Abstract
Introduction:
The novel coronavirus has been shown to infect many bodily organs. Recent studies have suggested that the virus may be capable of causing inappropriate thrombosis formation. In the present case study, we present a pregnant patient who had severe pneumonia caused by the virus; and subsequently developed pulmonary thromboembolism.Case Presentation:
A 39-year-old primi-gravid pregnant woman presented to the emergency department with moderate to severe respiratory symptoms and tested positive for SARS-CoV-2. The patient was hospitalized and received routine treatment. The patient had a rapid deterioration of clinical signs and symptoms, coupled with sensations of palpitations and chest discomfort. The patient had an echocardiogram, which was suggestive of right ventricular strain. D-dimer tested positive, and the patient had a CT angiography, showing filling defects in branches of the pulmonary arteries.Conclusions:
Pulmonary thromboembolism may be a complicating factor in patients with severe viral pneumonia. In patients with underlying procoagulant conditions, such as pregnancy, the occurrence of Pulmonary Thromboembolism (PTE) should be strongly considered.Keywords
1. Introduction
The viral pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is characterized by varying degrees of lower respiratory tract symptoms, encompassing a wide range of clinical presentations; with most patients experiencing mild to moderate symptoms such as coughs, myalgia, rigor, gastrointestinal disturbances and myalgia (1).
It has been suggested that the virus may affect other bodily systems and normal organ functions, including but not limited to the hepatobiliary system, nervous system, and myocardium (2, 3). It has also been suggested that the virus can affect the inflammatory system and Interfere with the normal immune responses, subsequently leading to conditions such as severe inflammatory response syndrome and diffuse intravascular coagulation (4). Considering the possibility of the latter and the relation between the inflammatory cascade and coagulation cascade (5), it has been hypothesized that SARS-CoV-2 could contribute to the inappropriate formation of thrombosis (6). In the present report, we present the case of a pregnant patient who, subsequent to coronavirus disease 2019 (COVID-19), developed pulmonary artery thromboembolism.
2. Case Presentation
A pregnant 39-year-old Gravid 1, parity 1 G1P1 women presented to the Emergency Department with progressive dyspnea starting 6 days ago, coupled with a fever of 38°C. The gestational age was 34 weeks, based on a first-trimester ultrasonography. The patient had a non-significant past medical history and did not have a history of complications related to the current pregnancy. The patient was a non-smoker, did not partake in alcohol or recreational drugs, and was not on any specific medication. The patient was hospitalized for blood workup and further evaluation. Upon admission, the blood oxygen saturation in ambient air was 90 percent; as a result, the patient was put on 4 liters of oxygen per minute by nasal cannula. During the physical examination, we noted that the patient had diffuse crackles osculated in both lungs. Both S1 and S2 sounds were heard, and no murmurs existed. The blood workup showed a decreased white blood cell and leukocyte count (2.91, 0.37, respectively). Blood cultures were negative and the patient had a normal urine analysis. More detailed lab data is presented in Table 1.
Biochemical Test Results of the Patient
| Test | Results |
|---|---|
| WBC (1000/mm3) | 2.91 |
| Lymphocyte count (1000/mm3) | 0.37 |
| Platelet (1000/mm3) | 103 |
| Hemoglobin (gr/dL) | 9.6 |
| RBC count (106 /mm3) | 2.74 |
| TSH (IU/L) | 0.87 |
| Free T4 (ng/dL) | 1.04 |
| Lupus anti-coagulant | Negative |
| ALT (IU/L) | 29 |
| Total Bili (mg/dL) | 1.26 |
| Urea (mg/dL) | 51 |
| Creatinine (mg/dL) | 1.1 |
| Albumin (gr/dL) | 3.34 |
| Ck-Mb (IU/L) | 30.9 |
| Troponin | Negative |
| Ca (mg/dL) | 7.67 |
| Mg (mg/dL) | 2.26 |
| Anti-ds-DNA (IU/mL) | Negative |
| SGPT (IU/L) | 14 |
| Direct Bili (mg/dL) | 0.48 |
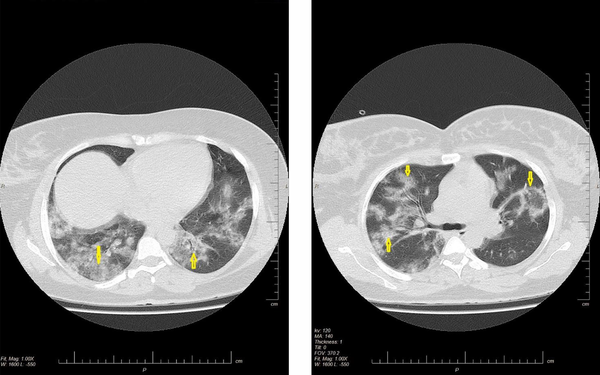
After consultation with the infectious disease ward, the possibility of infection with SARS-CoV-2 was suggested. At which point, we conducted a CT scan that showed bilateral multifocal patchy ground glass opacities. The patient also had 2 specimens collected from the nasopharynx and oropharynx, which tested positive for COVID-19. The patient was then isolated in a negative pressure room and was put on hydroxychloroquine 200 BID.
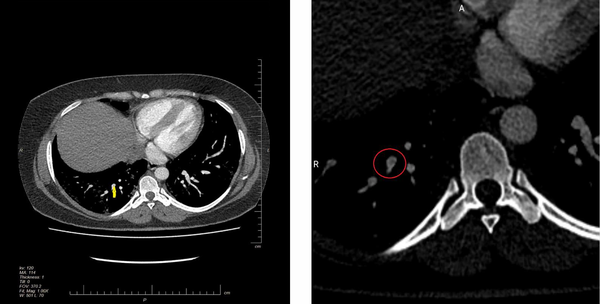
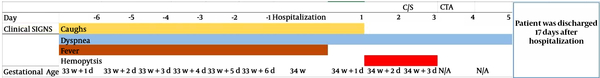
On the second day of admission, the patient developed hemoptysis and had greater breathing difficulties. Additionally, the blood oxygen saturation had become 82 percent in ambient air, and the patient was receiving oxygen by a mask with a reservoir bag. A consultation was made with the gynecologic and internal medicine wards in regard to next treatment steps. We performed a biophysical profile for the fetus and obtained a score of 10 out of 10. The patient was put on intravenous immunoglobulin by an internist doctor. On the second day of admission, the patient deteriorated at nighttime, and oxygen saturation remained below 82 percent amid oxygen therapy with 7 liters of oxygen provided via mask with a 2-liter reservoir. At this point, we proceeded with an emergency Cesarean section. The patient was then admitted into an intensive care unit (ICU). The patient complained of heartbeat palpitation and mild discomfort in her chest. An ECG showed an S wave in the lead I, q wave in lead II and sinus tachycardia, suggestive of right ventricle straining. The patient had a transthoracic echocardiography, which showed an ejection fraction of 45% - 50%. Severe right ventricle enlargement was also evident, with moderate to severe dysfunction of the right ventricle. A consultation with the Cardiology Department suggested further investigation to rule out pulmonary embolism. The patient was immediately put on low molecular weight heparin, and a CT pulmonary angiography was performed. The results illustrated filling defects and confirmed the diagnosis of pulmonary thromboembolism. The patient was then re-admitted to the ICU where treatment was continued. On the second day of ICU admission, the patient had oliguria for more than 12 hours; a consultation conducted with the Nephrology Department suggested that hemoperfusion should be performed. Following the hemoperfusion procedure, the patient was stabilized. The findings of the imaging studies are presented in Figures 1 and 2, with the clinical course of the patient presented in Figure 3.
Axial non-contrast HRCT scan of chest shows bilateral diffuse mixed ground glass and alveolar consolidation in left and right upper and lower lobe
Axial contrast enhance computed tomographic angiography shows small filling defect in right descending pulmonary artery
Clinical course of the patient
3. Discussion
The emergence of the COVID-19 pandemic has caused fatalities to reach the tens of thousands worldwide. The first set of evidence reported from clinical studies suggested that the main cause of mortality was a combination of respiratory failure and systemic inflammatory response syndrome. Subsequently, most of the therapies were directed against the aforementioned difficulties (7). However, more recent studies suggest that the virus could also affect the circulatory system; with case reports suggesting that the virus causes myocarditis, in addition to affecting the pump function of the left ventricle (8). Additionally, there is echocardiographic evidence that suggests that the virus can even have an effect on the function of the right ventricle. A limited number of case reports have suggested that one of the mechanisms resulting in this loss of function could be pulmonary thromboembolism, leading to right ventricle straining. Xie et al. presented two cases of patients with COVID-19, who deteriorated and had elevated D-dimer levels. The patients developed signs of pulmonary thromboembolism PTE in their second and sixth day of hospitalization, and were subsequently put on therapy. Both patients had moderate to severe bilateral lung involvement prior to the PTE (9). Danzi et al. reported the case study of a 75-year-old patient with severe bilateral involvement, with signs of infarct in the basal regions of the right ventricle. An echocardiography showed a hypokinetic right ventricle and a mean pulmonary artery pressure of 60 mmHg (10). More concrete evidence of this is presented in a study conducted by Klok et al. (11). They found that out of the 184 patients hospitalized in the ICU due to COVID-19, 31% (95%CI: 17% - 37%) showed signs of thrombotic disease, with pulmonary thromboembolism being the most common. All of the patients included in the study had received standard doses of prophylactic anticoagulants, but had developed thrombotic events regardless. Thus, the authors concluded that high-dose prophylaxis should be considered for these patients (11).
It is important to note that pregnant patients have an increased susceptibility to thrombosis formation, and any further pro-thrombosis factors may severely predispose them to inappropriate thrombosis formation (12). Clinicians should pay more attention to the acute deterioration of COVID-19 pneumonia in pregnant patients, as it may represent a potentially life-threatening condition such as PTE.
References
-
1.
Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. Jama. 2020.
-
2.
Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain, Behavior, and Immunity. 2020.
-
3.
Zhang C, Shi L, Wang F. Liver injury in COVID-19: management and challenges. The Lancet Gastroenterology & Hepatology. 2020.
-
4.
Wang YD, Zhang SP, Wei QZ, Zhao MM, Mei H, Zhang ZL, et al. COVID-19 complicated with DIC: 2 cases report and literatures review. Zhonghua xue ye xue za zhi= Zhonghua xueyexue zazhi. 2020;41. E001.
-
5.
Oikonomopoulou K, Ricklin D, Ward PA, Lambris JD, editors. Interactions between coagulation and complement—their role in inflammation. Seminars in immunopathology. Springer; 2012. p. 151-65.
-
6.
Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. Journal of Clinical Virology. 2020:104362. https://doi.org/10.1016/j.jcv.2020.104362.
-
7.
Shi Y, Wang Y, Shao C, Huang J, Gan J, Huang X, et al. COVID-19 infection: the perspectives on immune responses. Cell Death & Differentiation. 2020;27:1451-4.
-
8.
Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA cardiology. 2020.
-
9.
Xie Y, Wang X, Yang P, Zhang S. COVID-19 Complicated by Acute Pulmonary Embolism. Radiology: Cardiothoracic Imaging. 2020;2(2). e200067.
-
10.
Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? European Heart Journal. 2020.
-
11.
Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thrombosis Research. 2020. https://doi.org/10.1016/j.thromres.2020.04.013.
-
12.
Katz D, Beilin Y. Disorders of coagulation in pregnancy. BJA: British Journal of Anaesthesia. 2015;115(suppl_2):ii75-88.
