 times more likely to have poor outcomes compared to those who underwent EVT. In addition, the one-year follow up of patients who underwent endovascular coiling showed a good outcome compared to clipping patients (4). However, the recently published ISAT 5-year follow up data demonstrated that the differences in outcomes of the two treatment modalities have vanished over the years (5). Although EVT is evolving and considered to be the first line option for management of intracranial aneurysms, there is a subset of patients for whom surgery could be considered as the preferred and cost effective alternative. These patients include those with complex angiographic anatomy, severe atherosclerosis of the neck vessels, tortuous neck vessels, very small blood blister-like aneurysms, aneurysms associated with intracranial hematomas requiring surgical evacuation, and patients who cannot afford the high cost of EVT.
2. Objectives
In this paper, we have retrospectively analyzed the demographic data of the patients, the morphology of the aneurysm, intraprocedural and postoperative complications, the cost of treatment, the reasons for surgery as an option, and the outcomes of patients who had been treated for intracranial aneurysm by surgical clipping.
3. Patients and Methods
This study was a retrospective analysis of all patients admitted with angiographic evidence of symptomatic intracranial aneurysms, including ruptured and unruptured intracranial aneurysms, from January 2010 to December 2013 at Krishna institute of medical sciences Ltd., Secunderabad, India. Upon admission, patients underwent a clinical evaluation according to WFNS grading and computed tomography (CT) SAH Fisher grading. All patients were subjected to digital subtraction angiography (DSA) or CT angiogram of the brain. Patients who had non-aneurysmal SAH, patients who refused any mode of treatment, and patients who underwent coiling were excluded from this study. About 19 patients had non-aneurysmal SAH in the initial scan, and were followed up with DSA and CT angiogram four weeks after the first scan. Four patients who had angio-negative SAH in the initial scan were positive for aneurysm in the follow-up period and also underwent definitive treatment. A total of 230 patients had confirmed angiographic evidence of aneurysm. The 170 patients who underwent surgical clipping were considered for this study. The following data were collected in all cases: (a) patients WFNS grades of ruptured aneurysms; (b) intraprocedural complications and postoperative complications; (c) total length of hospital stay; (d) cost of treatment; and (e) Glasgow outcome scale score at discharge and three months after discharge.
3.1. Our Treatment Policy
The decision to use clipping and coiling was considered by the neurosurgeon and an interventional neuroradiologist. The patient’s party had been thoroughly counselled about the nature of the disease and the pros and cons of each treatment modality. Surgery was opted for in most cases by the patient’s party, as it was cheaper than coiling in our hospital setup. The patient/family was informed of the principles and risks of the chosen modality of treatment and consent was obtained in all cases.
3.2. Patients With Multiple Aneurysms
Multiple aneurysms were found in 22% (n = 50) of the patients. The strategic plan was to treat the aneurysm that was likely to be responsible for the rupture, unless a second aneurysm was seen in the same side on craniotomy. Additional aneurysms were clipped or coiled in a second sitting on a later date.
3.3. Treatment Surgical Clipping
All admitted patients underwent a diagnostic four-vessel angiogram as early as possible. In stable patients, surgery was performed immediately after the angiogram. We prefer early surgery, before the patient develops clinical vasospasm. The median time delay from the day of ictus to surgery in the surgical group was 2.7 days. All surgeries were performed by a single senior neurosurgeon who had 18 years of experience. The surgical repair of the aneurysms was done by standard pterional craniotomy in a majority of the anterior circulation aneurysms, and in some cases fronto-temporo-zygomatic osteotomy, temporal craniotomy, and subtemporal approaches were used. Suboccipital craniotomies and far lateral approaches were used for posterior circulation aneurysms. Post-clipping indocyanine green injections with fluorescein angiograms were conducted in some cases to confirm the completeness of the occlusion and the patency of the perforators, parent artery, and the branches. Technical complications during surgery were noted. All microsurgical clippings were postoperatively managed in the ICU with triple-H therapy, nimodipine for 21 days, and post clipping blood pressures were maintained at around 140 systolic. If required, inotropics were used.
3.4. Clinical Follow up
The Glasgow outcome scale (GOS) was used to measure the neurological and functional outcomes. At the time of discharge, and at the end of three months after discharge, all patients were evaluated clinically with the GOS. The GOS is a five-point score applied to victims of traumatic brain injury. It is also widely used in SAH patients for assessment of outcomes. Patients with a GOS score of 1, 2, or 3 were collectively grouped as “poor outcome” and GOS scores of 4 or 5 were grouped as “good outcome”.
4. Results
During the study period, a total of 230 patients with confirmed aneurysms were managed in the study hospital. Of the total, 170 patients underwent surgical clipping and 60 underwent endovascular treatment. Table 1 shows the demographic data of the surgical group patients. A total of 174 craniotomies and clipping procedures were performed for 194 aneurysms in 170 patients. Twenty (54%) patients with multiple intracranial aneurysms were addressed by single surgeries, and clipping of the aneurysms was performed through the same craniotomy. Four (10.8%) patients with multiple aneurysms underwent a second surgery. A total of 13 (35%) patients were informed about the necessity of coiling and clipping and were reluctant to proceed further. They are being followed up.
| Variable | No. (%) |
|---|---|
| Gender | |
| Female | 92 (54.1) |
| Male | 78 (45.88) |
| Ruptured aneurysms | 152 (89.4) |
| Unruptured aneurysms | 18 (10.5) |
| Multiple aneurysms | 37 (21.7) |
Though EVT is considered a first line of treatment, in our series a majority of the patients underwent surgical clipping. The reasons were as follows: 35% (60) of the patients had very complex angiographic anatomy, such as multilobulated aneurysm, 8.2% had blood blister-like aneurysm, 2.3% had acute angulations of the aneurysm with the parent artery, 2.3% had a wide neck with an increased dome neck ratio > 2, 15.2% had very small aneurysms < 3 mm, 3.5% had aneurysms branched from the dome, 3.5% from the parent artery, poor access to the aneurysm due to atherosclerosis and stricture of the ipsilateral neck vessels , and 3.5% had tortuous neck vessels.
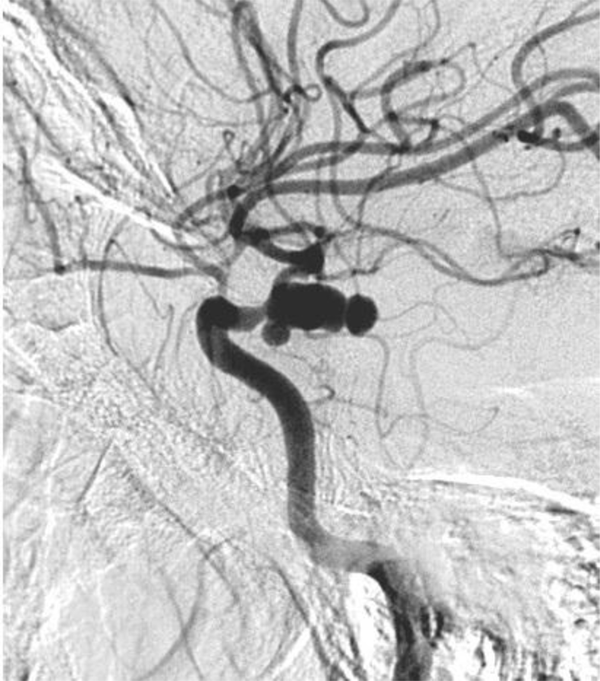
Case 1: A 56-year-old female presented with WFNS grade II on the second day of ictus with no comorbidity. Angiogram showed a complex multilobulated PCOM aneurysm. The option of coiling with flow diverters/pipeline stent-assisted techniques was discussed with the interventional radiologist and the patient’s party. Due to the non-availability of hardware, the patient was referred back to the surgeon for clipping. She underwent a pterional craniotomy and clipping of the aneurysm. There were no intraoperative complications and the postoperative period was uneventful (Figure 1).
Four Vessel Angiogram Picture Showing Multilobulated Irregular Shaped PCOM Aneurysm
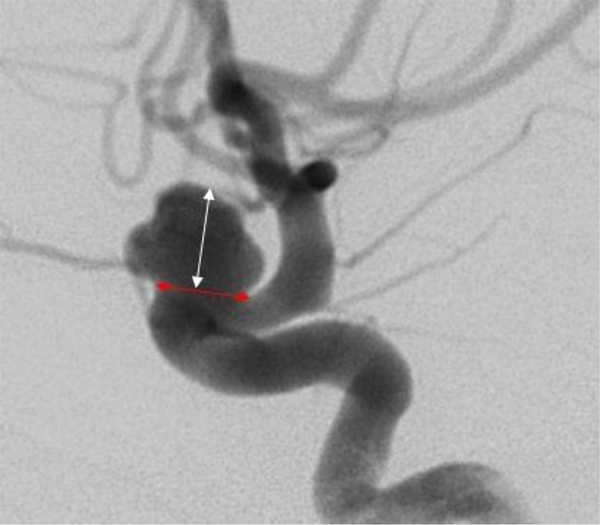
Case 2: A 48-year-old male presented within 12 hours of ictus with WFNS grade I. Angiogram revealed a wide neck paraclinoid aneurysm projecting superiorly-medially (Figure 2). He was advised about the coiling/endovascular technique as the patient had associated comorbidities such as obesity, smoking, and hypertension. Because of the cost factor, the patient’s family opted for surgical clipping, and he underwent front temporal orbitotomy and clipping of the aneurysm. The patient had a good recovery.
Wide Neck Paraclinoid Aneurysm Having a Dome-Neck Ratio < 2
Case 3: A 24-year-old female with no comorbidity presented on the second day of ictus with WFNS grade II and was found to have a fusiform aneurysm in the right PCA, incorporating the parent vessel in the four-vessel angiogram (Figure 3). The interventional radiologist was anticipating an infarct following coiling, as the aneurysm incorporated the distal PCA. Surgical clipping was performed on this patient. Postoperatively, the patient suffered with vasospasm, which was effectively managed with cisternal papaverine irrigation and the patient was discharged in two weeks with a GOS of five.
PCA Aneurysm Incorporating Parent Vessel in the Aneurysm Neck

Case 4: A 72-year-old male presented with a ruptured PCOM aneurysm with WFNS grade I. His angiogram revealed stricture in the proximal ICA with good normal filling distal to the stricture (Figure 4). The presence of stricture is one of the contraindications for coiling; therefore, the patient underwent a surgical clipping and had an uneventful recovery.
Atherosclerotic Stricture at Proximal Internal Carotid Artery

In our study, 10% of the patients had associated intracranial hematomas, such as intracerebral hematomas and subdural hematomas with mass effect, which warranted surgical evacuation. Giant intracranial aneurysms, requiring trapping of the aneurysm, wrapping, clipping, and reconstruction of the parent vessel, and bypass procedures occurred in seven patients. Financial constraints were a consideration in 40% of the patients, as they could not afford the high cost of EVT and opted for the low cost surgical technique. Of the total, 2.5% (4) of the patients had failure of the EVT and eventually underwent microsurgical clipping. Due to the absence of hardware or an endovascular operator, 10% (17) of the patients underwent surgery.
Case 5: A 39-year-old male with no comorbidity presented with a history of right-side stroke and was found to have a calcified ring lesion in the middle cranial fossa. He was referred for angiogram, which revealed a giant partially thrombosed aneurysm (Figure 5). He underwent a superficial temporal artery and MCA bypass and trapping of the aneurysm, and had a good postoperative outcome.
Giant, Partially Thrombosed Aneurysm

4.1. Detailed Results
The average size of aneurysms in the clipping group was 7 mm (2 mm - 4 cm); the average size of the neck was 4 mm (2 mm - 15 mm). In 158 patients, the aneurysm was located in the carotid circulation [ACom/ACA (71), MCA (31), ICA (24)]. In 12 patients, the aneurysm was located in the posterior circulation [PCA (3), basilar top (3), PICA (6), vertebral (2)]. The average time elapsed between the day of ictus to surgery was 2.7 days. Seven patients had giant aneurysms with intramural thrombus, while six patients had ruptured, very small aneurysms. Technical difficulties were encountered in about one-third of the surgical clipping patients such as difficulty in dissecting the sac or neck, injury to the nearby vessels, difficulty in application of the clip due to atherosclerosis in which part of the neck had to be left unclipped to avoid kinking of the parent vessels, and intraprocedural rupture and brain swelling that required decompressive craniectomy. About 45% of the patients had evidence of early or established hydrocephalus, requiring evacuation of the CSF from the ventricle before dural opening. Postoperative external ventricular drainage was required in 44 patients, and 12 patients required a permanent shunt.
The average hospital stay in the surgical clipping patients was 13 days. The average cost for treatment of surgical group was Rs 2, 89, 238.
Statistical Analysis of the Cost Factor Showing Mean and Standard Deviation of Expenditure in Rupees
| Statistical Parameter | Clipping |
|---|---|
| Mean | 270655 |
| Std Dev | 76985.2 |
| Std Error | 5904.5 |
| 95% CL Mean | 258999 - 282311 |
| 95% CL Std Dev | 69579.6 - 86168.9 |
Outcome of Surgical Clipping
| Variable | Value |
|---|---|
| N | 170 |
| GOS 5, 4 (favorable outcome), No. (%) | 140 (82.3) |
| GOS 3, 2, 1 (unfavorable outcome),No. (%) | 30 (17.6) |
| Overall survival rate, (%) | (94) |
| Mortality, (%) | (6) |
Among 170 patients who underwent surgical clipping, 140 (82.3%) patients had a good outcome, with a GOS score of 4 or 5. The survival rate percentage in clipping was 94%. Of the total surviving patients, 111 returned to work and 29 patients were able to perform daily activities of living without support but could not return back to work. Poor outcome was found in 30 (17.6%) patients with a GOS score of 1, 2, or 3. Of these, 14 patients had disability and required assistance for their activities of daily living. Six patients were severely disabled and bedridden, requiring PEG feeding and Foley catheters. Ten patients from the surgical group expired. Seven patients died during the admission period, and three patients died within three months of discharge. The patients who had a bad preoperative WFNS score did not fare well and succumbed to death. Of the patients who died, one patient died of myocardial infarction, another patient with HIV failed coiling, and another, who underwent a far lateral approach for vertebral artery dissecting aneurysm, developed septicemia and died. Over the three months of follow up, one patient had rebled and had already been operated on for a ruptured PCOM aneurysm. The aneurysm was about 11 mm, clipped with single clip during the first surgery, and there was a residual neck. In the follow-up angiogram, the patient presented with rebleed and underwent an emergency craniotomy and reinforcement of the neck with a second clip. Postoperatively, the patient improved.
Statistical Analysis of Survival Rate Survival Rate was 94%
| Statistical Parameter | Clipping |
|---|---|
| Mean | 0.9412 |
| Std Dev | 0.2360 |
| Std Error | 0.0181 |
| 95% CL Mean | 0.9054 - 0.9769 |
| 95% CL Std Dev | 0.2133 - 0.2641 |
5. Discussion
The results of the ISAT trial suggested that endovascular coiling gives rise to immediate results that are superior to surgery for the majority of aneurysms (5). There are clear advantages to coiling such as a shorter hospital stay, avoidance of open surgical manipulation of the brain, and the absence of postoperative epilepsy. In the present study, although the management results may be regarded as satisfactory, complications, such as hydrocephalus and infarct, occurred in 58 (34%) of patients, and 47 (27.6%) patients required surgery, such as bone flap removal, insertion of a reservoir, and a VP shunt procedure, in addition to the aneurysm operation. Most of the patients recovered from these complications and additional procedures. It is likely that coiling will eliminate most of these complications and additional operations, but there will be patients who will still require treatment for hydrocephalus (6).
Nevertheless, it is by no means certain that the long-term outcome of coiling will be as satisfactory as successful clipping of an aneurysm (7, 8). If a ruptured aneurysm can be fully clipped, as confirmed by postoperative angiography, then the condition may be regarded as cured and the long-term risk of recurrence of the aneurysm is negligible. The same does not apply to coiling. Reformation of the sac and further bleeding is known to occur in a handful of cases, at least in the short term, even if a sac appears to have been completely occluded at the time of initial coiling (9). The long-term risk of recurrence after coiling is simply not known. In coiling, recanalization is still a significant occurrence when compared to surgical clipping (10, 11). Recanalization, if significant, often requires retreatment either by re-coiling or surgical clipping.
5.1. Drawback of the Study
One limitation of this study is its retrospective design, with case selection bias, including both ruptured and unruptured aneurysm.
5.2. Conclusion
Most of our patients had a good outcome with microsurgical clipping in the management of intracranial aneurysms; hence, despite this endovascular era, we recommend microsurgical clipping as a viable and cost effective alternative in selected cases for the management of intracranial aneurysms.
Acknowledgements
References
-
1.
Dupont SA, Wijdicks EF, Lanzino G, Rabinstein AA. Aneurysmal subarachnoid hemorrhage: an overview for the practicing neurologist. Semin Neurol. 2010;30(5):545-54. [PubMed ID: 21207347]. https://doi.org/10.1055/s-0030-1268862.
-
2.
Penn DL, Komotar RJ, Sander Connolly E. Hemodynamic mechanisms underlying cerebral aneurysm pathogenesis. J Clin Neurosci. 2011;18(11):1435-8. [PubMed ID: 21917457]. https://doi.org/10.1016/j.jocn.2011.05.001.
-
3.
Hoh BL, Kleinhenz DT, Chi YY, Mocco J, Barker FG. Incidence of ventricular shunt placement for hydrocephalus with clipping versus coiling for ruptured and unruptured cerebral aneurysms in the Nationwide Inpatient Sample database: 2002 to 2007. World Neurosurg. 2011;76(6):548-54. [PubMed ID: 22251503]. https://doi.org/10.1016/j.wneu.2011.05.054.
-
4.
McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, et al. The barrow ruptured aneurysm trial: clinical article. J Neurosurg. 2012;116(1):135-44. https://doi.org/10.3171/2011.8.JNS101767.
-
5.
Molyneux AJ, SC Kerr R, Birks J, Ramzi N, Yarnold J, Sneade M, et al. Risk of recurrent subarachnoid haemorrhage, death or dependence and standardised mortality ratios after clipping or coiling of an intracranial aneurysm in the International Subarachnoid Aneurysm Trial (ISAT): long-term follow-up. Lancet Neurol. 2009;8(5):427-33. https://doi.org/10.1016/S1474-4422(09)70080-8.
-
6.
de Oliveira JG, Beck J, Setzer M, Gerlach R, Vatter H, Seifert V, et al. Risk of shunt-dependent hydrocephalus after occlusion of ruptured intracranial aneurysms by surgical clipping or endovascular coiling: a single-institution series and meta-analysis. Neurosurgery. 2007;61(5):924-33. discussion 933-4. [PubMed ID: 18091269]. https://doi.org/10.1227/01.neu.0000303188.72425.24.
-
7.
Hayakawa M, Murayama Y, Duckwiler GR, Gobin YP, Guglielmi G, Vinuela F. Natural history of the neck remnant of a cerebral aneurysm treated with the Guglielmi detachable coil system. J Neurosurg. 2000;93(4):561-8. [PubMed ID: 11014533]. https://doi.org/10.3171/jns.2000.93.4.0561.
-
8.
Mericle RA, Wakhloo AK, Lopes DK, Lanzino G, Guterman LR, Hopkins LN. Delayed aneurysm regrowth and recanalization after Guglielmi detachable coil treatment. Case report. J Neurosurg. 1998;89(1):142-5. [PubMed ID: 9647186]. https://doi.org/10.3171/jns.1998.89.1.0142.
-
9.
Tan IYL, Agid RF, Willinsky RA. Recanalization rates after endovascular coil embolization in a cohort of matched ruptured and unruptured cerebral aneurysms. Interv Neuroradiol. 2011;17(1):27-35.
-
10.
Sluzewski M, van Rooij WJ, Rinkel GJ, Wijnalda D. Endovascular treatment of ruptured intracranial aneurysms with detachable coils: long-term clinical and serial angiographic results. Radiology. 2003;227(3):720-4. [PubMed ID: 12773678]. https://doi.org/10.1148/radiol.2273020656.
-
11.
Willinsky RA, Peltz J, da Costa L, Agid R, Farb RI, terBrugge KG. Clinical and angiographic follow-up of ruptured intracranial aneurysms treated with endovascular embolization. AJNR Am J Neuroradiol. 2009;30(5):1035-40. [PubMed ID: 19299485]. https://doi.org/10.3174/ajnr.A1488.