Transcranial sonography (TCS) is an important tool for the careful study of certain areas of the central nervous system. It is unknown whether the extent of substantia nigra (SN) hyperechogenicity correlates with the degeneration of presynaptic dopaminergic neurons, but it is clear that this alteration is found widely and abundantly in patients with greater impairment and in the later stages of Parkinson’s disease (PD) (1). By observing closely and in real time some typical alterations of the SN and the region of the basal ganglia, we can discover details never seen before, due to the availability of ultrasound machines capable of providing information about certain small areas that other common diagnostic tools fail to detect. This is possible because the physical principles of ultrasound are different from those of other imaging methods. Ultrasound waves interfere with tissues that have different acoustic impedances, and are able to distinguish small differences within small anatomical regions of the brain. In addition, over the past decade, new discoveries have allowed deeper investigation of several extrapyramidal syndromes, not limited to parkinsonism, creating maps of their main ultrasonographic features (2-4).
In PD, hyperechoic areas are known to be present at the level of the SN They are assumed to be deposits of iron an ferritin (5-7). The same feature can be seen in corticobasal degeneration (CBD) and Lewy body dementia (LBD) (Figure 1).However, it is difficult to identify these different conditions studying only SN. It is important to remember that TCS is highly sensitive but it is not highly specific (8). Therefore, it is necessary to include more ultrasonographic details. If we identify hyperechoic areas in the lenticular region, we can direct our diagnosis at CBD. If there is a dilatation of the third ventricle, in addition to the presence of hyperechoic areas in the SN and the lenticular nucleus, the patient is likely suffering from LBD. The lack of hyperechoic areas in the SN excludes PD and points toward other parkinsonian syndromes, such as multiple system atrophy (MSA) and progressive supranuclear palsy (PSP). MSA has predominantly hyperechoic areas in the lenticular nuclei, whereas PSP presents dilatation of the third ventricle (sometimes associated with hyperechoic areas in the basal ganglia) (Figure 2). Only a short quote (description) to Huntington’s disease, in which we can find hyperechoic areas in the head of the caudate nucleus (copper deposits). More than 75% of patients with cervical or upper-limb dystonia display lentiform nucleus hyperechogenicity, so it is easier to distinguish this disease from functional forms of dystonia. This subject is both complex and fascinating, and is still the subject of argument and study. Many countries have already adopted TCS as a diagnostic method to improve performance and to allow clinicians to make a targeted diagnosis at earlier stages of disease. It is important to note that adequate training and knowledge of the tool is required for the use of TCS, as this technique is primarily operator-dependent (9).
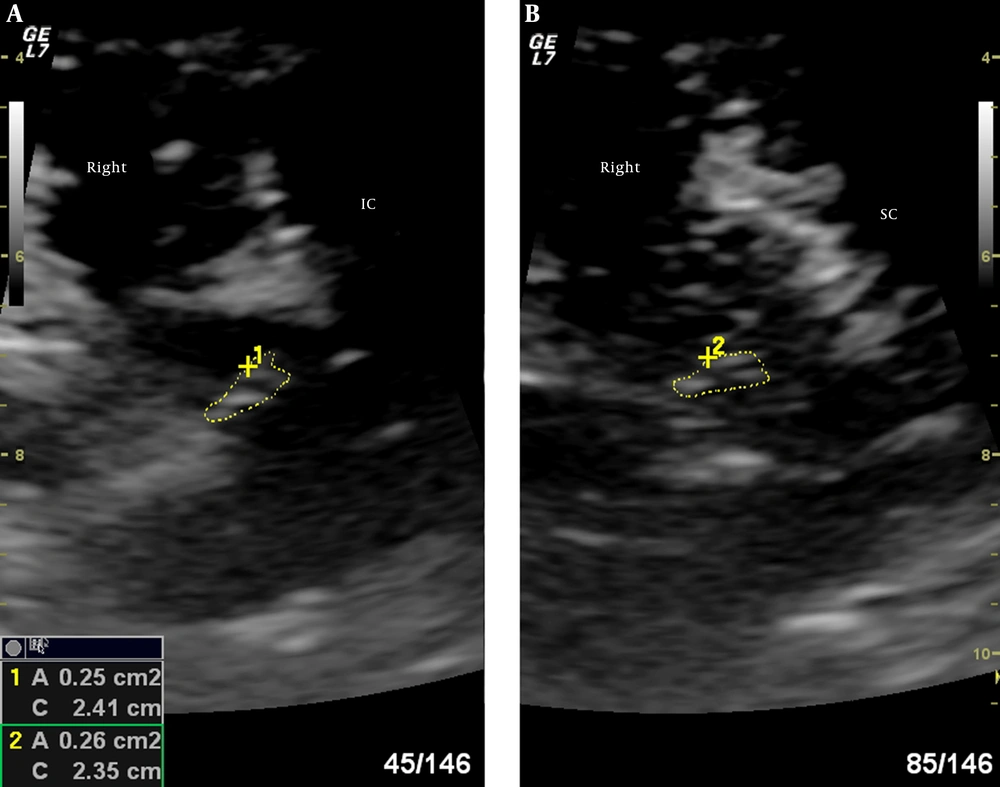
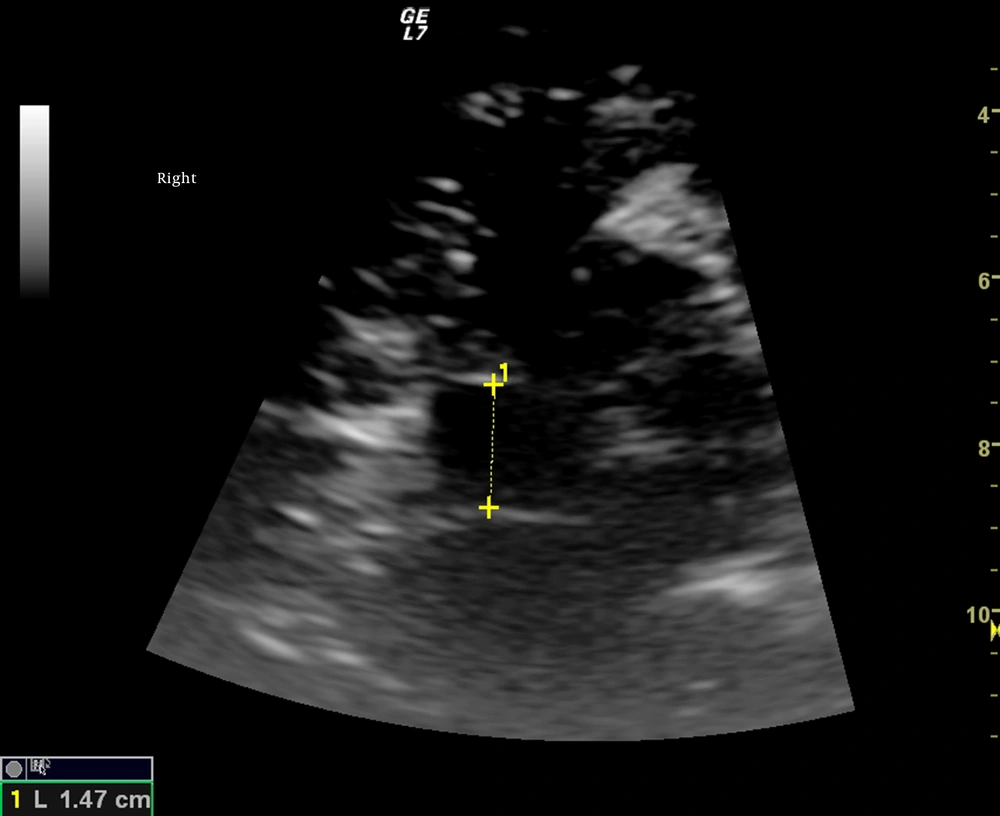
Hyperechoic areas in the SN are measured both at the level of the inferior and superior colliculus of the midbrain (10)