Abstract
Background:
A series of racial specific predictive equations for exercise parameters are needed to determine a lack of cardiopulmonary fitness or having an exercise limitation on cardiopulmonary exercise testing (CPET).Objectives:
The study aimed to develop a new set of predictive equations of CPET parameters during maximal cycling exercise for Thai adults.Methods:
A sample of 580 Thai adults whom could pass screening tests were asked to fill a health questionnaire and the Global Physical Activity questionnaire. Participants with history of symptomatic heart and pulmonary diseases, current smokers, history of smoking ≥ 10 pack-years, and abnormal spirometry were excluded. The CPET was performed using a cycle ergometer with an incremental symptom-limited protocol. Values of CPET parameters at the peak exercise (oxygen uptake [V̇O2], work rate, heart rate, oxygen pulse, and minute ventilation), lactic acidosis threshold, and ventilatory equivalents for oxygen and carbon dioxide were documented. Analyses were stratified using age and gender criterion. Predictive equations for CPET parameters were established using multivariable linear regression with age (A), weight (W), height (H), and physical activity level (Act) as independent variables.Results:
A total of 493 participants (208 men and 285 women) were analysed. The predictive equation of V̇O2peak (L.min-1) for males was: -2.268 + (0.037 × A) - (0.0005 × A2) + (0.016 × W) + (0.014 × H) + (0.104 × Act), (R2 = 0.41, SEE = 0.392), and for females, it was: -0.34 + (0.009 × A) - (0.0002 × A2) + (0.012 × W) + (0.005 × H) + (0.058 × Act), (R2 = 0.44, SEE = 0.220).Conclusions:
This is the first study that constructed the predictive equations for cycling CPET parameters in Thai adults. These equations are useful to evaluate the cardiopulmonary health of the Thai population and may be generalized to other populations with geographical or ethnic proximity to the Thai people.Keywords
Reference Values Cardiopulmonary Exercise Test Peak Oxygen Uptake Predictive Equations
1. Background
Cardiopulmonary Exercise testing (CPET) is widely used to evaluate physiological parameters related to cardiopulmonary disorders and fitness (1). To measure oxygen uptake (V̇O2), cycle ergometry has more advantageous than a treadmill, as it can precisely measure the external work rate during exercise on a cycle ergometer (2). Additionally, for several aspects, physiological responses are different on the treadmill (e.g. the maximum V̇O2 is usually higher by about 10 to 15%) (3). Therefore, the predictive equations should discriminate by the exercise modality. Application of CPET warrants the normal values of parameters obtained from maximal exercise testing, such as (1) cardiovascular and metabolic functions (e.g. V̇O2 at peak or maximal exercise (V̇O2peak or V̇O2max), heart rate (HRpeak), and oxygen pulse (O2P); (2) ventilatory function (e.g. minute ventilation (V̇Epeak)); and (3) gas exchange efficiency function, expressed by the ventilatory equivalents for oxygen (V̇E/V̇O2) and carbon dioxide (V̇E/V̇CO2) at the lactic acidosis threshold (LAT). Reference values and predictive equations for these indices in healthy subjects have been published (4-9). Unfortunately, these predictive equations are mostly available for the Caucasians. Although there are few reference values for the Asians, but the predictive equations are constructed based on small samples (i.e. Iran (n = 34), China (n = 95) and India (n = 101)) (10-12). Moreover, different countries and ethnicities have various reference values (13). A study in Hong Kong conducted on a large population (n = 659) has evaluated the V̇O2max, but participants were all elder women (14). In Thailand, a study conducted by Promsrisuk et al. (15) on 44 healthy participants has only estimated V̇O2max during the treadmill exercise. Meanwhile, its sample size is small, particularly for those aged > 35 years of old.
2. Objectives
The study aimed to develop a new set of predictive equations of CPET parameters during maximal cycling exercise for Thai adults.
3. Methods
The current cross-sectional study is conducted at Ramathibodi Hospital for the period of 2015 to 2017. It is approved by the local Ethics Review Board (ID: 02-60-09). Written informed consent is obtained from all participants.
3.1. Participants
All 580 participants were recruited by local advertisement in the metropolitan area and were asked to complete a health screening questionnaire. First, physicians performed the physical examination for all participants. Then, spirometry was performed. Exclusion criteria were as follow: abnormal spirometry, having symptoms of diseases associated with cardiovascular and pulmonary disorders and being current smokers or ex-smokers with a history of smoking ≥ 10 pack-years. Participants who were well-treated and had asymptomatic co-existing diseases such as hypertension, diabetes mellitus, and dyslipidaemia, were allowed to participate, except for those who were on beta-blockers and calcium-channel blockers.
3.2. Procedures
All participants filled the Global Physical Activity questionnaire (GPAQ) (16). After electrocardiography (ECG), CPET was conducted by a well-trained staff using the incremental exercise protocol on a calibrated, electromagnetically braked cycle ergometer (VIAsprint 150 P, Viasys Healthcare, CA, USA). Meanwhile, gas exchange and ventilatory variables were measured breath-by-breath using a computer-based exercise system (Vmax Encore 229d, Viasys Healthcare, CA, USA).
The exercise protocol consisted of 2 minutes of rest, 2 minutes of unloaded cycling, exercise with a linear work rate increment of 10 to 25 watts/min until reaching maximum tolerance of the participant, followed by 3 minutes of recovery. In the absence of chest pain and ECG abnormalities, if despite of verbal encouragements, the participant was not able to continue the cadence, the exercise test was terminated, or if the participants reported severe fatigue or dyspnoea and reaching ≥ 8 points of the modified Borg’s numerical rating scales (17). Participants with abnormal blood pressure responses, or myocardial ischemia symptoms or those who stopped the test due to any other reasons other than intolerable fatigue were excluded. The CPET data were averaged for every 30 seconds interval, and the highest V̇O2 at the nearest 30 s -before exhaustion was chosen as V̇O2peak. The following parameters were recorded: V̇O2peak, HRpeak, peak O2P, V̇Epeak, and ventilatory equivalents for oxygen (V̇E/V̇O2), and carbon dioxide (V̇E/V̇CO2) at the LAT. To identify the LAT, non-invasive method described by Beaver et al. (18), was employed, which clearly identifies the breakpoint from the V̇CO2-V̇O2 association (V-slope method) or by the ventilatory equivalents method (19, 20).
To determine the V̇O2peak, all CPET data were reviewed by an investigator (PP) and if had the following criteria were included in the study: (1) intolerable fatigue; (2) achieving HRpeak of ≥ 85% of the predicted value, determined based on the participants’ age (220-age); and (3) respiratory exchange ratio (RER) of ≥ 1.1 (1).
The GPAQ questionnaire developed by the World Health Organization for surveillance of physical activities was employed to calculate the physical activity level in three levels (i.e. low, moderate, and high) (16). Permission to use the GPAQ was obtained from the developer.
3.3. Statistical Analysis
Data are presented by using mean and standard deviation (SD). The CPET data are separated by age and gender and are grouped into 10-year strata. To evaluate differences in CPET parameters between age groups, analysis of variance was used. Linear regression, including squared terms (to minimize the residual sum of squares) with 95% confidence interval (CI) was used to assess the associations between CPET parameters and demographic data (i.e. age, weight, height, and physical activity level). Multivariable linear regression was used to generate prediction models. For all CPET parameters, the coefficient of determination (R2) is reported with the standard error of the estimate (SEE). Data are analysed by STATA V14.0. A P value < 0.05 was considered statistically significant.
4. Results
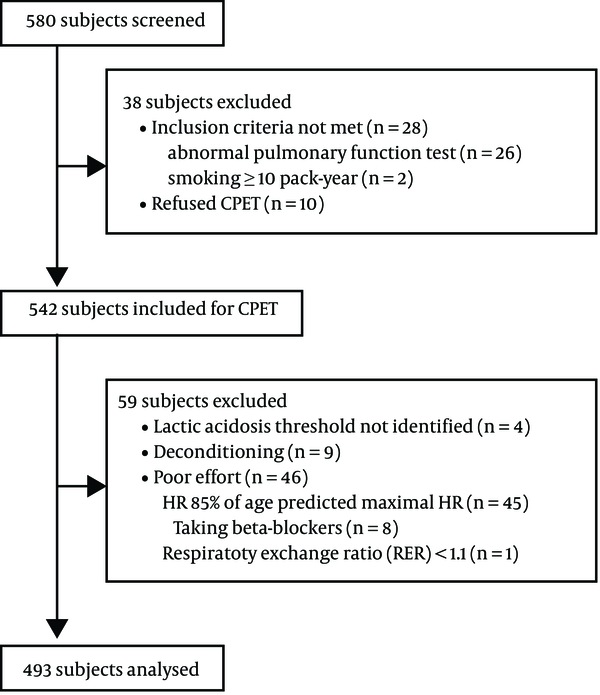
Of 580 participants, based on the exclusion criteria, 38 were excluded before CPET (Figure 1). As well, 59 were subsequently excluded from the analysis, because their CPET results revealed early termination of exercise due to any other reasons than intolerable fatigue. Finally, 493 participants were included in the analysis (208 men and 285 women). The characteristics of participants are shown in Table 1. Two participants had asthma diagnoses, but both were well-controlled without the administration of asthma medications and had normal spirometry results. Although diagnoses of hypertension (n = 44) and diabetes mellitus (n = 18) were reported, but they had acceptable blood pressure and plasma glucose control with medications. The spirometric data stratified by decade of age are illustrated in Appendix 1 in Supplementary File.
Flowchart of the recruitment scheme
4.1. Peak Oxygen Uptake and Lactic Acidosis Threshold
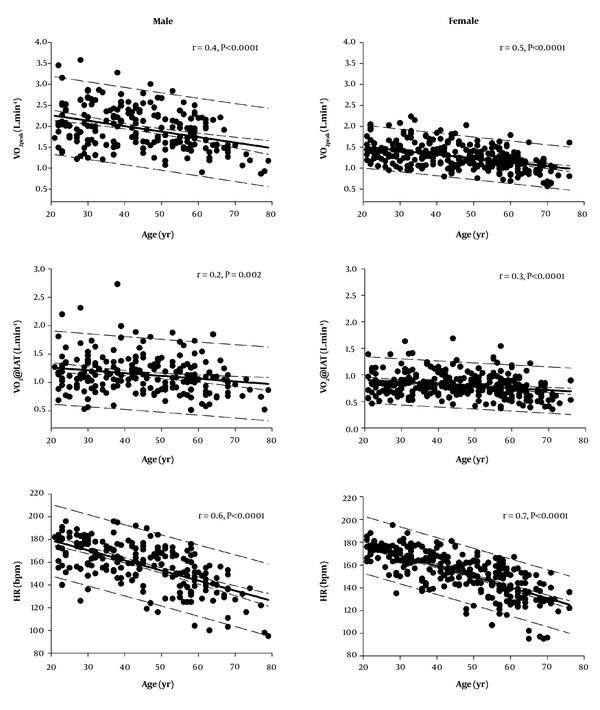
The older the participant, the lower were both V̇O2peak and V̇O2 at the LAT for both sexes (Figure 2, upper and middle panel). The average decline of V̇O2peak and LAT in men were 0.131 L.min-1 and 0.049 L.min-1 per decade of age, respectively. For women, the decline was 0.094 L.min-1 and 0.038 L.min-1 per decade of age, respectively. The rate of decline of V̇O2peak in women was not different from men (P = 0.105). The V̇O2peak of each age group is shown in Table 2. The ratio of LAT/V̇O2peak (expressed as percentages) was positively associated with age (average increase in male: 1.75% per decade of age; and for female: 1.60% per decade of age), suggesting that in comparison to LAT, the V̇O2peak declines faster as the age increases. In the current study, the LAT was achieved at approximately 60% (SD, 11.58%; range, 34% - 94%) and 64% (SD, 11.8%; range, 32% - 95%) of V̇O2peak in men and women, respectively.
Scatter plots showing the correlations between V̇O2peak (upper panel), V̇O2 at the LAT (middle panel), heart rate at peak exercise (lower panel) and age group per decade in both sexes. Solid lines represent regression lines. Medium dashed lines represent 95% confidence intervals. Long dashed lines represent 95% prediction intervals.
| Parameters | Age, y | ||||||
|---|---|---|---|---|---|---|---|
| Sex | 20 - 30 (N = 48) | 31 - 40 (N = 38) | 41 - 50 (N = 42) | 51 - 60 (N = 47) | 61 - 70 (N = 27) | 71 - 80 (N = 6) | P Value |
| Male | |||||||
| V̇O2peak, L.min -1 | 2.090 ± 0.56; [1.22 - 3.58] | 2.098 ± 0.50; [1.22 - 3.28] | 2.088 ± 0.45; [1.24 - 3.01] | 1.819 ± 0.38; [1.07 - 2.84] | 1.620c, d ± 0.35; [0.90 - 2.21] | 1.090c, d,e,f ± 0.17; [0.86 - 1.33] | < 0.001 |
| Peak WR, Watts | 166.4 ± 32.92; [91 - 251] | 165.3 ± 33.73; [77 - 258] | 153.8 ± 26.92; [99 - 217] | 133.4c, d, e ± 24.44; [85 - 207] | 110.1c, d, e, f ± 19.50; [75 - 159] | 70.7c, d, e, f, ± 24.15; [35 - 104] | < 0.001 |
| LAT, L.min -1 | 1.177 ± 0.36; [0.5 - 2.3] | 1.224 ± 0.38; [0.6 - 2.7] | 1.196 ± 0.29; [0.8 - 1.9] | 1.116 ± 0.28; [0.6 - 1.9] | 0.999 ± 0.30; [0.6 - 1.8] | 0.803 ± 0.18; [0.5 - 1.1] | 0.007 |
| HRpeak, bpm | 171.5 ± 15.52; [136 - 196] | 166.0 ± 12.66; [141 - 196] | 160.5c ± 17.66; [125 - 192] | 149.2c, d, e ± 16.45; [122 - 176] | 138.1c, d, e ± 15.54; [110 - 157] | 116.7c, d, e, f, g ± 17.29; [100 - 137] | < 0.001 |
| Peak O2P, mL/beat | 12.3 ± 3.46; [7.5 - 21.5] | 12.7 ± 3.28; [8.0 - 20.5] | 13.1 ± 2.66; [7.5 - 18.3] | 12.3 ± 2.64; [7.1 - 18.4] | 11.8 ± 2.25; [7.0 - 15.4] | 9.5 ± 2.04; [7.1 - 12.4] | 0.085 |
| V̇Epeak, L.min -1 | 80.6 ± 19.59; [40 - 124] | 75.4 ± 15.76; [46 - 101] | 74.8 ± 17.08; [43 - 110] | 65.8c ± 15.22; [40 - 110] | 60.0c, d, e ± 13.91; [36 - 99] | 38.9c, d, e, f ± 7.30; [30 - 48] | < 0.001 |
| V̇E/V̇O2 at LAT | 25.5 ± 2.53; [21 - 32] | 25.7 ± 3.51; [20 - 35] | 26.3 ± 2.92; [22 - 38] | 27.2 ± 3.86; [23 - 38] | 29.2c, d, e ± 3.39; [24 - 38] | 31.8c, d, e, f ± 3.76; [28 - 37] | < 0.001 |
| V̇E/V̇CO2 at LAT | 25.0 ± 2.62; [21 - 33] | 25.9 ± 3.99; [20 - 38] | 26.9 ± 3.17; [22 - 37] | 27.6c ± 3.84; [21 - 39] | 30.2c, d, e, f ± 3.23; [26 - 39] | 33.0c, d, e, f ± 4.00; [28 - 38] | < 0.001 |
| V̇Epeak/MVV | 0.54 ± 0.14 | 0.55 ± 0.12 | 0.59 ± 0.15 | 0.58 ± 0.14 | 0.60 ± 0.14 | 0.52 ± 0.18 | 0.275 |
| Female | |||||||
| V̇O2peak, L.min -1 | 1.403 ± 0.28; [1.01 - 2.08] | 1.413 ± 0.30; [1.00 - 2.23] | 1.302 ± 0.28; [0.81 - 2.02] | 1.202c, d ± 0.23; [0.75 - 1.79] | 1.051c, d, e, f ± 0.20; [0.65 - 1.62] | 0.940c, d, e, f ± 0.31; [0.63 - 1.61] | < 0.001 |
| Peak WR, Watts | 107.1 ± 19.06; [75 - 156] | 100.8 ± 24.21; [70 - 154] | 90.0c, d ± 16.81 [60 - 134] | 82.7c, d, e ± 16.20; [48 - 121] | 69.4c, d, e, f ± 14.23; [45 - 112] | 65.8c, d, e ± 23.82; [45 - 113] | < 0.001 |
| LAT, L.min -1 | 0.819 ± 0.22; [0.5 - 1.4] | 0.871 ± 0.25; [0.5 - 1.6] | 0.852 ± 0.21; [0.4 - 1.7] | 0.797 ± 0.22; [0.4 - 1.5] | 0.692 d, e ± 0.19; [0.4 - 1.2] | 0.577 d, e ± 0.16; [0.4 - 0.9] | < 0.001 |
| HRpeak, bpm | 170.8 ± 10.34; [135 - 195] | 161.3c ± 12.47; [134 - 188] | 155.6c ± 12.98; [117 - 181] | 144.3c, d ± 15.68; [107 - 171] | 131.7c, d, e, f ± 18.01; [102 - 167] | 132.0c, d, e ± 10.92; [119 - 153] | < 0.001 |
| Peak O2P, mL/beat | 8.2 ± 1.64; [6.0 - 12.7] | 8.9 ± 2.64; [6.0 - 23.8] | 8.4 ± 1.64; [6.0 - 13.2] | 8.4 ± 1.53; [5.0 - 11.7] | 8.0 ± 1.50; [5.3 - 13.1] | 7.1 ± 2.21; [5.0 - 11.8] | 0.065 |
| V̇Epeak, L.min -1 | 56.3 ± 11.33; [35 - 82] | 50.7 ± 9.70; [35 - 71] | 47.9c ± 13.59; [27 - 87] | 42.3c, d ± 9.71; [24 - 67] | 39.1c, d, e ± 7.55; [24 - 56] | 35.35c, d, e ± 10.59; [24 - 58] | < 0.001 |
| V̇E/V̇O2 at LAT | 28.2 ± 3.58; [22 - 43] | 27.1 ± 2.49; [21 - 32] | 28.1 ± 4.22; [22 - 36] | 27.8 ± 2.52; [23 - 34] | 30.3 d, e, f ± 3.74; [26 - 37] | 31.4 d, e, f ± 2.77; [29 - 36] | < 0.001 |
| V̇E/V̇CO2 at LAT | 28.0 ± 3.49; [22 - 30] | 28.4 ± 2.34; [23 - 33] | 28.8 ± 3.94; [23 - 35] | 28.7 ± 2.73; [23 - 35] | 31.0c, d, e, f ± 3.02; [27 - 39] | 33.3c, d, e, f ± 2.55; [29 - 36] | < 0.001 |
| V̇Epeak/MVV | 0.52 ± 0.10 | 0.54 ± 0.11 | 0.56 ± 0.15 | 0.54 ± 0.13 | 0.57 ± 0.12 | 0.56 ± 0.14 | 0.448 |
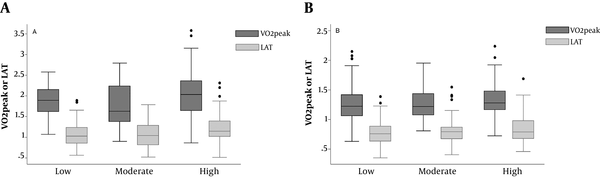
Analysis of V̇O2peak and V̇O2 at the LAT stratified by physical activity level is shown in Figure 3A and B, respectively. Participants who reported low physical activity had lower V̇O2peak and V̇O2 at the LAT than those who reported high physical activity. (value difference for men: 0.178 ± 0.08, P = 0.037, and 0.150 ± 0.05 L.min-1, P = 0.007, respectively, value difference for female: 0.075 ± 0.04, P = 0.093, and 0.074 ± 0.03 L.min-1, P = 0.031, respectively). The values of V̇O2peak and V̇O2 at the LAT in participants who reported moderate physical activity were not different than those who reported low physical activity.
A, V̇O2peak and V̇O2 at the LAT across the physical activity levels for males; B, V̇O2peak and V̇O2 at the LAT across the physical activity levels for females.
4.2. Peak Heart Rate
As Figure 2 shows, HRpeak is negatively associated with age (average group decline in male: 8.9 bpm per decade of age, female: 9.4 bpm per decade of age). There was no difference between men and women in any age group. The HRpeak in each age group is shown in Table 2.
4.3. Peak Oxygen Pulse
For both sexes, the values of peak O2P slightly declined with advancing age; average decline for male was: 0.18 mL/beat per decade of age, and for female was: 0.10 mL/beat per decade of age.
4.4. Peak Minute Ventilation
The values of V̇Epeak were negatively associated with age, so that the higher the age, the lower was VEpeak (average decline in male: 5.7 L.min-1 per decade of age, and for female: 4.3 L.min-1 per decade of age), as shown in Figure 4 (upper panel). The highest value of V̇Epeak for men (80.6 ± 19.6 L.min-1) and women (56.3 ± 11.3 L.min-1) were observed in the youngest age groups (difference between both sexes, P < 0.001).
Scatter plots showing the correlations between V̇Epeak (upper panel), V̇E/V̇CO2 at the LAT (lower panel) and age group per decade in both sexes. Solid lines represent regression lines. Medium dashed lines represent 95% confidence intervals. Long dashed lines represent 95% prediction intervals.
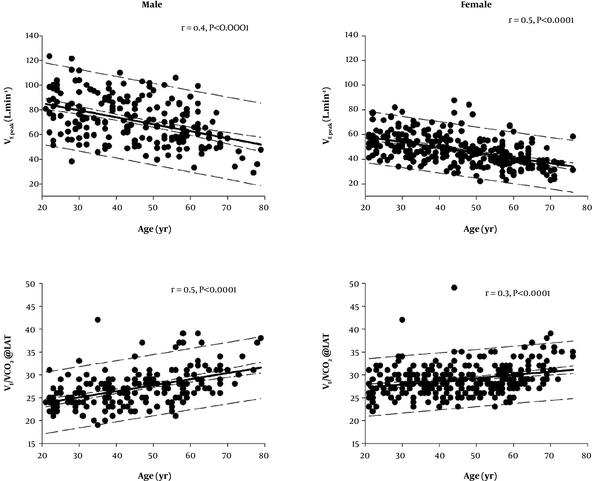
4.5. Ventilatory Equivalents for Oxygen and Carbon Dioxide
For both sexes, values of V̇E/V̇O2 and V̇E/V̇CO2 (Figure 4, lower panel) were increasing with age. (average increase in male: 1.0 per decade of age, for female: 0.5 per decade of age; and for male: 1.3 per decade of age, and for female: 0.7 per decade of age, respectively), with a steeper slope in men (P = 0.021 and P = 0.003, respectively).
4.6. Predictive Equations for key CPET Parameters
The predictive equations for CPET parameters are listed in Table 3. The correlations of CPET parameters with age, weight, height, and physical activity level are summarized in Appendix 2 in Supplementary File.
| Parameters | Sex | Equations | R2 | SEE |
|---|---|---|---|---|
| V̇O2peak, L.min-1 | M | -2.268 + (0.037 × A) - (0.0005 × A2) + (0.016 × W) + (0.014 × H) + (0.104 × Act) | 0.41 | 0.392 |
| F | -0.34 + (0.009 × A) - (0.0002 × A2) + (0.012 × W) + (0.005 × H) + (0.058 × Act) | 0.44 | 0.220 | |
| Peak WR, Watts | M | -56.87 + (2.64 × A) - (0.04 × A2) + (0.80 × W) + (0.64 × H) + (7.68 × Act) | 0.56 | 24.4 |
| F | -49.10 - (0.79 × A) + (0.48 × W) + (0.90 × H) + (3.36 × Act) | 0.46 | 17.0 | |
| LAT, L.min-1 | M | -1.082 + (0.017 × A) - (0.0002 × A2) + (0.012 × W) + (0.006 × H) + (0.083 × Act) | 0.32 | 0.270 |
| F | -1.030 + (0.163 × A) - (0.0002 × A2) + (0.008 × W) + (0.007 × H) + (0.052 × Act) | 0.29 | 0.190 | |
| HRpeak, bpm | M | 197.17 - (0.90 × A) | 0.40 | 15.82 |
| F | 195.86 - (0.94 × A) | 0.46 | 14.79 | |
| Peak O2P, mL/beat | M | -18.43 + (0.18 × A) - (0.002 × A2) + (0.10 × W) + (0.11 × H) + (0.67 × Act) | 0.32 | 2.50 |
| F | -3.86 + (0.11 × A) - (0.001 × A2) + (0.09 × W) + (0.13 × H) + (0.42 × Act) | 0.28 | 1.66 | |
| V̇Epeak, L.min-1 | M | 7.86 - (0.47 × A) + (0.52 × W) + (0.28 × H) | 0.32 | 15.41 |
| F | 16.69 - (0.41 × A) + (0.32 × W) + (0.20 × H) | 0.35 | 9.89 | |
| V̇E/V̇O2 at LAT | M | 27.24 - (0.15 × A) + (0.003 × A2) | 0.19 | 3.21 |
| F | 31.82 - (0.23 × A) + (0.003 × A2) | 0.08 | 3.33 | |
| V̇E/V̇CO2 at LAT | M | 25.38 - (0.07 × A) + (0.002 × A2) | 0.26 | 3.35 |
| F | 30.17 - (0.14 × A) + (0.002 × A2) | 0.11 | 3.13 |
5. Discussion
This is the first study that established predictive equations for the key CPET parameters during cycle ergometry in Thai adults. A large study about CPET measurements is conducted on 4,631 healthy Norwegian using a treadmill protocol (9). The authors reported that coefficients of determination for V̇O2max and LAT are the best, a finding similar to the results of the current study in terms of V̇O2peak, and HRpeak. The values of V̇O2peak and LAT in a sample of the Caucasian were higher than those reported in the current study, mainly due to differences in anthropometric measures and physical fitness. The average (SD) of V̇O2peak for Thai male (age range, 20 - 50 years) was 2.056 (0.53) L.min-1, comparable to those of Chinese male [1.993 (0.45) L.min-1] (11), and higher than those of Indian male [1.795 (0.39) L.min-1] (12). Also, the V̇O2peak for Thai female (age range, 20 - 50 years) is 1.373 (0.29) L.min-1, similar to Chinese female [1.339 (0.22) L.min-1] (11), and was higher than those of the Indian female [1.292 (0.24) L.min-1] (12). Therefore, ethnic diversity plays a significant role in the differences between CPET parameters of various populations.
In Thailand, a study conducted by Promsirisuk et al. (15) on 44 healthy Thais established a predictive equation for V̇O2max on a treadmill. The values obtained by the current study for predictive equations are lower than those in the previously conducted study by about 17% in both sexes. Because as a result of lesser muscle utilization and increased perception of leg fatigue while exercising on a cycle ergometer, the value of V̇O2 derived from cycle ergometry is generally lower than that of the treadmill (2).
The findings also show that the highest value of V̇O2peak was observed in the group of 31 to 40 years old. The V̇O2peak values begun to decline significantly for 51 - 60 years old age group for both sexes, while LAT in men declined slightly slower than women in the 61 to 70 years old age group. The observed decline in V̇O2peak of older Asian is mostly related to their lower lean muscle mass (21), and the decline in V̇O2 at the LAT can be attributed to lower muscle aerobic capacity, lower physical activity, or significant reduction in cardiac output.
The highest value of V̇Epeak was observed in the youngest age group and its decline began sooner in women than men, indicating the more limited ventilatory capacity in women. For males aged 20 to 50 years of old, the average (SD) of V̇Epeak was 77 (17.5) L.min-1. These values are aligned with age-group matched V̇Epeak from other Asian populations. The values of V̇Epeak for Chinese and Indian male were 80 (24.3) L.min-1, and 61 (15.7) L.min-1, respectively (11, 12). Interestingly, the ratio of V̇Epeak to maximal voluntary ventilation (MVV) was not changing by changing age group, implying that individuals ceased the exercise at the same ventilatory demand.
For both sexes, the values of V̇E/V̇O2 and V̇E/V̇CO2 at LAT were lower in younger than those with higher ages, the effect begun at age of > 60 years. Brischetto et al. (22) reported that the V̇E/V̇CO2 during exercise was greater in older than younger participants and argued that the increased ventilation to maintain an isocapnic state during exercise seems to compensate for the declined efficiency of gas exchange in aging lungs.
Compared with other studies on Caucasians (4-9), in the current study, the V̇O2peak values were lower by about 40% for both sexes. This could be due to a major difference between the two populations in terms of body stature, habitual physical activity, nutrition, and socioeconomic factors. Therefore, many participants would have been misclassified as having functional impairment, if the predictive equations for the Caucasians were applied.
It worth noting that, it seems using the prevailing formula of age-predicted maximal HR (220-age) in Thai population results in significant overestimation of maximal HR. Applying a new predictive equation of HRpeak may have important implications in exercise prescription and prediction of V̇O2 during submaximal exercise.
We acknowledge that the current study has limitations. First, due to a small proportion of elder participants, extrapolation of the predictive values to older adults may be controversial. Second, 8% and 3.5% of elder participants had hypertension and diabetes mellitus, respectively. However, they had good disease control, and didn’t have cardiovascular complications when they entered the study, which minimized the influence of these comorbidities on the results. Finally, the data are mainly derived from participants with a relatively sedentary lifestyle. Future research should be with greater number of participants and contain various fitness statuses from all age ranges.
In conclusion, this is the first study providing predictive equations for incremental cycling exercise in Thai adults. These will be useful tools for evaluating cardiopulmonary heath of the Thai and perhaps for other populations with geographical or ethnical proximity.
References
-
1.
American Thoracic Society; American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211-77. [PubMed ID: 12524257]. https://doi.org/10.1164/rccm.167.2.211.
-
2.
Hansen JE. Exercise instruments, schemes, and protocols for evaluating the dyspneic patient. Am Rev Respir Dis. 1984;129(2 Pt 2):S25-7. [PubMed ID: 6696337]. https://doi.org/10.1164/arrd.1984.129.2P2.S25.
-
3.
Porszasz J, Stringer W, Casaburi R. Equipment, measurements and quality control. In: Palange P, Laveneziana P, Neder JA, editors. Clinical Exercise Testing. Sheffield: European Respiratory Society; 2018. p. 59-81. https://doi.org/10.1183/2312508x.10011117.
-
4.
Sue DY, Hansen JE. Normal values in adults during exercise testing. Clin Chest Med. 1984;5(1):89-98. [PubMed ID: 6723246].
-
5.
Jones NL, Makrides L, Hitchcock C, Chypchar T, McCartney N. Normal standards for an incremental progressive cycle ergometer test. Am Rev Respir Dis. 1985;131(5):700-8. [PubMed ID: 3923878]. https://doi.org/10.1164/arrd.1985.131.5.700.
-
6.
Hansen JE, Sue DY, Wasserman K. Predicted values for clinical exercise testing. Am Rev Respir Dis. 1984;129(2 Pt 2):S49-55. [PubMed ID: 6421218]. https://doi.org/10.1164/arrd.1984.129.2P2.S49.
-
7.
Neder JA, Nery LE, Castelo A, Andreoni S, Lerario MC, Sachs A, et al. Prediction of metabolic and cardiopulmonary responses to maximum cycle ergometry: A randomised study. Eur Respir J. 1999;14(6):1304-13. [PubMed ID: 10624759]. https://doi.org/10.1183/09031936.99.14613049.
-
8.
Koch B, Schaper C, Ittermann T, Spielhagen T, Dorr M, Volzke H, et al. Reference values for cardiopulmonary exercise testing in healthy volunteers: The SHIP study. Eur Respir J. 2009;33(2):389-97. [PubMed ID: 18768575]. https://doi.org/10.1183/09031936.00074208.
-
9.
Loe H, Steinshamn S, Wisloff U. Cardio-respiratory reference data in 4631 healthy men and women 20-90 years: The HUNT 3 fitness study. PLoS One. 2014;9(11). e113884. [PubMed ID: 25426954]. [PubMed Central ID: PMC4245230]. https://doi.org/10.1371/journal.pone.0113884.
-
10.
Mohammad MM, Dadashpour S, Adimi P. Predicted values of cardiopulmonary exercise testing in healthy individuals (a pilot study). Tanaffos. 2012;11(1):18-25. [PubMed ID: 25191396]. [PubMed Central ID: PMC4153176].
-
11.
Ong KC, Loo CM, Ong YY, Chan SP, Earnest A, Saw SM. Predictive values for cardiopulmonary exercise testing in sedentary Chinese adults. Respirology. 2002;7(3):225-31. [PubMed ID: 12153688]. https://doi.org/10.1046/j.1440-1843.2002.00393.x.
-
12.
John N, Thangakunam B, Devasahayam AJ, Peravali V, Christopher DJ. Maximal oxygen uptake is lower for a healthy Indian population compared to white populations. J Cardiopulm Rehabil Prev. 2011;31(5):322-7. [PubMed ID: 21734591]. https://doi.org/10.1097/HCR.0b013e318220a7b0.
-
13.
Paap D, Takken T. Reference values for cardiopulmonary exercise testing in healthy adults: A systematic review. Expert Rev Cardiovasc Ther. 2014;12(12):1439-53. [PubMed ID: 25418758]. https://doi.org/10.1586/14779072.2014.985657.
-
14.
Yu R, Yau F, Ho S, Woo J. Cardiorespiratory fitness and its association with body composition and physical activity in Hong Kong Chinese women aged from 55 to 94 years. Maturitas. 2011;69(4):348-53. [PubMed ID: 21683535]. https://doi.org/10.1016/j.maturitas.2011.05.003.
-
15.
Promsrisuk T, Khrisanapant W, Pasurivong O, Boonsawat W, Pussadhamma B, Benjapornlert P, et al. Prediction equations for maximum aerobic capacity using cardiopulmonary exercise testing among Thais. Asia-Pac J Sci Technol. 2015;20(4):449-58.
-
16.
Cleland CL, Hunter RF, Kee F, Cupples ME, Sallis JF, Tully MA. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health. 2014;14:1255. [PubMed ID: 25492375]. [PubMed Central ID: PMC4295403]. https://doi.org/10.1186/1471-2458-14-1255.
-
17.
Crisafulli E, Clini EM. Measures of dyspnea in pulmonary rehabilitation. Multidiscip Respir Med. 2010;5(3):202-10. [PubMed ID: 22958431]. [PubMed Central ID: PMC3463047]. https://doi.org/10.1186/2049-6958-5-3-202.
-
18.
Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol (1985). 1986;60(6):2020-7. [PubMed ID: 3087938]. https://doi.org/10.1152/jappl.1986.60.6.2020.
-
19.
Wasserman K, Beaver WL, Whipp BJ. Gas exchange theory and the lactic acidosis (anaerobic) threshold. Circulation. 1990;81(1 Suppl):II14-30. [PubMed ID: 2403868].
-
20.
Sun XG, Hansen JE, Garatachea N, Storer TW, Wasserman K. Ventilatory efficiency during exercise in healthy subjects. Am J Respir Crit Care Med. 2002;166(11):1443-8. [PubMed ID: 12450934]. https://doi.org/10.1164/rccm.2202033.
-
21.
Wong SY, Chan FW, Lee CK, Li M, Yeung F, Lum CC, et al. Maximum oxygen uptake and body composition of healthy Hong Kong Chinese adult men and women aged 20 - 64 years. J Sports Sci. 2008;26(3):295-302. [PubMed ID: 17943590]. https://doi.org/10.1080/02640410701552658.
-
22.
Brischetto MJ, Millman RP, Peterson DD, Silage DA, Pack AI. Effect of aging on ventilatory response to exercise and CO2. J Appl Physiol Respir Environ Exerc Physiol. 1984;56(5):1143-50. [PubMed ID: 6427148]. https://doi.org/10.1152/jappl.1984.56.5.1143.