Abstract
Objectives:
This study aimed to assess the outcome and mortality predictors of SARS-CoV-2 infection requiring hospitalization among elderly population.Methods:
In this retrospective study, hospitalized elderly people with virologically confirmed SARS-CoV-2 infection were evaluated. Participants were divided into three groups of mild, moderate, and severe based on oxygenation. The primary outcome was death or discharge to home.Results:
A total of 169 patients were studied (mean age: 68 years). Apart from respiratory symptoms, other reported symptoms included gastrointestinal complaints in 11% (n = 19), acute stroke in 1.1% (n = 2), delirium in 1.7% (n = 3), and anosmia or ageusia in 8.88% (n = 15). Also, 65 (38.5%) patients required oxygen support, 25 (14.7%) were admitted to the intensive care unit (ICU), 7 (4.1%) required non-invasive ventilation (Fio2 0.6 to 1.0), 14 (8.28%) were mechanically ventilated. 72 (42%) received steroid, and 100 (59%) received prophylactic heparin. Overall mortality was 12.4% (n = 21). Gender had no effect on mortality (P = 0.83). Presence of ≥ 3 risk factors, elevated neutrophil lymphocyte ratio, D-dimer, and lactate dehydrogenase, were associated with mortality (P = 0.001, P = 0.0005, P = 0.05, and P = 0.0005, respectively). Sepsis and cardiovascular events were higher among those who died.Conclusions:
We observed a low mortality among the elderly treated with steroids compared to studies done in the pre-steroid period. Elevated NLR, LDH, and D-dimer were associated with mortality.Keywords
1. Background
Old age is a major risk factor for poor survival after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (1, 2). The elderly people, especially men, have had a high case fatality rate (2, 3). Aging leads to many anatomical and physiological changes in the respiratory tract, such as progressive decrease in the number of cilia and ciliated airway cells, as well as an increase in nasal cavity volume (4, 5). Dysregulated immune response in the elderly occurs as a result of immunological alterations with increased production of inflammatory mediators and cytokines, known as ‘Inflammaging', and impaired expression and downstream signaling of Toll-like receptors (6, 7). Male gender related aberrant methylation of the ACE2 promoter and inverted CD4/CD8 T-cell ratio may be responsible for the differential response in men (8, 9). These factors, along with multiple preexisting chronic medical illness make them more susceptible to severe SARS-CoV-2 illness (4, 5). The mortality of the illness among elderly people ranges from 19.2% to 96%, with the majority of deaths in the age group of above 80 years (2, 10). Most of these reports were published early during the pandemic when only supportive therapy was used. There is paucity of data from South Asia on hospitalization outcomes among elderly people.
2. Objectives
This study reports a single-center observation on severity and outcomes of SARS-Co-V-2 among elderly.
3. Methods
This retrospective study was conducted in a tertiary care teaching hospital in Chennai, India, from May 13 and July 31, 2020. A total of 169 hospitalized patients (aged ≥ 60 years) with confirmed SARS-CoV-2 infection by reverse transcription polymerase chain reaction (RT-PCR) of nasopharyngeal swab were included. The patients were divided into three groups (mild, moderate, and severe). Mild infection was defined as presence of one or more symptoms of SARS-coV-2 infection with no features of pneumonia and oxygen saturation > 94% on room air. Moderate infection was defined as presence of oxygen desaturation ≤ 94%, but ≥ 90%. Severe infection was defined as oxygen saturation < 90%. Those who died or were discharged within 24 hours of admission were excluded. All variables including age, gender, clinical symptoms, investigations, radiological features, requirement for intensive care or high dependency care, duration of hospital stay, complications, and outcomes were recorded. Primary outcome was defined as death or discharge from hospital to home. Patients were considered to have prolonged hospital stay if they required more than 10 days of hospitalization. Difference in baseline characteristics between groups were compared using unpaired t-test, chi-square test, Fischer’s exact test, and analysis of variance (ANOVA) as applicable. Variables associated with severe illness were done using multivariate analysis by one-way ANOVA (MANOVA) followed by Tukey's honest significance test (HSD). The receiver operator characteristic (ROC) curve analysis was used to find the sensitivity and specificity of the variables associated with mortality. Analysis was done using SPSS software version 23.0, and P-value < 0.05 was considered as statistically significant. The study was approved with waiver of consent by Institutional Ethics Committee [IEC-NI/AUG/20/75/54].
4. Results
In this study, a total of 169 patients were included. Table 1 describes the baseline characteristics of the patients in three groups. The mean age of patients was 68 ± 7.9 years, 23 (13.6%) aged ≥ 80 years (mild-13, moderate-4, severe-6), and the majority (59.8%) of patients were male. There was no significant difference in age (P = 0.07) or gender (P = 0.8) between the groups. Also, 135 (80%) had at least one preexisting medical illness, with diabetes mellitus as the most common (59.6%). Diabetes was more prevalent in moderate and severe groups (P = 0.004). Coronary artery disease (CAD) was more prevalent in severe group (P = 0.004). Table 2 elaborates the presenting features of study participants. Two patients in severe category had an acute stroke as the initial presentation. The mean days after onset of symptoms to presentation was 4.69 days with no significant difference observed across groups (P = 0.22). Neutrophil lymphocyte ratio (NLR) and ferritin were significantly higher in severe illness (P = 0.005). Serum albumin (P = 0.0005) and serum sodium (P = 0.001) had a significant difference between groups; this might be of little clinical significance relevance since the mean serum albumin, and serum sodium values across all three groups were > 3g/dL and > 130meq/L, respectively. In addition, 65 (38.5%) patients required oxygen support, 25 (14.7%) patients were admitted to the intensive care unit (ICU) of whom 7 (4.1%) required non-invasive ventilation (with Fio2 0.6 to 1.0), and 14 (8.28%) patients were mechanically ventilated.
| Clinical Parameter | Mild (N = 104) | Moderate (N = 38) | Severe (N = 27) | P Value* |
|---|---|---|---|---|
| Age in years | 68.3 ± 7.8 | 68 ± 7.1 | 72 ± 9 | 0.07 |
| Gender | 0.82 | |||
| Male | 64 (61.5) | 22 (57.9) | 15 (55.6) | |
| Female | 40 (38.5) | 16 (42.1) | 12 (44.4) | |
| Comorbidities | ||||
| Diabetes mellitus | 52 (50) | 28 (77.8) | 19 (73.1) | 0.004 |
| Coronary artery disease | 13 (12.5) | 5 (13.2) | 12 (44.4) | 0.004 |
| Hypertension | 56 (53.8) | 21 (56.8) | 19 (70.4) | 0.3 |
| Chronic lung disease | 4 (3.8) | 0 (0) | 3 (4.1) | - |
| Others | 1 (0.9) | 3 (7.8) | 6 (22) | - |
| Day of illness on presentation, day | ||||
| Mean ± SD | 4.5 ± 2.8 | 4.4 ± 3.0 | 5.5 ± 3.0 | 0.22 |
| Median | 4.5 | 4.0 | 6.0 | |
| Investigations | ||||
| NLR | 3 ± 2.1 | 5.8 ± 6.6 | 12.0 ± 12.9 | 0.0005 |
| S. Ferritin (ng/mL) | 161 ± 146.3 | 322 ± 241.7 | 663 ± 1318.8 | 0.0003 |
| LDH (IU/L) | 261 ± 71.2 | 412 ± 240.9 | 477 ± 279.1 | 0.0005 |
| Sodium (meq/L) | 135 ± 4.8 | 133 ± 4.2 | 131 ± 4.6 | 0.001 |
| Albumin (g/d) | 3.7 ±0.4 | 3.4 ±0.3 | 3.2 ±0.6 | 0.0005 |
| D-Dimer (mg/L) | 0.05 | |||
| < 0.5 | 59 (56.7) | 8 (21) | 6 (22.2) | |
| 0.5 - 1 | 23 (22.1) | 8 (21) | 8 (29.6) | |
| 1.01 - 2 | 8 (7.6) | 8 (21) | 8 (29.6) | |
| 2.01- 4 | 5 (4.8) | 7 (18.4) | 1 (3.7) | |
| > 4 | 2 (1.9) | 6 (15.7) | 4 (14.8) | - |
| Chest X-ray | ||||
| Normal | 50 (48) | 8 (21) | 1 (3.7) | |
| Single lobar opacities | 8 (7.69) | 3 (7.8) | 4 (14.8) | |
| Multi-lobar opacities | 43 (41) | 27 (71) | 22 (81.4) |
| Symptoms | Mild (N = 104) | Moderate (N = 38) | Severe (N = 27) |
|---|---|---|---|
| Asymptomatic | 12 (11.5) | 2 (5) | 0 (0) |
| Fever | 70 (67) | 30 (79) | 18 (66.6) |
| Shortness of breath | 8 (7.6) | 15 (39) | 18 (66.6) |
| Cough | 30 (29) | 21 (55) | 12 (44) |
| Sore throat | 30 (29) | 5 (13) | 0 (0) |
| Myalgia or fatigue | 17 (16) | 5 (13) | 3 (11) |
| Anosmia or ageusia | 12 (11.5) | 0 (0) | 3 (11) |
| Vomiting or diarrhoea | 9 (8.6) | 3 (7.8) | 7 (26) |
| Others b | 0 (0) | 0 (0) | 3 (11.1) |
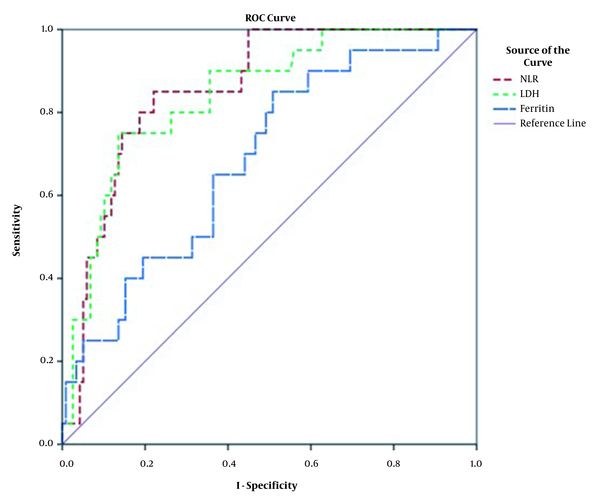
Complications during stay were bacterial sepsis (n = 16), fungal sepsis (n = 4), and cardiovascular events (n = 8). Pathogens isolated in patients with bacterial sepsis were Klebsiella (n = 8), Acinetobacter (n = 6), Escherichia (n = 4), Pseudomonas (n = 3), methicillin resistant Staphylococcus aureus (MRSA, n = 1), and coagulase negative Staphylococcus aureus (CONS, n = 1). Medications used were dexamethasone or methylprednisolone (n = 72), heparin (n = 100), remdesivir (n = 11), meropenem (n = 11), piperazillin tazobactum (n = 10), colistin or polymyxin (n = 9), vancomycin (n = 3) and caspofungin (n = 3). The mean duration of hospital stay was 10 days. However, the stay was 18.8 days for those with bacterial sepsis and 16.5 days when complicated by cardiovascular event. Overall mortality was 12.4% (n = 21). All the six patients aged above 80 years had severe illness, 14 of 16 patients who had bacterial sepsis, and seven of eight patients with cardiovascular event died. Non-survivors were older (mean age: 72 years) compared to survivors (mean age: 68 years) (P = 0.02). While gender had no effect on mortality (P = 0.83), presence of ≥ 3 risk factors was associated with mortality (P = 0.001). Admission Spo2 of 94% had sensitivity of 76% and specificity of 74% in predicting mortality (area under curve AUC = 0.833, P = 0.0005). Raised D-dimer was not significantly associated with mortality (P = 0.05), though a trend towards mortality was observed. NLR of 5.34 had a sensitivity of 81% and specificity of 80% in predicting mortality (AUC = 0.857, P = 0.0005). LDH of 361 (IU/L) had a sensitivity of 76.2% and specificity of 76% in predicting mortality (AUC = 0.842, P = 0.0005). Figure 1 shows the ROC curve analysis for variables NLR, LDH, and Ferritin.
Shows receiver operating characteristic (ROC) curve analysis for variables NLR, LDH and Ferritin. NLR (AUC-0.857, P = 0.0005, cut off value 5.34, sensitivity 81%, specificity 80.9%); LDH (AUC-0.842, P = 0.0005, cut off value 361U/L, sensitivity 76%, specificity 76%).
5. Discussion
The coronavirus disease 2019 (COVID-19) pandemic has had a devastating effect on the elderly with high mortality rates in population above 80 years (2, 10). Our mortality rate of 12.4% was lower compared to an early study of 339 elderly patients from China, which reported survival of 65 of 156 (41.6%) patients for whom outcome of death or discharge to home was known (2). The latter had a higher prevalence of hypertension (40%), lower diabetes mellitus (16%), more severe or critically ill patients (70%), and 42% had bacterial sepsis. The mortality in our study was low despite 80% having at least one preexisting medical illness and 60% having diabetes mellitus. We did not find any gender differences, unlike previous studies, which found men to be at risk for increased mortality (1-3).
A review of mortality among patients aged ≥60 years reported that this age group formed 96.4% (1567 of 1625) of SARS-CoV-2 deaths in Italy and 81% (829 of 1023) of deaths in China during early phase of the pandemic (10). Our center had 30 deaths during the study period across all age groups, of whom 21 (70%) were aged ≥ 60 years.
In RECOVERY trial, dexamethasone was the first drug found to reduce mortality in SARS-CoV-2 infection observing an absolute reduction in mortality of 2.8%, which was subsequently confirmed in meta-analysis of seven randomized controlled trials which observed that use of low-dose steroids (dexamethasone, methyl prednisolone, or hydrocortisone) reduced odds of death (Odds Ratio = 0.66) (11, 12). Since most of our patients were admitted after May 2020, when the beneficial effects of steroids on critically ill and those needing oxygen had begun to be known, all the elderly in moderate and severe groups were treated with low-dose steroids.
Risk of thrombosis is increased in elderly people due to age related endothelial dysfunction, presence of multiple comorbidities, platelet hyperactivity, and changes in platelet function. Early data showed increased risk of thrombosis associated with SARS-CoV-2 infection, and heparin (unfractionated or low molecular weight) administration appeared to lower mortality by 20% (13). This led to our practice changing policy of giving prophylactic heparin to all elderly patients who had either an elevated D-dimer or required oxygen support. The reported incidence of acute stroke among COVID-19 patients varies between 1 - 3% (14). Acute ischemic stroke event observed in our study was 1.1%.
Elevated NLR due to neutrophilia and lymphocytopenia predicts poor outcomes. We found significant increasing trend in NLR among severe versus non-severe illness. LDH, an immunosurveillance biomarker released into circulation following cell lysis. LDH promotes action of immunosuppressive cells like dendritic cells and inhibits action of cytolytic T cells and natural killer (NK) cells. This tilt in balance blunts immune response mounted against viral clearance; hence, elevated LDH portends poor outcomes (15, 16). In our study, we found significantly elevated LDH and ferritin in severe illness, but stronger association with mortality was observed with increased LDH than ferritin.
The possible factors leading to lower mortality in our study are a) clinical presentation < 5 days from onset of symptoms enabling appropriate monitoring and oxygen support, b) lower age with lower percentage of population aged ≥ 80 years, and c) lower percentage of secondary infections complicating the illness, d) administration of steroids in all patients needing supplementary oxygen and, e) prophylactic administration of heparin in high-risk group.
The second wave of the pandemic in India started in early half of March 2021, and consistent with all urban regions in India, our center witnessed a shift in age of hospitalized patients, with younger patients aged between 30 and 59 years presenting with hypoxic pneumonia. At a national level, the weekly mortality average was more than 21000 in the first week of May 2021 (www.covid19india.org). In our hospital, 720 patients were hospitalized between February and April 2021, of whom 486 (67.5%) were younger than 60 years. A total of 20 patients died, of whom 5 (25%) were < 60 years and 15 (75%) were ≥ 60 years. During the same period, our region (Chennai) had 22,843 hospitalizations, of whom 14802 (64.8%) were younger than 60 years and 836 died. Also, 249 (29.7%) of deaths were reported in patients aged less than 60 years with majority of deaths (656 of 836 deaths) reported in April 2021 (https://stopcorona.tn.gov.in/daily-bulletin/). Compared to the first wave, younger age group (< 60 years) was more affected with no significant difference in the elderly population in the second wave.
Of the total population in India (136.64 crores), 6.5% is above 65 years of age and belongs to the vulnerable group. Vaccination is prioritized for the elderly in India from the public health perspective, considering the maximum mortality reported in elderly people.
5.1. Conclusions
The elderly people aged ≥ 60 years had a mortality of 12.4%. Most of the patients were referred to the hospital within seven days of illness. Those who had complications like sepsis and cardiovascular event had higher rates of death. The mortality rate was low compared to other studies, probably due to early hospitalization, lower secondary sepsis, and steroid use.
References
-
1.
Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. [PubMed ID: 32217618]. https://doi.org/10.1136/bmj.m1198.
-
2.
Wang L, He W, Yu X, Hu D, Bao M, Liu H, et al. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639-45. [PubMed ID: 32240670]. [PubMed Central ID: PMC7118526]. https://doi.org/10.1016/j.jinf.2020.03.019.
-
3.
Meng Y, Wu P, Lu W, Liu K, Ma K, Huang L, et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: A retrospective study of 168 severe patients. PLoS Pathog. 2020;16(4). e1008520. [PubMed ID: 32343745]. [PubMed Central ID: PMC7209966]. https://doi.org/10.1371/journal.ppat.1008520.
-
4.
Levitzky MG. Effects of aging on the respiratory system. Physiologist. 1984;27(2):102-7. [PubMed ID: 6374697].
-
5.
Xu J, Kang YA, Park SK, Yoon YH, Bai SJ, Jin Y, et al. Nasality Changes With Age in Normal Korean-Speaking Adults. Clin Exp Otorhinolaryngol. 2019;12(1):95-9. [PubMed ID: 30257547]. [PubMed Central ID: PMC6315219]. https://doi.org/10.21053/ceo.2018.00717.
-
6.
Aw D, Silva AB, Palmer DB. Immunosenescence: emerging challenges for an ageing population. Immunology. 2007;120(4):435-46. [PubMed ID: 17313487]. [PubMed Central ID: PMC2265901]. https://doi.org/10.1111/j.1365-2567.2007.02555.x.
-
7.
Aiello A, Farzaneh F, Candore G, Caruso C, Davinelli S, Gambino CM, et al. Immunosenescence and Its Hallmarks: How to Oppose Aging Strategically? A Review of Potential Options for Therapeutic Intervention. Front Immunol. 2019;10:2247. [PubMed ID: 31608061]. [PubMed Central ID: PMC6773825]. https://doi.org/10.3389/fimmu.2019.02247.
-
8.
Fan R, Mao SQ, Gu TL, Zhong FD, Gong ML, Hao LM, et al. Preliminary analysis of the association between methylation of the ACE2 promoter and essential hypertension. Mol Med Rep. 2017;15(6):3905-11. [PubMed ID: 28440441]. https://doi.org/10.3892/mmr.2017.6460.
-
9.
Gubbels Bupp MR. Sex, the aging immune system, and chronic disease. Cell Immunol. 2015;294(2):102-10. [PubMed ID: 25700766]. https://doi.org/10.1016/j.cellimm.2015.02.002.
-
10.
Onder G, Rezza G, Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020;323(18):1775-6. [PubMed ID: 32203977]. https://doi.org/10.1001/jama.2020.4683.
-
11.
Recovery Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693-704. [PubMed ID: 32678530]. [PubMed Central ID: PMC7383595]. https://doi.org/10.1056/NEJMoa2021436.
-
12.
W. H. O. Rapid Evidence Appraisal for COVID-19 Therapies Working Group, Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, et al. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA. 2020;324(13):1330-41. [PubMed ID: 32876694]. [PubMed Central ID: PMC7489434]. https://doi.org/10.1001/jama.2020.17023.
-
13.
Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18(5):1094-9. [PubMed ID: 32220112]. https://doi.org/10.1111/jth.14817.
-
14.
Merkler AE, Parikh NS, Mir S, Gupta A, Kamel H, Lin E, et al. Risk of Ischemic Stroke in Patients With Coronavirus Disease 2019 (COVID-19) vs Patients With Influenza. JAMA Neurol. 2020. [PubMed ID: 32614385]. [PubMed Central ID: PMC7333175]. https://doi.org/10.1001/jamaneurol.2020.2730.
-
15.
Zhang JJY, Lee KS, Ang LW, Leo YS, Young BE. Risk Factors for Severe Disease and Efficacy of Treatment in Patients Infected With COVID-19: A Systematic Review, Meta-Analysis, and Meta-Regression Analysis. Clin Infect Dis. 2020;71(16):2199-206. [PubMed ID: 32407459]. [PubMed Central ID: PMC7239203]. https://doi.org/10.1093/cid/ciaa576.
-
16.
De Smet R, Mellaerts B, Vandewinckele H, Lybeert P, Frans E, Ombelet S, et al. Frailty and Mortality in Hospitalized Older Adults With COVID-19: Retrospective Observational Study. J Am Med Dir Assoc. 2020;21(7):928-932 e1. [PubMed ID: 32674821]. [PubMed Central ID: PMC7280137]. https://doi.org/10.1016/j.jamda.2020.06.008.