1. Introduction
Hydatidosis is caused by Echinococcus, a tape worm, and is a worldwide zoonosis disease (1). While dogs or other carnivores are definitive, sheep or other ruminants are intermediate hosts for hydatid disease, and humans can become infected through contaminated food (2). Any organ can be affected by Echinococcus granulosus except hair and nails (3). While the liver is the most commonly involved site, unusual affected sites include the heart, ovary, fallopian tube, and thyroid gland (2, 4). Involvement of the peritoneal cavity is only seen in 12% of patients with previous hydatid cyst surgery or microrupture of hepatic cysts (2). In the past 20 years, in our country, omental and retroperitoneal involvement by hydatid disease is the third most uncommon sites of invasion. There are only less than ten cases of these type of involvement in our country in past 20 years.(5). These cysts usually remain asymptomatic until reaching a large size (5). In this report, we discuss a case of asymptomatic involvement of the peritoneum and liver with hydatid disease, which was incidentally discovered during a course of acute abdomen workup.
2. Case Presentation
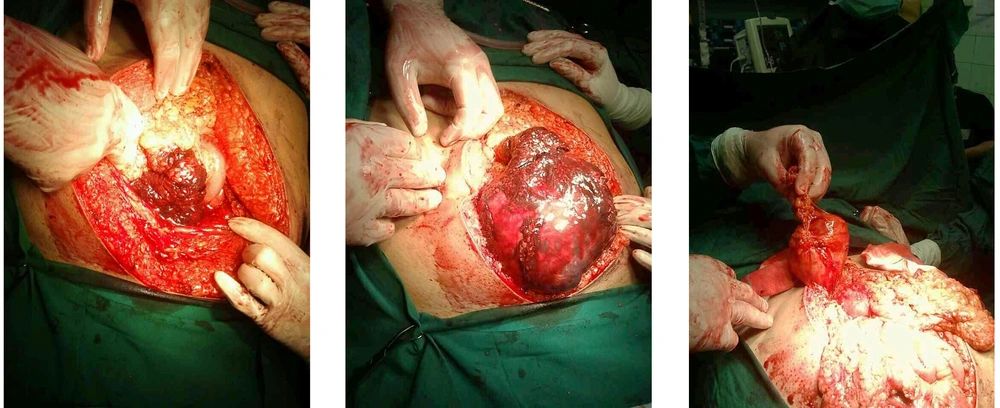
In early April 2015, a 40-year-old man was referred to the emergency department of Vasei hospital (Sabzevar, Iran) because of dull and intermittent abdominal pain, which started a week prior. The patient complained of anorexia, which was not accompanied with nausea or vomiting and began with the onset of pain. The pain was moderate in intensity and located in the periumbilical, left lower quadrant, and right lower quadrant regions. The patient did not have any history of medical illness in his life. The vital signs were normal except for a low-grade fever. In physical examination, moderate tenderness and rebound were identified with involuntary guarding over the entire lower half portion of the obese abdomen. The complete blood count and urinalysis were unremarkable. As the patient condition and abdominal pain worsened rapidly, open laparotomy was scheduled with the impression of peritonitis. After performing a midline incision, the whole abdomen was explored. Surprisingly, there were five omental cysts within different parts of the abdomen (Figure 1). The biggest cyst was located in the pelvis with an approximate diameter of 13 cm and was torted. Other cysts were located in the splenic flexure (6 cm) and between the transverse colon and stomach (6 cm), and the two others were laid approximately side by side in the hepatic flexure (3 cm and 6 cm). The cysts did not have any adhesion to adjacent structures and were sent for pathology. As the surgery became prolonged, the abdomen was closed after resecting an inflamed appendix. After the surgery, the patient stayed in the surgery ward for about three days, and the abdominal pain disappeared gradually. The pathology result of the removed cysts was consistent with a hydatid cyst. The patient underwent high-resolution computed tomography in order to evaluate the lungs for any hydatid cysts. While the lungs were clear, there were two simple cysts in the segments 7 and 8 of the liver. With the confirmed diagnosis of hydatid disease, the patient was discharged with oral 800 mg albendazole daily and advised for further reoperation of the remaining hepatic cysts. However, in the follow-up visit, the patient did not agree to undergo any further workups for the hepatic cysts.
3. Discussion
Hydatid disease is common in the Middle East and should be considered a dilemma in Iran (6, 7). A possible differential diagnosis of cystic mass lesions in endemic areas can be cystic hydatidosis (4, 8). History, imaging, and immunological tests may be used to assist physicians in order to confirm echinococcosis (8). Sheep and goats are two main animals that play an important role in transmitting this disease in Iran (9). The liver and lungs of these animals are the most infected organs (9). Our patient declared no direct contact with farm animals.
Bilateral hydatid cysts of the lungs and concomitant liver hydatid disease can occur in endemic areas, as in our case (10). It is reasonable to search for additional hydatids in patients who present either with liver or pulmonary involvement (11). While primary peritoneal hydatidosis is a rare finding, the liver was identified as the primary source of the disease in further searches of other sites (12). Abdominal hydatid disease is usually asymptomatic, and the possible reason for diagnosis in this patient was the torted cyst (12). Peritoneal hydatid disease is more likely to be seen in patients with previous hepatic surgery for echinococcosis, and the dissemination is mostly seen after blunt trauma (12). However, our case did not have any history of previous surgery or blunt trauma. It has also been reported that peritoneal cavity involvement can be caused by spontaneous and asymptomatic microrupture of hepatic cysts (2). Abdominal hydatid disease can present in various ways, but it rarely presents with acute abdominal pain because of torsion. Only Karagulle et al. (13) reported a case of torted hydatid cyst attached to the greater omentum with a peduncle. Lianos et al. (14) reported a case of multiple splenic echinococcosis in a 72-year-old Caucasian male, which presented as acute abdomen and abdominal distention. Their patient had huge hepatic cysts with multiple splenic hydatidosis (14). Ozalp et al. (15) reported a case of hydatid disease that presented with acute abdomen and ileus and abdominal distention. Their patient had a ruptured liver and many peritoneal cysts. The cyst completely obstructed the intestine (15). Shah et al. (12) reported a case of disseminated hydatid disease in a 45-year-old woman who presented with chronic dull aching pain. Their patient also had a palpable abdominal mass and positive history of blunt trauma five year prior. At the time of surgery, the peritoneal cavity was studded with 250 cysts. Despite removal of these cysts, their patient died from anaphylactic shock (12).
While pre- and postoperative medication will kill spilled scolices in the ruptured hydatid cysts, we did not start albendazole for our patient because of the acute abdomen and presence of other possible etiologies such as a complicated appendicitis (16). Medical treatment is recommended in patients with extensive disease (17). Albendazole and praziquantel is an effective therapy for treating hydatid cysts and an alternative to surgery for patients with disseminated hydatidosis (17). In patients who are going to have surgery, laparoscopic treatment is a less traumatic approach with better cosmetic outcomes (18). As previously noted, anaphylactic reaction is a possible serious complication of accidental cyst rupture and should be avoided. Rupture of these cysts is considered a serious complication because of chemical peritonitis and anaphylaxis (19). Intravascular spreading of the cyst contents can cause sudden death. Despite the hydatid cysts’ location, performing abdomen or thorax imaging is reasonable (20). Imaging should be repeated at least once in two years to detect possible recurrence (20). In conclusion, echinococcosis presents in different ways depending on the involved body organ. This disease should be considered as a differential diagnosis for acute abdomen in endemic areas. In our case, a huge torted cyst caused acute abdomen manifestations. It is important to keep in mind that even peritoneal involvement may be seen despite intact hepatic cysts. Careful excision of these cysts is the treatment of choice.