Abstract
Background:
Hydatid disease (HD) is still an important health hazard in the world. This disease is a parasitic infestation endemic in many sheep- and cattle-raising areas such as Iran.Objectives:
This study aimed to review the clinical manifestations, laboratory aspects, imaging findings, and management of HD.Patients and Methods:
Data were collected from the medical records of patients diagnosed with HD in eight referral hospitals in different provinces of Iran from 2001 to 2014.Results:
Overall, 161 children at a mean age of 9.25 ± 3.37 years (age range = 1 - 15 years old) hospitalized with a definite diagnosis of the hydatid cyst between 2001 and 2014 were studied. The male-to-female ratio was 1.6:1. The most commonly involved organ was the lung (67.1%), followed by the liver (44.1%) and a combined liver and lung involvement was found in 15.5% of the patients. The cysts were found more frequently in the right lobe of the liver and lung than in the left lobe. The most frequent complaints were fever (35.4%) and abdominal pain (31.7%), and the most frequent sign was an abdominal mass in the liver involvement and cough in the lung involvement. There was a high eosinophil count (> 500/micL) in 41% of our cases. A high erythrocyte sedimentation rate (> 30) or positive C-reactive protein (based on the qualitative method) was found in 18.6% of the patients and leukocytosis > 15000/micL in 29.2% of the children. Ultrasonography was the main imaging test, with an accuracy rate of 96%, and chest X-ray was helpful in 88.6% of the cases. Surgery was performed in 89% of the patients, and selective patients underwent percutaneous aspiration-injection-reaspiration drainage or medical treatment.Conclusions:
The lung was the most commonly involved organ in the children recruited in the present study. Given the high probability of multiple organ involvement, we recommend that patients with HD be assessed via ultrasonography and chest X-ray. In endemic regions, unexplained eosinophilia should be considered as a parasitic disease like HD and its complications.Keywords
1. Background
Hydatid disease (HD), also known as hydatidosis, is still a global problem in highly endemic areas such as Iran (1, 2). The hydatid cyst is the larval stage of Echinococcus granulosus, which is hosted by dogs and other canines (3, 4). Humans are intermediate hosts by eating the tapeworm eggs (5). According to recent estimations, echinococcosis is responsible for about 1 - 220/10000 infections in the common areas (2, 6, 7).
HD is commonly asymptomatic, and often the cysts are detected incidentally (8). In other cases, the symptoms vary largely and are non-specific, depending on the location, size, rupture, and infection of the cysts (9). The liver and lung are the most commonly involved organs in humans; and in children, the lung is more frequently infected (10-14). An elevated eosinophil count in a patient from an endemic region accompanied by non-specific symptoms such as abdominal pain, abdominal mass, and cough, is suggestive of HD (15). The diagnosis is usually made via imaging modalities (i.e. ultrasonography and chest X-ray) and confirmed by pathology (16). Surgery is the chief therapeutic method for the management of HD, although currently percutaneous aspiration-injection-reaspiration drainage is regarded as a first choice in many cases (9, 14).
The present study was performed to evaluate the epidemiological aspects, clinical presentations, paraclinical findings, and management of HD in Iranian children.
2. Objectives
We sought to review the clinical manifestations, laboratory aspects, imaging findings, and management of HD.
3. Patients and Methods
In this retrospective study, we investigated the medical records of 161 patients (1 - 15 years old) with a definite diagnosis of HD admitted to eight major referral hospitals of Iran during a 13-year period (2001 - 2013). Data were collected on sex, age, clinical manifestations, anatomical location of the cysts, size and number of the cysts, laboratory tests, and therapeutic management. Statistical analysis was carried out using statistical package for the social sciences (SPSS) version 18.
4. Results
The study population consisted of 99 (61.5%) boys and 62 (38.5%) girls (range = 1 - 15 years old) from eight teaching referral hospitals around Iran (Table 1).
| University-Hospital | Values |
|---|---|
| Isfahan-Emam Hosein | 45 (28) |
| Shanhid Beheshti-Mofid | 32 (19.9) |
| Zahedan-Ali Ebne Abitaleb | 24 (14.9) |
| Kordestan-Besat | 14 (8.7) |
| Kermanshah-Emam Reza | 13 (8.1) |
| Iran-Ali Asghar | 12 (7.5) |
| Hamedan-Besat | 12 (7.5) |
| Arak-Amir Kabir | 9 (5.6) |
| Total | 161 (100) |
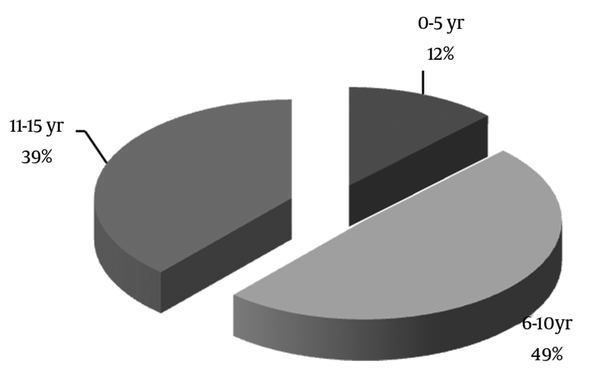
Echinococcosis was diagnosed in all our patients via pathology. The mean age of the study population was 9.25 ± 3.37 years, and most of the affected patients (49.1%) were in the age range of 6 to 10 years old (Figure 1).
Distribution of the Patients’ Age
The most frequent anatomical location of the hydatid cysts was the lung (in 108 (67.1%) patients), followed by the liver (in 71 (44.1%) patients). Additionally, the cysts were detected in the kidney (2.5%), spleen (2.5%), brain (1.9%), colon (1.2%), heart (0.6%) and eye (0.6%). Multiple organ involvement was found in 32 (19.8%) patients, with a single-to-multiple ratio of about 4: 1. There was no significant statistical difference between age (P = 0.551) or gender (P = 0.243) and the anatomical location of the cysts.
Our patients had totally 335 cysts: 181 (54%) with right-sided and 138 (41%) with left-sided cysts. Regarding size, 130 (39%) cysts were smaller than 5 cm in diameter, 157 (47%) cysts were between 5 and 10 cm in diameter, and 47 (14%) cysts were more than 10 cm in diameter (Table 2).
| Location | No. of Patients | No. of Cysts |
|---|---|---|
| Liver | 71 (44.1) | 137(40.5) |
| Right lobe | 54 (57.4) | 78 (56.9) |
| Left lobe | 40 (42.6) | 59 (43.1) |
| Lung | 108 (67.1) | 182 (54.3) |
| Right upper lobe | 15 (11.1) | 21 (11.5) |
| Right lower lobe | 52 (38.2) | 66 (36.3) |
| Right intermediate lobe | 11 (8.1) | 16 (8.8) |
| Left upper lobe | 19 (13.9) | 26 (14.3) |
| Left lower lobe | 39 (28.7) | 53 (29.1) |
| Other sites | 15 (9.3) | 16 (4.8) |
| Spleen | 4 (2.5) | 5 (31.25) |
| Kidney | 4 (2.5) | 4 (25) |
| Brain | 3 (1.9) | 3 (18.75) |
| Colon | 2 (1.2) | 2 (12.5) |
| Heart | 1 (0.6) | 1 (6.25) |
| Eye | 1 (0.6) | 1 (6.25) |
| Total | 161 (100) | 335 (100) |
Fever was the most common complaint (35.4%). Cough was the most common symptom associated with the lung hydatid cyst (29.8%) and an abdominal mass was more common in the liver hydatidosis (9.3%) (Table 3).
| Chief Complaint | Values |
|---|---|
| Fever | 57 (35.4) |
| Abdominal pain | 51 (31.7) |
| Cough | 48 (29.8) |
| Chest pain | 34 (21.1) |
| Dyspnea | 34 (21.1) |
| Nausea/vomiting | 21 (13) |
| Weight loss | 20 (12.4) |
| Anorexia | 20 (12.4) |
| Abdominal mass | 15 (9.3) |
| Pulmonary effusion | 14 (8.7) |
| Hepatomegaly | 12 (7.5) |
| Hemoptysis | 11 (6.8) |
| Lung abscess | 11 (6.8) |
| Respiratory distress | 8 (5) |
| Allergic reaction | 6 (3.7) |
| Cholestasis | 3 (1.9) |
| Urinary tract infection | 3 (1.9) |
| Biliary colic | 2 (1.2) |
| Liver abscess | 2 (1.2) |
| Splenomegaly | 2 (1.2) |
| Seizure | 2 (1.2) |
| Incidental findings | 24 (14.9) |
Laboratory data showed eosinophilia (≥ 500/micL) in 66 children, leukocytosis (WBC ≥ 15000/micL) in 47 patients, erythrocyte sedimentation rate (ESR) ≥ 30 and positive C-reactive protein (CRP) in 30 patients, and anemia (Hb ≤ 11 g/dL) in 28 patients. We assessed the abdominal sonography reports in 87 patients, which revealed the hydatid liver cyst in 83 (95.4%) cases. There were 79 chest X-ray reports, 70 (88.6%) of which suggested the lung hydatid cyst. Computed tomography (CT) scan confirmed the diagnosis in all the patients suspected of having the cyst (Table 4).
| Radiologic Findings | Values |
|---|---|
| Chest X-ray, n = 79 | |
| Normal | 9 (11.4) |
| Abnormal | 70 (88.6) |
| Pure cyst | 35 (44.3) |
| Ruptured | 21 (26.6) |
| Mass | 7 (8.9) |
| Abscess formation | 5 (6.3) |
| Calcification | 2 (2.5) |
| Sonography, n = 87 | |
| Normal | 4 (4) |
| Abnormal | 83 (96) |
| Pure cyst | 55 (52.4) |
| Daughter cyst | 14 (13.3) |
| Ruptured | 7 (6.7) |
| Calcification | 3 (2.9) |
| Coarse echo | 2 (1.9) |
| Mass | 1 (1) |
| Abscess formation | 1 (1) |
| Computed tomography scan, n = 87 | |
| Normal | 0 (0) |
| Abnormal | 87 (100) |
| Pure cyst | 45 (51.7) |
| Ruptured | 18 (20.7) |
| Abscess formation | 9 (10.3) |
| Daughter cyst | 7 (8) |
| Mass | 5 (5.7) |
| Calcification | 3 (3.4) |
Overall, 143 (89%) patients underwent surgery, 12 (7%) patients were treated with percutaneous aspiration-injection-reaspiration drainage, and 6 (4%) patients were prescribed medication. Four out of these 6 patients were transferred to other hospitals for surgery.
5. Discussion
HD is still a health hazard in endemic countries (14). In the present study on 161 children in an age range of 1 - 15 years old, the demographical characteristics and infected sites, clinical presentations, paraclinical data, and treatment strategy were assessed. The majority of the study population were male (61.5% vs. 49.1%), and the mean age was 9.25 ± 3.37 years. Based on our findings, the lung was the most commonly involved organ (67%), followed by the liver (44%), and the combined organ involvement was seen in 19.8% of the cases. Generally, the right side was the dominant site of infection (54%). Laboratory data showed elevated eosinophil counts in 41% and ESR/CRP in 18.6% of the patients. Chest X-ray and abdominal sonography constituted the principal imaging modalities with respective accuracy rates of 88% and 96%.
The mean age of our patients was 9.25 ± 3.37 years, and 49.1% of them were in the age range between 6 and 10 years old. Males and females comprised 61.5% and 38.5% of the study population, correspondingly (male-to-female ratio = 1.6:1). Vlad et al. (8) studied 82 cases at a mean age of 10.8 years, the majority of them being between 10 and 14 years old. The female-to-male ratio was 1.6:1 (8). Djuricic et al. (18) reported the mean age of 10.1 ± 3.8 years in their study, which included 149 patients under 18 years of age. The authors found no significant difference in terms of the gender of their patients. In a large Iranian study, Mirshemirani et al. (1) reported the mean age of 11.8 ± 4.6 years in 100 patients. In our study, chiming in with the other studies, pre-adolescent years (between 8 and 12 years old) accounted for the most frequent age at clinical presentation. In Iran, various studies have demonstrated that boys are more likely to be infected by Eosinophilic gastroenteritis than girls. It should also be borne in mind that in Iran, boys tend to spend more time outdoors than girls, which can explain the higher incidence of HD in the male cases in our study.
Chaouachi et al. (17) studied 1195 cases of the hydatid cyst in children aged between 2 and 15 years at the Children’s Hospital in Tunis and reported that the most commonly involved organ was the lung (in 643 cases), followed by the liver (in 486 cases). Their result is similar to that in our study insofar as the lung was the most commonly involved organ (49.7%) in our patients, which is concordant with the results of some other similar studies on children (3, 4, 11). Nevertheless, there are some other studies that show a larger number of hydatid cysts in the liver than in the lung among children (8, 18, 19). Various genotypes of Echinococcus granulosus isolated form different animal sources can be responsible for the heterogeneity of the results and may contribute to a clinically or histologically heterogeneous disease (20, 21). Combined liver and lung involvement was detected in 15.5% of our cases, with the percentage of other combinations of the infected sites being 4.7%, which is in line with some other surveys performed in children (6% - 16%) (18, 22, 23). It is vitally important that the combined organ involvement not be missed because the maltreatment of the hydatid cyst can result in recurrence in patients.
The frequency of the uncommon anatomical locations of the hydatid cysts in the present study was 9.3%; the spleen and kidney comprised the majority of such locations. These results are slightly higher than those in the literature on the prevalence of hydatid cysts in the spleen (0.9% - 8%) and kidney (18, 23-33).
Single organ involvement was 80.2% in our study, and the single-to-multiple-organ ratio was 4:1, which is similar to those reported by Oudni-M’Rad et al. (4.3:1 in children) (23) and Talaiezadeh and Maraghi (5.7:1 in children) (34). The highest ratio was reported by Al-Shibani et al. (38:1) in cases under 20 years old (35).
Only a few studies have reported such laboratory data as eosinophil or WBC counts and ESR values (36-38). In a review article by Moro and Schantz (39), eosinophilia was found in fewer than 25% of the cases with HD. Our results showed eosinophilia (≥ 500/micL) in 41% and ESR ≥ 30 or positive CRP in 18.6% of the study population. We used a value range that was different from the one employed by Vlad et al. (8) as they found higher figures in their survey (eosinophilia ≥ 5% in 59% and ESR ≥ 10 in 68.7% of the pediatric patients). We think that the higher rate of this laboratory marker can be related to the higher risk of complications such as rupture and, accordingly, recommend that sufficient attention be paid to these results in hydatidosis patients.
Among our pediatric patients, the lung was the most commonly involved organ. We would, therefore, urge that physicians be aware of different radiological forms of echinococcosis on chest X-ray in endemic areas and consider the probability of multiple cysts or multiple organ involvement.
References
-
1.
Mirshemirani A, Khaleghnejad A, Kouranloo J, Sadeghian N, Rouzrokh M, Hasas-Yeganeh S. Liver Hydatid Cyst in Children (A 14-year Review). Iran J Pediatr. 2011;21(3):385-9. [PubMed ID: 23056818].
-
2.
Harandi MF, Hobbs RP, Adams PJ, Mobedi I, Morgan-Ryan UM, Thompson RC. Molecular and morphological characterization of Echinococcus granulosus of human and animal origin in Iran. Parasitology. 2002;125(Pt 4):367-73. [PubMed ID: 12403325].
-
3.
Tensaw IM. Hydatid cyst in children. Ann Ped Surg. 2010;6(2):98-104.
-
4.
Cherry J, Demmler-Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ. Feigin and Cherry's Textbook of Pediatric Infectious Diseases. Elsevier - Health Sciences Division; 2013.
-
5.
Mandell GL, Bennett JE, Dolin R. Principles and Practice of Infectious Diseases. Elsevier Books, Oxford; 2004.
-
6.
Sadjjadi SM. Present situation of echinococcosis in the Middle East and Arabic North Africa. Parasitol Int. 2006;55 Suppl:S197-202. [PubMed ID: 16337429]. https://doi.org/10.1016/j.parint.2005.11.030.
-
7.
Rokni MB. The present status of human helminthic diseases in Iran. Ann Trop Med Parasitol. 2008;102(4):283-95. [PubMed ID: 18510809]. https://doi.org/10.1179/136485908X300805.
-
8.
Vlad DC, Neghina AM, Dumitrascu V, Marincu I, Neghina R, Calma CL. Cystic echinococcosis in children and adults: a seven-year comparative study in western Romania. Foodborne Pathog Dis. 2013;10(2):189-95. [PubMed ID: 23336269]. https://doi.org/10.1089/fpd.2012.1281.
-
9.
Schantz PM, Kern P, Brunetti E. Echinococcosis. Tropical Infectious Diseases: Principles, Pathogens & Practice. 2011. p. 824-38. https://doi.org/10.1016/b978-0-7020-3935-5.00120-8.
-
10.
Celik M, Senol C, Keles M, Halezeroglu S, Urek S, Haciibrahimoglu G, et al. Surgical treatment of pulmonary hydatid disease in children: report of 122 cases. J Pediatr Surg. 2000;35(12):1710-3. [PubMed ID: 11101720]. https://doi.org/10.1053/jpsu.2000.19219.
-
11.
Beggs I. The radiology of hydatid disease. AJR Am J Roentgenol. 1985;145(3):639-48. [PubMed ID: 3895873]. https://doi.org/10.2214/ajr.145.3.639.
-
12.
Karaoglanoglu N. Giant hydatid lung cysts. European Journal of Cardio-Thoracic Surgery. 2001;19(6):914-7. https://doi.org/10.1016/s1010-7940(01)00687-x.
-
13.
Khan RA, Wahab S, Chana RS, Fareed R. Isolated retroperitoneal hydatid cyst in a child: a rare cause of acute scrotal swelling? J Pediatr Surg. 2010;45(8):1717-9. [PubMed ID: 20713227]. https://doi.org/10.1016/j.jpedsurg.2010.04.019.
-
14.
Mirshemirani A, Razavi S, Sadeghian N. Surgical treatment of pulmonary hydatid cyst in 72 children. Tanaffos. 2009;8(1):56-61.
-
15.
Muller R, Wakelin D. Worms and Human Disease. 2002. https://doi.org/10.1079/9780851995168.0000.
-
16.
Brunetti E, White ACJ. Cestode infestations: hydatid disease and cysticercosis. Infect Dis Clin North Am. 2012;26(2):421-35. [PubMed ID: 22632647]. https://doi.org/10.1016/j.idc.2012.02.001.
-
17.
Chaouachi B, Ben Salah S, Lakhoua R, Hammou A, Gharbi HA, Saied H. [Hydatid cysts in children. Diagnostic and therapeutic aspects. Apropos of 1195 cases]. Ann Pediatr (Paris). 1989;36(7):441-4. 447-9. [PubMed ID: 2817698].
-
18.
Djuricic SM, Grebeldinger S, Kafka DI, Djan I, Vukadin M, Vasiljevic ZV. Cystic echinococcosis in children - the seventeen-year experience of two large medical centers in Serbia. Parasitol Int. 2010;59(2):257-61. [PubMed ID: 20206293]. https://doi.org/10.1016/j.parint.2010.02.011.
-
19.
Şehitoǧulları A. Our results in surgical treatment of hydatid cyst of the lungs. Eur J General Med. 2007;4(1):5-8.
-
20.
Vahedi MA, Vahedi ML. Demographics of patients with surgical and nonsurgical cystic echinococcosis in East Azerbaijan from 2001 to 2012. Pak J Biol Sci. 2012;15(4):186-91. [PubMed ID: 22816176].
-
21.
Ahmadi N, Dalimi A. Characterization of Echinococcus granulosus isolates from human, sheep and camel in Iran. Infect Genet Evol. 2006;6(2):85-90. [PubMed ID: 16503509]. https://doi.org/10.1016/j.meegid.2005.01.005.
-
22.
Talaiezadeh A, Paziar F. The factors of arteriovenous fistula failure in hemodialysis patient. Saudi Med J. 2006;27(1):114-6. [PubMed ID: 16432612].
-
23.
Oudni-M'Rad M, M'Rad S, Gorcii M, Mekki M, Belguith M, Harrabi I, et al. [Cystic echinococcosis in children in Tunisia: fertility and case distribution of hydatid cysts]. Bull Soc Pathol Exot. 2007;100(1):10-3. [PubMed ID: 17402685].
-
24.
Col C, Col M, Lafci H. Unusual localizations of hydatid disease. Acta Med Austriaca. 2003;30(2):61-4. [PubMed ID: 12752092].
-
25.
Dopchiz MC, Elissondo MC, Andresiuk MV, Maiorini E, Gutierrez AM, Muzulin PM, et al. Pediatric hydatidosis in the south-east of the Buenos Aires province, Argentina. Rev Argent Microbiol. 2009;41(2):105-11. [PubMed ID: 19623901].
-
26.
Moreno J, Tellez CJ, Pardo FJ. [Hydatid disease in the Department of Health #2 of the Valencian Community (Spain)]. Rev Esp Quimioter. 2009;22(2):62-7. [PubMed ID: 19544098].
-
27.
Hamamci EO, Besim H, Korkmaz A. Unusual locations of hydatid disease and surgical approach. ANZ J Surg. 2004;74(5):356-60. [PubMed ID: 15144257]. https://doi.org/10.1111/j.1445-1433.2004.02981.x.
-
28.
Prousalidis J, Tzardinoglou K, Sgouradis L, Katsohis C, Aletras H. Uncommon sites of hydatid disease. World J Surg. 1998;22(1):17-22. [PubMed ID: 9465756].
-
29.
Tsaroucha AK, Polychronidis AC, Lyrantzopoulos N, Pitiakoudis MS, Karayiannakis AJ, Manolas KJ, et al. Hydatid disease of the abdomen and other locations. World J Surg. 2005;29(9):1161-5. [PubMed ID: 16088421]. https://doi.org/10.1007/s00268-005-7775-3.
-
30.
Zahawi HM, Hameed OK, Abalkhail AA. The possible role of the age of the human host in determining the localization of hydatid cysts. Ann Trop Med Parasitol. 1999;93(6):621-7. [PubMed ID: 10707107].
-
31.
Ernest E, Nonga HE, Kynsieri N, Cleaveland S. A retrospective survey of human hydatidosis based on hospital records during the period 1990-2003 in Ngorongoro, Tanzania. Zoonoses Public Health. 2010;57(7-8):e124-9. [PubMed ID: 19968843]. https://doi.org/10.1111/j.1863-2378.2009.01297.x.
-
32.
Sarkari B, Sadjjadi SM, Beheshtian MM, Aghaee M, Sedaghat F. Human cystic echinococcosis in Yasuj District in Southwest of Iran: an epidemiological study of seroprevalence and surgical cases over a ten-year period. Zoonoses Public Health. 2010;57(2):146-50. [PubMed ID: 19175567]. https://doi.org/10.1111/j.1863-2378.2008.01200.x.
-
33.
Rostami Nejad N, Hoseinkhan N, Nazemalhosseini E, Cheraghipour K, Abdinia E, Zali MR. An analysis of hydatid cyst surgeries in patients referred to hospitals in Khorram-Abad, Lorestan during 2002–06. Iranian J Parasitol. 2007;2:29-33.
-
34.
Talaiezadeh AH, Maraghi S. Hydatid disease in children: A different pattern than adults. Pakistan J Med Sci. 2006;22(3):329-32.
-
35.
Al-Shibani LA, Al-Eryani SM, Azazy AA, Al-Mekhlafi AM. Cases of hydatidosis in patients referred to Governmental hospitals for cyst removal in Sana'a City, Republic of Yemen. Trop Biomed. 2012;29(1):18-23. [PubMed ID: 22543599].
-
36.
Safioleas M, Misiakos EP, Dosios T, Manti C, Lambrou P, Skalkeas G. Surgical treatment for lung hydatid disease. World J Surg. 1999;23(11):1181-5.
-
37.
Ahmadi NA, Hamidi M. A retrospective analysis of human cystic echinococcosis in Hamedan province, an endemic region of Iran. Ann Trop Med Parasitol. 2008;102(7):603-9. [PubMed ID: 18817601]. https://doi.org/10.1179/136485908X337517.
-
38.
Gonlugur U, Ozcelik S, Gonlugur TE, Arici S, Celiksoz A, Elagoz S, et al. The retrospective annual surgical incidence of cystic echinococcosis in Sivas, Turkey. Zoonoses Public Health. 2009;56(5):209-14. [PubMed ID: 19068075]. https://doi.org/10.1111/j.1863-2378.2008.01186.x.
-
39.
Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13(2):125-33. [PubMed ID: 18938096]. https://doi.org/10.1016/j.ijid.2008.03.037.