Abstract
Keywords
1. Introduction
End stage renal disease (ESRD) patients have a predisposition to adverse infectious events because of overwhelming uremia, which is associated with alterations in primary host defense mechanisms and increases the risk of bacterial infections. Neutrophils exhibit impaired chemotaxis, oxidative metabolism, phagocytic activity, degranulation, intracellular killing and dysregulated programmed cell death. These immunologic abnormalities are complicated by the use of immunosuppressive drugs to treat and control underlying diseases and exacerbated by nutritional deficiencies, the dialysis procedure, and the disruption of cutaneous and mucosal barriers to infection (1). Hemodialysis patients, during the normal course of treatment, are exposed to several infectious risks, and the majority of patients require at least 1 hospitalization every year for treatment of infections (2). We report a bladder and urinary tract abscess discovered by hip arthritis in a hemodialysis patient.
2. Case Presentation
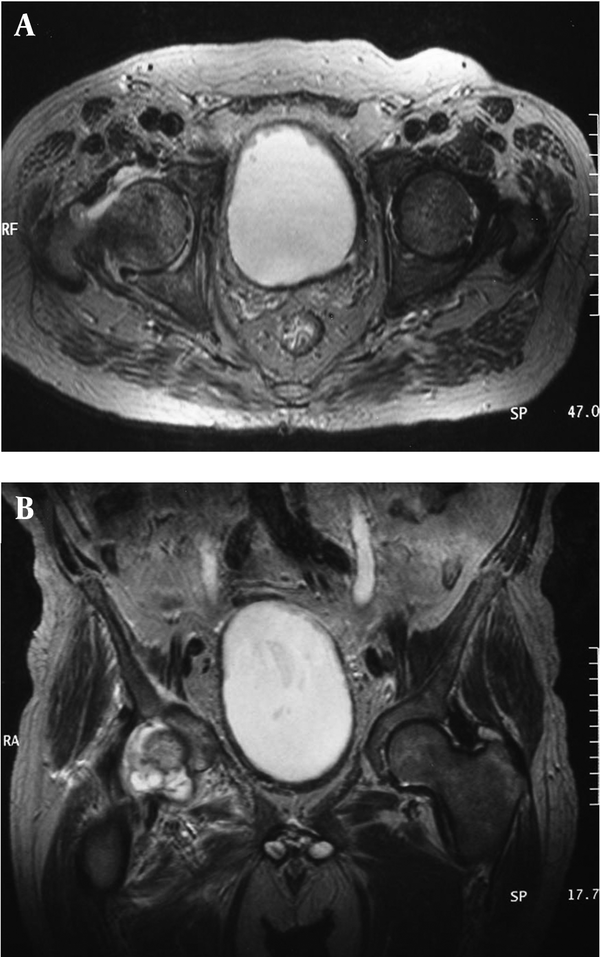
A 64-year-old man with a history of ESRD on chronic hemodialysis presented to our department with a two-month history of progressive dysuria, fever, asthenia and left hip pain. The anamnesis revealed that the patient had been hospitalized 6 months ago for diagnostic investigation of dysuria. At the time, he had received an urethrotomy for urethral stenosis and the urine was sterile. In our department, physical examination revealed normal blood pressure of 130/80 mmHg, temperature was 38.5°C and painful limitation of hip movements. The laboratory findings showed white blood cell (WBC) count of 18.5 x 109/L (reference range 4.0 - 10.0 x 109/L) and C-reactive protein (CRP) level of 115 mg/L (reference range < 2mg/L). Blood and urine cultures were negative. A hip radiography showed a diffuse bone demineralization. A hip magnetic resonance imaging (MRI) demonstrated long T1 and long T2 signal in bladder and left hip that suggested simultaneous bladder abscess and left hip arthritis (Figure 1).
Hip Magnetic Resonance Imaging (MRI) Shows Long T1 Signal in Bladder, Ureter and Left Hip, Suggesting Simultaneous Bladder Abscess and Left Hip Arthritis
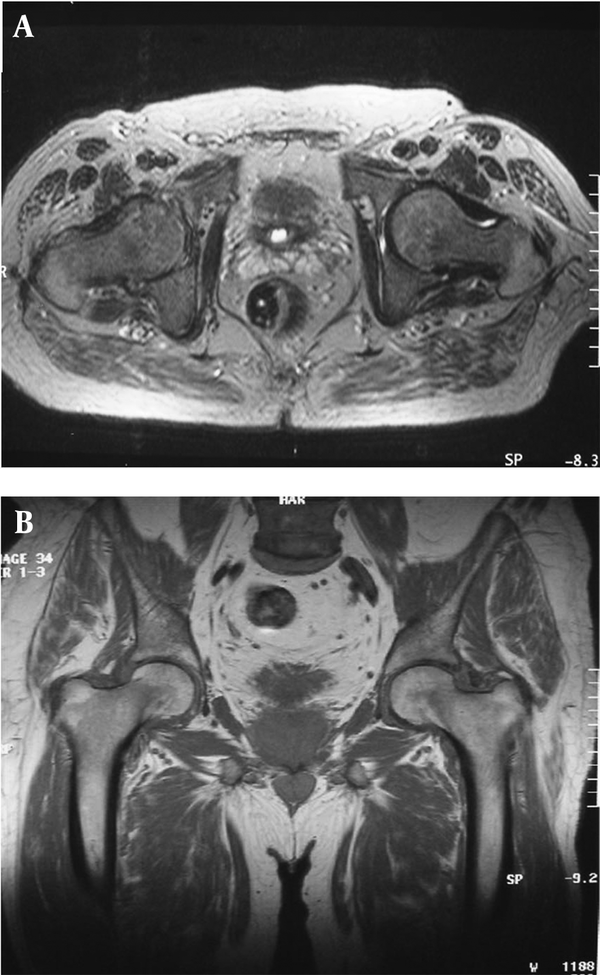
A synovial fluid leukocyte count of the hip was 9000/mm 3 and it consists of 87% neutrophils. The synovial fluid culture was negative. An endoscopic drainage of the bladder abscess after urethrotomy for urethral stenosis was performed on the third day of hospitalization. The abscess culture subsequently grew Pseudomonas aerogenosa. An adapted antibiotic treatment (Ceftriaxone, Amikacine and Ciprofloxacine) was introduced. Temperature had defervesced to 37.2 ºC and rapid recovery followed. The patient was discharged from the hospital after 3 weeks of intravenous antibiotic therapy. At her last follow-up visit, after 3 months under orally Ciprofloxacine, a hip MRI control showed a marked improvement with regression of joint effusion (Figure 2) and the patient was completely asymptomatic.
Hip Magnetic Resonance Imaging (MRI) Shows Regression of Hip Arthritis After Draining of Bladder Abscess
3. Conclusions
Infection is a common cause of morbidity and mortality in hemodialysis patients (3). Patients with ESRD on hemodialysis have documented defects in their immune responses and infections contribute significantly to their morbidity and mortality. Epidemiological studies suggest that ESRD patients have a higher risk of contracting bacterial infections and that the 3 most commonly seen infectious complications are urinary tract infections (UTI), pneumonia, and sepsis (1). Our case presents a very rare UTI case of complications that occur after urethrotomy and discovered by hip arthritis symptoms. We could not find a description of a similar case in the literature. The higher UTI susceptibility in the chronic kidney disease group may be explained, in part, by a greater incidence of urinary obstructions, which in turn leads to infections (4), commonly seen in those with benign prostatic hypertrophy, kidney stones and urinary tract cancers (5, 6). The urinary tract, which may not be recognized as an important source of infection among dialysis patients because of their minimal urine output (7), is responsible for the highest rates of hospitalization followed by pulmonary infections. This case study indicates that a urinary endoscopy must always be done under the most sterile and least traumatic conditions as possible especially in patients with ESRD on hemodialysis.
Acknowledgements
References
-
1.
Naqvi SB, Collins AJ. Infectious complications in chronic kidney disease. Adv Chronic Kidney Dis. 2006;13(3):199-204. [PubMed ID: 16815225]. https://doi.org/10.1053/j.ackd.2006.04.004.
-
2.
USRDS 1997 Annual Data Report. Bethesda, Maryland: National Institutes of Health, National institute of Diabetes and Digestive and Kidney Diseases; 1997.
-
3.
Atlas of End-Stage Renal Disease in the United States, USRDS 2000 Annual Data Report. Bethesda: MD, National Institute of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2000.
-
4.
Ishani A, Collins AJ, Herzog CA, Foley RN. Septicemia, access and cardiovascular disease in dialysis patients: the USRDS Wave 2 study. Kidney Int. 2005;68(1):311-8. [PubMed ID: 15954922]. https://doi.org/10.1111/j.1523-1755.2005.00414.x.
-
5.
Appel GB, Radhakrishnan J, D'Agati V. Secondary Glomerular Disease. In: Brenner BM, editor. Brenner & Rector's The Kidney. 6 ed. Philadelphia: W.B. Saunders; 2000. p. 1350-448.
-
6.
Asplin JR, Favus MJ, Coe FL. Nephrolithias. In: Brenner BM, editor. Brenner & Rector’s The Kidney. 6 ed. Philadelphia: W.B. Saunders; 2000. p. 1774-819.
-
7.
D'Agata E, Mount DB, Thayer V, Schaffner W. Hospital-acquired infections among chronic hemodialysis patients. Ame J Kidney Dis. 2000;35(6):1083-8.