Abstract
Background:
Neurological trauma and diseases are the second cause of mortality and the main reason of acquired disability. Neurocritical care plays a major role in treating such patients. A longer life expectancy, treatment of incurable diseases, and limited resources available to add to hospital beds necessitates engineering the knowledge of health systems to prioritize allocation of current resources and present a proper pattern.Objectives:
The current study aimed at optimizing bed use and shortening the length of patients` hospitalization in neurocritical care unit (NCCU) of Loghman Hakim hospital affiliated to Shahid Beheshti University of Medical Sciences, Tehran, Iran, and completely stimulating the procedure of bed allocation and prioritization of patients.Methods:
Data of 420 patients hospitalized in NCCU was gathered and the procedure of bed allocation simulation was performed considering the priorities defined based on the length of hospitalization and patients’ chance of survival. The PROMETHEE (preference ranking organization method for enrichment evaluation) method was used to prioritize and allocate beds. To study the consequences of the suggested method, event discrete simulation tool was used to compare the current status and the results of the new method for 20 periods each including one month data.Results:
The mean number of patients admitted to NCCU during one month without any prioritization was 76, while it increased to 86 based on prioritization.Conclusions:
Patients’ simulation and prioritization using the PROMETHEE method resulted in 13% rise in the number of patients admitted to NCCU and higher utilization of this ward.Keywords
Bed Allocation NCCU Health Systems Engineering Simulation Prioritization
1. Background
In today’s modern world, neurological diseases and trauma especially cerebrovascular accident (CVA) are the second cause of mortality and the main reason of acquired disability. Treating these diseases in neurocritical care unit (NCCU) reduces the mortality. Allocation of intensive care beds (also known as NCCU) to patients with neurological disorders result in greater reduction in the mortality compared with what is observed for general intensive care unit (ICU) (1-7).
Considerable rise in life expectancy and the rising population of the elderly, feasibility of the treatment of complex diseases among patients with severe underlying diseases, and increasing trend of new diseases, are important to increase the access to ICU beds to preserve various medical outcomes (8).
Intensive care equipment as the most expensive and advanced hospital appliances play a major and vital role in treating and improving patients’ outcome (9). Timely access of patient and treatment teams to intensive care beds is very important (10) and when the patients with critical conditions are hospitalized in general wards where there are no experts and necessary equipment (11-13), the mortality rate increases among the patients (14). The waiting time for ICU bed availability varies between hospitals and countries, and typically ranges two hours to 3.5 days (15, 16).
Patients’ admission to ICU within the first 72 hours of critical conditions has a major effect on their survival rate (17). Some studies showed that if patients fail to be admitted to ICU in the exact time, the risk of death increases five times and the length of hospitalization is doubled (18).
Shortage or inappropriate allocation of equipment results in longer times that patients should wait in various wards and critically ill patients may need to be transferred to other hospitals. This shatters the confidence of patients and their families in the management of intensive care unit beds (19). On the other hand, providing hospital beds (particularly ICU beds) is always a big challenge in the developing countries, and optimized use of beds is the main determinant of hospitals’ productivity in a country (20).
It is necessary to improve access to these beds and increase their number. At the same time, proper and economical utilization of them needs to be managed using quality improvement methods.
Health system engineering seeks to find a systematic method to improve the procedure of bed allocation in such a way that this valuable resource can be used in the most efficient way.
When the system is complex and there are many non-linear interactions between the elements, classical mathematical methods may fail to analyze the system, but simulation is capable of analyzing every system. Simulation is a term to refer to a set of methods to mimic a real system behavior using computer technology. It seeks to analyze and study the performance of the system by analyzing and improving it through certain predictions. In other words, simulation is a sample of a real performance system using computer, which tries to possess all of its properties and parameters (21).
Simulation-based models present scenarios similar to real life conditions and their ultimate goal is to understand complicated interactions and procedures between them. To model the whole hospital, it is required to analyze all independent performances of wards, mutual effects wards have on each other, and keep in mind the randomized nature of the system. Simulation yields desired results as it is close to real conditions (22).
In the previous researches, simulation and mathematical modeling were used to determine the admission capacity and reduce the length of stay and waiting time for patients, which were performed with changes in equipment and human resources (23-26).
But in the current study, bed allocation simulation based on patients’ admission prioritization was used to optimize ICU bed utilization and decrease the length of hospitalization.
2. Methods
The current descriptive-applied study was conducted in the field of modeling and simulating ICU procedures. It was a practical example of health systems engineering science using discrete event simulation (DES) software called enterprise dynamic (ED) based on data obtained from 420 patients hospitalized in the NCCU of Loghman Hakim hospital affiliated to Shahid Beheshti University of Medical Sciences, Tehran, Iran from 2015 to 2017.
The data required for simulation was obtained from the NCCU data bank. To classify patients entering the ICU, data mining was conducted based on length of stay in NCCU using decision tree algorithm. Hospital information system (HIS) was used to extract the data of patients admitted to ICU.
By ED software, NCCU beds and patients waiting in the queue along with patients’ admission data and the data associated with the length of hospitalization were simulated and the resulted model was created without any prioritization based on the first-in, first-out (FIFO) order. Minitab software was used to validate the resulted model. The Kolmogorov-Smirnov test was used to determine the normality of data obtained during eight months in the real world with those obtained in the same period through simulation. After confirmation of data normality, the paired t test was used to compare the means of the two populations with an internal confidence (IC) of 95% and the validity of the model was verified.
Preference ranking organization method for enrichment evaluation (PROMETHEE), which is considered as a multi criteria decision-making (MCDM) method was used to prioritize patients admitted to NCCU. This is a structured method for preferential ranking. Patients’ prioritization was conducted considering survivability (positive criteria) and the length of hospitalization (negative criteria) as well as definitions of indifference and preference threshold, shape of the function, the weight of criteria, and data associated with choices (27).
With regard to patient prioritization, the simulation was diverted from the FIFO principle; hence, it was re-prioritized and the obtained results were compared with the prioritizations.
3. Results
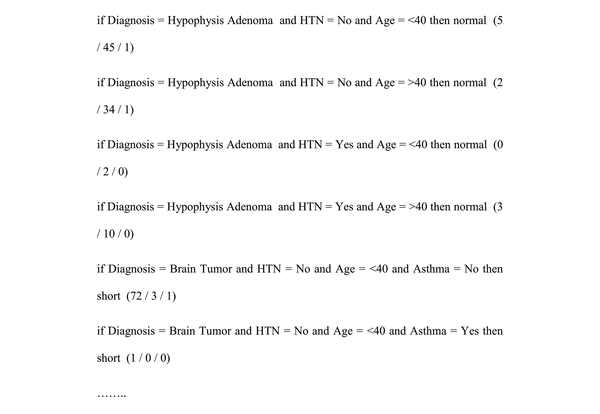
Data obtained from 420 patients admitted to NCCU by decision tree algorithm yielded 31 classes of patients entering NCCU, which is briefly presented in Figure 1.
Rules extracted through data mining (decision tree)
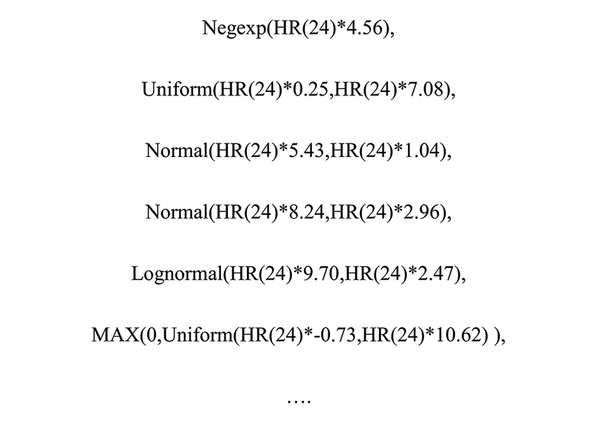
To produce patients` simulation model in NCCU, distribution of entrance level data and the length of hospitalization were defined for each patient (Figure 2) and the simulation model for 14 NCCU beds with FIFO order was formed. According to the output of Minitab software and zero in the range (-18.16, 12.44), the idea of the equality of the two populations was valid and the model had sufficient credibility.
Functions obtained from data associated with each class of patients admitted to NCCU
After ensuring validity of the simulation model, the model was conducted for 20 one-month periods and the mean entry of patients in the non-prioritized state was 76 patients.
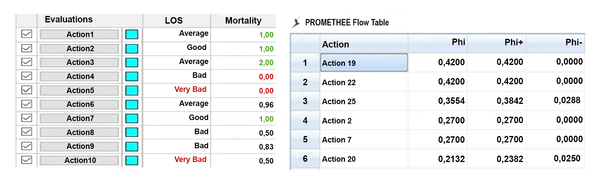
Figure 3 presents the results of prioritizing 31 classes of patients admitted to NCCU using the PROMETHEE method considering the survivability rate and the patients’ length of stay. Action represents patients’ classification, while Phi indicates the weight of criteria.
Patients’ prioritization using the PROMETHEE method
The results of a secondary simulation based on prioritization of patients admitted to NCCU for 20 one-month periods were equal to the mean value reported for 86 patients.
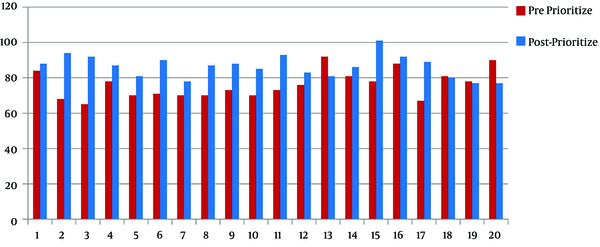
Table 1 and Figure 4 compared the two simulated models before and after patients’ prioritization in 20 one-month periods. The mean of data showed that 10 patients were added to the previous recorded number.
The Results of the Two Bed-allocation Model Prior to and After Prioritization
| Ave | SD | L-Bound (95%) | U-Bound (95%) | Min | Max | |
|---|---|---|---|---|---|---|
| Pre prioritize | 76.15 | 7.86 | 72.47 | 79.83 | 65 | 92 |
| Post-prioritize | 86.45 | 6.34 | 83.48 | 89.42 | 77 | 101 |
Comparing the number of patients admitted to NCCU before and after the prioritization
4. Discussion
NCCU beds as the most valuable hospital assets play a major role in the recovery, treatment, and rehabilitation of patients with neurological diseases. Inappropriate use of hospital beds increases costs, reduces efficiency, and contributes to a greater mortality. However, proper management of hospital beds, particularly ICU beds, improves the efficiency and reduces the mortality (9).
This issue is important in allocating NCCU beds and prioritizing the admission of patients with neurological diseases. Due to central nervous system’s sensitivity and the looming danger of disability influencing the patients in various degrees, providing timely care to patients with brain involvement is a vital issue in NCCU. Failing to take proper and timely therapeutic measures and hospitalizing such patients in ICU deteriorates their condition and secondary insults may occur (7, 28). Long-term hospitalization of some patients in NCCU with inadequate equipment endangers their priorities.
The current study employed simulation to present a model to assign beds based on prioritization in NCCU. This prioritization was conducted according to patients’ length of hospitalization and their survivability.
Based on the results achieved through prioritization, 76 patients were admitted to NCCU during one month without any defined prioritization criteria. This number increased to 86 when a prioritization criteria was defined indicating a 13% rise in the number of patients admitted to NCCU. As the survivability rate was taken into consideration in patients’ prioritization, the efficiency of the ward also increased.
There is no similar research focused on NCCU bed allocation simulation based on patients’ prioritization. However, a large number of simulation researches were performed in the field of hospital beds using expensive interventions and treatment team changes to reduce patients’ length of stay, waiting time, mortality rate, and efficiency.
To develop and improve a mathematical model to simulate bed occupation in ICU, Barado et al., (23) divided data of 6300 patients in Navarra hospital (Pamplona, Spain) to three categories. They presented a simulation model as a capacity analysis tool and their results showed how many beds were required to preserve the non-admission rate (5% and 10%) regarding population increase in the future (10% to 50% rise). Zeng et al., (24) used computational simulations to improve patients’ length of stay and waiting time in the emergency ward of a hospital. This simulation model altered the number of treatment team members to study its effect on the length of stay and waiting time patients usually experience. Their results pointed to a 5% reduction in the length of hospital stay, while this reduction for the waiting time ranged 13% to 26%. Zhu et al., (25) conducted a 12-month study of an ICU with 13 beds in Singapore to present a discrete event simulation model capable of predicting the effects of increasing ICU beds on the overall performance of the ward. Adding three more beds to ICU reduced bed occupation by 6%, while this reduction in rejected cases ranged 2% to 6%. Mathews et al., (26) conducted a study to provide a conceptual framework to increase the flow of patients in ICU. They planned a simulation to demonstrate how bed allocation changes can influence the bed occupation and waiting time. The results indicated a 7.2% decrease in waiting time and a 4% increase (80% to 84%) rise in bed occupation rate. Clermont et al., (29) studied 1400 patients in 49 ICUs in 11 different countries. By a time pattern obtained through multiple results of patients including mortality, length of hospitalization, etc., they presented a pattern which reduced the length of hospitalization from 8.1 to 7.7 days.
Furthermore, the current study made no alteration to the number of beds, treatment team staff, and equipment. Only a patient prioritization method was used through creation of a support system to help physicians in correct selection of patients for admission to NCCU. The results of the study indicated that priority-based bed allocation yielded a 13% rise in the patient admission rate and made a positive contribution to greater efficiency and optimized use of valuable assets of NCCU.
4.1. Conclusion
The employment of health systems management methods and prioritization of patients for NCCU beds allocation yielded a greater admission rate, a shorter length of stay in NCCU, and less mortality.
Acknowledgements
References
-
1.
Rezaei O, Shokouhi S, Hajiesmaeili M. Postoperative meningitis: The necessity of establishing a national comprehensive program. Arch Neurosci. 2016;3(2). https://doi.org/10.5812/archneurosci.34479.
-
2.
Rezaei O, Pakdaman H, Gharehgozli K, Simani L, Vahedian-Azimi A, Asaadi S, et al. S100 B: A new concept in neurocritical care. Iran J Neurol. 2017;16(2):83-9. [PubMed ID: 28761630]. [PubMed Central ID: PMC5526782].
-
3.
Nateghinia S, Afshar Kazemi MA, Sepehri MM, Goharani R. Better ICU management by analysis of clinical profile and outcomes of neuro-critical patients in neurocritical care unit. Arch Neurosci. 2018;5(1). https://doi.org/10.5812/archneurosci.61648.
-
4.
World Health Organization (WHO). Global Health Observatory (GHO) data. 2017. Available from: http://wwwwhoint/gho/mortality_burden_disease/causes_death/top_10/en/.
-
5.
Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6(2):182-7. [PubMed ID: 17239805]. https://doi.org/10.1016/S1474-4422(07)70031-5.
-
6.
Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8(4):355-69. [PubMed ID: 19233729]. https://doi.org/10.1016/S1474-4422(09)70025-0.
-
7.
Siegel J, Pizzi MA, Brent Peel J, Alejos D, Mbabuike N, Brown BL, et al. Update on Neurocritical Care of Stroke. Curr Cardiol Rep. 2017;19(8):67. [PubMed ID: 28646445]. https://doi.org/10.1007/s11886-017-0881-7.
-
8.
Angus DC, Kelley MA, Schmitz RJ, White A, Popovich JJ, Committee on Manpower for P, et al. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284(21):2762-70. [PubMed ID: 11105183].
-
9.
Amiri M. [Equity in distribution of intensive care beds in Iran with Gini coefficient and Lorenz curve approach]. Yafteh. 2011;12(2):75-83. Persian.
-
10.
Levin PD, Charles L. The process of intensive care triage. Springer; 2001.
-
11.
Blow O, Magliore L, Claridge JA, Butler K, Young JS. The golden hour and the silver day: detection and correction of occult hypoperfusion within 24 hours improves outcome from major trauma. J Trauma. 1999;47(5):964-9. [PubMed ID: 10568731]. https://doi.org/10.1097/00005373-199911000-00028.
-
12.
Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387-90. [PubMed ID: 11850367]. [PubMed Central ID: PMC65530]. https://doi.org/10.1136/bmj.324.7334.387.
-
13.
Sebat F, Musthafa AA, Johnson D, Kramer AA, Shoffner D, Eliason M, et al. Effect of a rapid response system for patients in shock on time to treatment and mortality during 5 years. Crit Care Med. 2007;35(11):2568-75. [PubMed ID: 17901831]. https://doi.org/10.1097/01.CCM.0000287593.54658.89.
-
14.
Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP; Delay-Ed study group. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35(6):1477-83. [PubMed ID: 17440421]. https://doi.org/10.1097/01.CCM.0000266585.74905.5A.
-
15.
Duke G, Green J, Briedis J. Survival of critically ill medical patients is time-critical. Crit Care Resusc. 2004;6(4):261-7. [PubMed ID: 16556104].
-
16.
Parkhe M, Myles PS, Leach DS, Maclean AV. Outcome of emergency department patients with delayed admission to an intensive care unit. Emerg Med (Fremantle). 2002;14(1):50-7. [PubMed ID: 11993835].
-
17.
Simchen E, Sprung CL, Galai N, Zitser-Gurevich Y, Bar-Lavi Y, Gurman G, et al. Survival of critically ill patients hospitalized in and out of intensive care units under paucity of intensive care unit beds. Crit Care Med. 2004;32(8):1654-61. [PubMed ID: 15286540]. https://doi.org/10.1097/01.CCM.0000133021.22188.35.
-
18.
Young MP, Gooder VJ, McBride K, James B, Fisher ES. Inpatient transfers to the intensive care unit: delays are associated with increased mortality and morbidity. J Gen Intern Med. 2003;18(2):77-83. [PubMed ID: 12542581]. [PubMed Central ID: PMC1494814].
-
19.
Bagust A, Place M, Posnett JW. Dynamics of bed use in accommodating emergency admissions: stochastic simulation model. BMJ. 1999;319(7203):155-8. [PubMed ID: 10406748]. [PubMed Central ID: PMC28163].
-
20.
Nabilu B, Mohebbi I, Alinezhad H. [Productivity of hospital beds: Evaluation of inpatient bed days in the West Azerbaijan selected hospitals]. J Urmia Nurs Midwifery Fac. 2012;10(4). Persian.
-
21.
Jung AL, Streeter NS. Total population estimate of newborn special-care bed needs. Pediatrics. 1985;75(6):993-6. [PubMed ID: 4000800].
-
22.
Garg L, McClean SI, Barton M, Meenan BJ, Fullerton K. Intelligent patient management and resource planning for complex, heterogeneous, and stochastic healthcare systems. IEEE Trans Syst Man Cybern A. 2012;42(6):1332-45. https://doi.org/10.1109/tsmca.2012.2210211.
-
23.
Barado J, Guergue JM, Esparza L, Azcarate C, Mallor F, Ochoa S. A mathematical model for simulating daily bed occupancy in an intensive care unit. Crit Care Med. 2012;40(4):1098-104. [PubMed ID: 22067625]. https://doi.org/10.1097/CCM.0b013e3182374828.
-
24.
Zeng Z, Ma X, Hu Y, Li J, Bryant D. A simulation study to improve quality of care in the emergency department of a community hospital. J Emerg Nurs. 2012;38(4):322-8. [PubMed ID: 21963136]. https://doi.org/10.1016/j.jen.2011.03.005.
-
25.
Zhu Z, Hen BH, Teow KL. Estimating ICU bed capacity using discrete event simulation. Int J Health Care Qual Assur. 2012;25(2):134-44. [PubMed ID: 22455178]. https://doi.org/10.1108/09526861211198290.
-
26.
Mathews KS, Long EF. A Conceptual Framework for Improving Critical Care Patient Flow and Bed Use. Ann Am Thorac Soc. 2015;12(6):886-94. [PubMed ID: 25822477]. [PubMed Central ID: PMC4590022]. https://doi.org/10.1513/AnnalsATS.201409-419OC.
-
27.
Zhaoxu S, Min H. Multi-criteria Decision Making Based on PROMETHEE Method. Computing, Control and Industrial Engineering (CCIE), 2010 International Conference on. IEEE; 2010. p. 416-8.
-
28.
Castillo J. Deteriorating stroke: diagnostic criteria, predictors, mechanisms and treatment. Cerebrovasc Dis. 1999;9 Suppl 3:1-8. [PubMed ID: 10436319]. https://doi.org/10.1159/000047548.
-
29.
Clermont G, Kaplan V, Moreno R, Vincent JL, Linde-Zwirble WT, Hout BV, et al. Dynamic microsimulation to model multiple outcomes in cohorts of critically ill patients. Intensive Care Med. 2004;30(12):2237-44. [PubMed ID: 15502934]. https://doi.org/10.1007/s00134-004-2456-5.
