1. Background
Low back pain (LBP) is a common complication in athletes. It has been reported that the point prevalence of LBP among competitive athletes displays a wide range (10% - 65%) (1, 2). Evidence also suggests that the prevalence of LBP in young elite athletes is about three to five times higher than age-matched non-athletes (3). In a recent study, the prevalence of LBP in male soccer players who were competing in the UEFA champions league was evaluated, and the results showed that the overall prevalence of LBP over 12 months was about 64% (3). In another study, the one-year prevalence rate of LBP in female soccer players was estimated to be approximately 57%. Apart from LBP prevalence, only a few studies have evaluated the incidence rate of LBP among soccer athletes. Overall, it appears that LBP is of great concern to athletes in relation to their career as it frequently leads to absences from competitions and missed training sessions (2).
Different general and sport-specific risk factors for LBP have been proposed in the literature. A recent review has shown that the previous history of LBP, reduced lumbar extension and flexion range of motion, tightness of hip flexor muscles, and higher body weight are positively associated with LBP in athletes (4). Moreover, deeper insight into the mechanism of LBP demonstrates the role of trunk muscles, including transversus abdominis (TrA), Internal Oblique (IO), external oblique (EO), and lumbar multifidus (LM) muscles in athletes’ LBP. Abdelraouf et al. (5) showed that poor core endurance is related to nonspecific LBP in male athletes. Also, previous studies have shown that LBP has altered the performance, thickness, or CSA of trunk muscles in elite Australian football players (6), off-road cyclists (7), cricketers (8), young male soccer players (9), and recreational runners (10). However, studies in ballet dancers, adolescent soccer players, and rowers did not show similar findings. Other studies have also reported that retraining trunk muscles reduced LBP in elite cricket and football players (11, 12).
Soccer is one of the most popular sports around the world. As noted previously, considering its prevalence and incidence, soccer players are at risk of LBP. However, little is known about the role of the trunk muscle thickness and CSA as a cause or effect of LBP. In recent studies, the relationship between a history of LBP in soccer players and trunk muscles has been investigated, but the design of the studies conducted to date are mainly retrospective (ex. cross-sectional or case-control), and thus prone to multiple biases (11). Recall bias is one of the main limitations in retrospective studies based on the memory of the athlete, which makes it difficult for the athlete to remember whether the symptom was matched with the term defined in the study. Furthermore, the natural course of the disease is not specified in retrospective studies, which is still a dilemma for LBP in soccer players. Therefore, the question remains whether LBP is a cause of trunk muscle weakness due to the athletes being less physically active, or whether the trunk muscle weakness could be an etiology of LBP. As cohort studies are mainly designed to reveal the etiologies of diseases and the possible risk factors, the purpose of this study is to prospectively measure the association between abdominal muscle thickness, lumbar multifidus cross-sectional area, hamstring flexibility, leg length discrepancy, lumbar spine flexibility, as well as trunk extensor muscle endurance and the development of LBP in a cohort of elite male adult soccer players. To the best of our knowledge, only one study before has assessed the relation between low back pain and some factors in the adolescent soccer players (13).
2. Objectives
This study, for the first time, investigates the risk factors in the adult soccer players.
3. Methods
3.1. Participants
For the current study, 42 elite male soccer players with the age range between 16 and 24 years were recruited from professional soccer teams. The participants met the inclusion criteria including playing in the premier league, having more than five hours of soccer training per week, having more than two years of experience in competitive sports and no history of LBP over the past 6 months; spinal or abdominal surgery, systemic disease or spinal deformity which could affect the diameter of lateral abdominal muscles and CSA of LM. The exclusion criteria were severe musculoskeletal trauma leading to leaving practice or participation in matches and experiencing LBP due to direct trauma to the spine. After explaining the protocol to the participants, a written consent form was obtained from the athletes and their parents (if they were younger than 18). Furthermore, the study protocol was approved by the Ethical Committee of the University (code: IR.TUMS.REC.1394.1120).
3.2. Measures
Background data including age, training hours per week, history of previous LBP, and age of starting to compete were obtained from the participants via a questionnaire. To measure the height of the participants, they were asked to stand up straight without shoes against a scaled wall. The distance between the terminal part of their heels and the top of their head was measured in centimeters. The participants were weighed on a calibrated scale by 0.1 kg accuracy while wearing the least clothes.
The thickness of lateral abdominal muscles including transversus abdominis (TrA), internal oblique (IO) and external oblique (EO) was measured in millimeters by the ultrasonography device (Micromaxx SonoSite, USA) and a linear transducer (6 - 13 MHZ) in a B-mode format in both the resting and abdominal drawing-in maneuver (ADiM). The transducer was located perpendicular to the transverse plane, and by using the device’s caliper, the measurement was performed at the midpoint of the image. The shot-view for the measurement was taken, by an expert assessor with more than three years of experience, after a normal expiration so that the muscles would be in their maximum thickness. The measurement was performed in a supine (hook-lying position) (14) with a distance of 25 millimeters anteromedial from the median point of the midaxillary line between the lowest rib and iliac crest (15). The space between the top of the inferior fascial layer and the bottom of the superior fascial layer was measured as muscle thickness. For avoiding the effect of food consumption on the aforementioned muscle thickness, the ultrasound measurements were performed with sufficient time after the last consumed meal (16, 17). Before thickness measurement during ADiM, we trained the participants to perform a proper ADiM two times with ultrasound feedback. Also, in the prone position, the CSA of the LM muscles at the L4 level was assessed bilaterally. Moreover, for LM measurement in contraction, the participants were asked to contract their paraspinal muscles (under the ultrasound probe) after a relaxed breath two times before the beginning of the assessment (18).
We evaluated the isometric endurance of trunk extensor muscles by the Sorensen test. In this test, the participants lied face down on the examination table while the superior border of their iliac crest was aligned with the edge of the table. The assessor fastened the lower part of their body to the table in three parts (pelvis, knees, and ankles). The patients were asked to fold their arms, and we recorded the time (sec) in which the patients could keep their upper body straight and horizontal. We applied an inclinometer lightly between their two scapulae, and when their upper body was down-sloped more than 10°, the test was stopped (19).
To measure leg length discrepancy (LLD), we measured the distance between the anterior superior iliac spine (ASIS) and the medial malleolus of both lower extremities and recorded the difference between them for each participant.
Hamstring flexibility (tightness) was measured by the knee extension angle (KEA) test (20). The participants lied on the examination table in the supine position while their right knee and hip were flexed at 90°, and the left knee was flat on the table. In that position, the assessor extended their knee just to the point of tightness or pain at the knee. Also, two Baseline® bubble inclinometers were placed at the superior pole of the patella on the thigh (for maintaining hip flexion at 90°) and parallel to medial malleolus on the tibia (to measure hamstring flexibility angle). We applied the “180° minus hamstring flexibility angle” as hamstring tightness in the statistical analysis (20).
Regarding back muscle flexibility, we applied an active lumbar forward flexion test. The distance between the spinous process of T12 and S1 vertebrae in the standing and active forward bending position was measured in centimeters. For precise detection of the spinous process after palpation, we confirmed their position via a longitudinal ultrasound scan (21).
The intensity of LBP felt by the participants during the season was evaluated by a visual analysis scale (VAS) from 0 (no pain) to 100 (most intense pain they had ever felt) on a solid horizontal line.
3.3. Study’s Process
Our examiner attended training sessions of the soccer players and explained the protocol of the study to the participants. After collecting the aforementioned data at the baseline, the examiner followed the participants for a season in case of any LBP incidence. We defined LBP as “low back pain is pain between the last rib and the lower gluteal fold as you can see in the following picture (a gray area), which is bad enough to limit or change athletes’ daily routine or sports activities for more than 1 day” which was explained and illustrated to the participants (2). If any player reported LBP during the study, he would be considered in the LBP group for analysis.
3.4. Statistics
The quantitative data are presented as mean (SD). Logistic regression, adjusted by age and weight was used to assess the relationship and odds ratio (OR) between LBP and the thickness of abdominal muscles and other related factors evaluated in the present study. Considering the importance of body mass normalization for ultrasound measurements (22), and since we did not have access to allometric parameters of lateral abdominal muscles in adult players (they were only provided for adolescents (23)), we adjusted logistic regression analysis by age and body mass (weight). The significance level of this study was considered as P less than 0.05, and SPSS, version 21 was used for all data analyses in the study.
4. Results
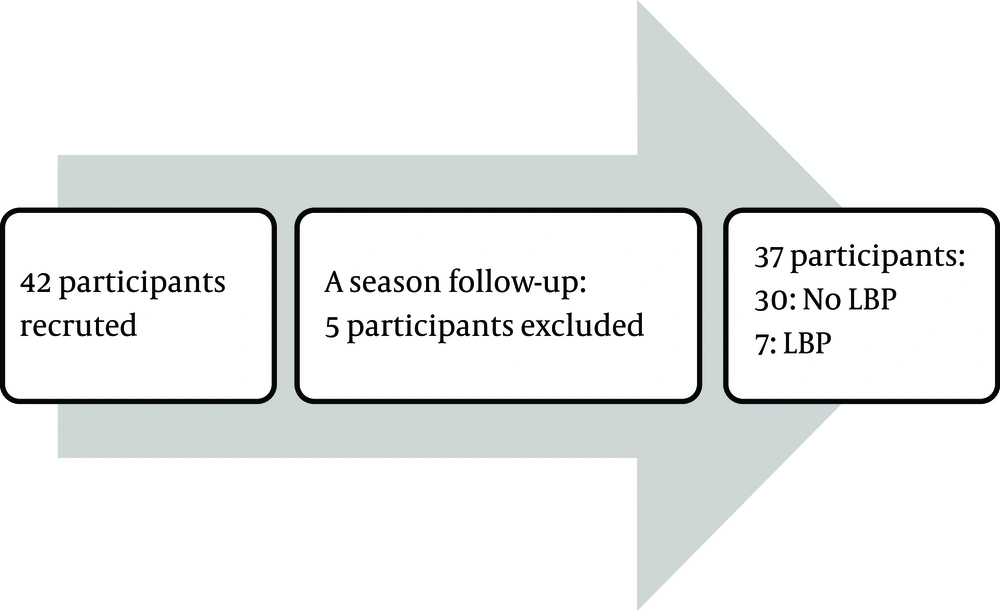
In the present study, 37 participants out of 42 completed the follow-up, and 5 participants were excluded from the study (2 due to trauma to the back and 2 had knee injuries which needed surgery and were prohibited from playing, and 1 left the team). Seven participants reported LBP during the follow-up (Figure 1).
The mean (SD) age and weight of the participants at the onset of the study were 18.5 (2.3) and 67.8 (7.5). Other background data of the participants are presented in Table 1. The results showed that 15 participants had experienced LBP in their lifetime, 13 of which had experienced LBP during their sports career (but not in the past six months). None of the participants suffered from LBP at the beginning of the study, and neither of them had felt radicular pain or paresthesia in their feet alongside LBP before.
| Variant (Range) | Values (Mean ± SD) |
|---|---|
| Age, y | |
| 16 – 23 | 18.5 ± 2.3 |
| Weight, kg | |
| 51.0 - 80.0 | 67.8 ± 7.5 |
| Height, cm | |
| 156.5 - 188.0 | 176.6 ± 7.7 |
| BMI, kg/m2 | |
| 19.4 - 23.9 | 21.7 ± 1.2 |
| Training time, h per week | |
| 5.0 - 16.0 | 8.3 ± 3.2 |
| Age of starting to compete, y | |
| 10 - 16 | 12.2 ± 1.8 |
Abbreviations: BMI, body mass index; N, number; SD, standard deviation.
aValues are expressed as mean ± SD.
No significant relation was detected between LBP’s incidence and a lifetime experience of LBP (P = 0.69) and also the history of LBP during their soccer career (P = 0.33). The mean (SD) score of VAS in the last episode of LBP reported by the participants was 3.9 (2.1), and no relation was seen between the VAS and incidence of LBP (P = 0.37).
We measured the muscle thickness of 3 trunk muscles (EO, IO, and TrA) and CSA of LM in resting and contraction position before the study. As presented in Table 2, we detected no significant relationship between LBP’s incidence and the thickness of the muscles mentioned above in the two statuses. The effect of other factors such as hamstring flexibility, back flexibility, muscle endurance, and LLD on the incidence of LBP were analyzed and presented in Table 3, in which no significant relationship was found.
| Muscles | Side of Muscle | Participants Who Did Not Report LBP During the Study (N = 30) | Participants Who Reported LBP During the Study (N = 7) | Between Groupsc | |
|---|---|---|---|---|---|
| Before Study | Before Study | OR | P Value | ||
| During rest | |||||
| EO, cm | Right | 0.7 ± 0.1 | 0.7 ± 0.1 | 1.2 | 0.97 |
| Left | 0.7 ± 0.1 | 0.7 ± 0.1 | 1.3 | 0.95 | |
| IO, cm | Right | 1.0 ± 0.2 | 1.0 ± 0.3 | 0.3 | 0.61 |
| Left | 1.0 ± 0.2 | 1.0 ± 0.1 | 2.6 | 0.75 | |
| TrA, cm | Right | 0.4 ± 0.1 | 0.4 ± 0.2 | 0.005 | 0.24 |
| Left | 0.4 ± 0.1 | 0.4 ± 0.1 | 0.003 | 0.18 | |
| LM cm2 | Right | 5.6 ± 1.8 | 5.5 ± 1.3 | 1.1 | 0.96 |
| Left | 5.4 ± 1.6 | 5.4 ± 1.3 | 0.9 | 0.82 | |
| During ADiM | |||||
| EO, cm | Right | 0.8 ± 0.1 | 0.8 ± 0.1 | 0.1 | 0.57 |
| Left | 0.8 ± 0.2 | 0.8 ± 0.1 | 0.6 | 0.88 | |
| IO, cm | Right | 1.9 ± 1.0 | 1.7 ± 0.9 | 2.1 | 0.26 |
| Left | 1.9 ± 0.9 | 1.6 ± 0.8 | 2.7 | 0.14 | |
| TrA, cm | Right | 0.5 ± 0.1 | 0.5 ± 0.1 | 0.001 | 0.14 |
| Left | 0.5 ± 0.1 | 0.5 ± 0.2 | 0.001 | 0.08 | |
| LM contraction | |||||
| LM cm2 | Right | 6.7 ± 2.0 | 6.4 ± 1.7 | 1.3 | 0.49 |
| Left | 6.8 ± 2.1 | 6.5 ± 1.5 | 1.2 | 0.56 | |
Abbreviations: EO, external oblique; IO, internal oblique; LM, lumber multifidus; SD, Standard deviation; TrA, transversus abdominis.
aValues are expressed as mean ± SD.
bStatistically significant (P value < 0.05).
cBinary logistic regression adjusted by age and weight.
| Variable | Participants Who Did Not Report LBP During the Study (N = 30) | Participants Who Reported LBP During the Study (N = 7) | Between Groupsc | |
|---|---|---|---|---|
| Before Study | Before Study | OR | P Value | |
| Weight, kg | 67.1 ± 7.9 | 70.7 ± 5.3 | 0.91 | 0.22 |
| Height, cm | 175.9 ± 8.3 | 179.1 ± 3.7 | 0.94 | 0.32 |
| BMI, kg/m2 | 21.6 ± 1.1 | 22.0 ± 1.2 | 0.68 | 0.35 |
| Sorensen test, sec | 176.8 ± 40.3 | 183.4 ± 29.6 | 0.99 | 0.57 |
| LLD, cm | 0.4 ± 0.4 | 0.3 ± 0.4 | 2.05 | 0.54 |
| HT, ° | ||||
| Right side | 22.7 ± 10.1 | 21.4 ± 7.3 | 1.02 | 0.65 |
| Left side | 20.1 ± 11.6 | 23.4 ± 5.9 | 0.97 | 0.48 |
| LFFT, cm | 4.7 ± 1.2 | 5.3 ± 1.4 | 0.65 | 0.25 |
| Training time, hour/week | 8.2 ± 3.3 | 8.8 ± 2.7 | 0.96 | 0.78 |
| Age of starting to compete, y | 12.4 ± 1.9 | 11.4 ± 1.5 | 1.40 | 0.25 |
Abbreviations: HT, hamstring tightness; LFFT, lumbar forward flexion test for evaluating back muscles flexibility; LLD, leg length discrepancy; SD, standard deviation; Sorensen test, evaluating the isometric endurance of trunk extensor muscles.
aValues are expressed as mean ± SD.
bStatistically significant (P value < 0.05).
cBinary logistic regression adjusted by age and weight.
5. Discussion
Trunk muscles’ size and function have received much attention in the literature considering their role as a risk factor for LBP in the general population and also in athletes (6-8, 24). Whether truck muscles’ size could be a cause for LBP in athletes, such as soccer players, was our question and led us to design the present study. This study’s findings revealed that LBP incidence (18.91%) in elite male soccer players was not directly associated with lateral abdominal muscles’ thickness, CSA of LM, hamstring flexibility, isometric endurance of trunk extensor, back muscles’ flexibility, and leg length discrepancy during the one season follow-up period. Alteration in these factors may be responsible for LBP recurrence, and its investigation is suggested for future studies.
The incidence of LBP in elite soccer players was estimated to be near 19 percent (7 out of 37), or 1.13 non-traumatic injuries per 1000 training hours, in this 6-month cohort study. In the literature, few studies have evaluated the incidence of LBP injuries in athletes. In the study of Haydt et al. (25), the incidence of LBP was reported at about 56% (50/90) in 90 female field hockey players between 18 and 24 years old. On the other hand, Newlands et al. (26) revealed the LBP’s incidence near 1.78 injuries per 1000 training hours in elite rowers. Also, Walden et al. (27) illustrated that the incidence of LBP in northern and southern groups of professional European football clubs was about 0.20 and 0.10 injuries per 1000 exposure hours, respectively, during the nine-season prospective cohort study. Besides, Mueller et al. (28) mentioned that the incidence of LBP is about 15% in adolescent soccer players. Moreover, Hangai et al. (29) reported that in soccer players, the LBP odds ratio is approximately 1.6 (CI: 1.3 - 2.2). Some of these studies have reported traumatic and non-traumatic injuries separately; others have not differentiated the injuries. Therefore, the inconsistency between the incidence rates of LBP could be due to different studies’ participants, injury definitions, and follow-up periods.
Overweightness and obesity have been suggested as risk factors for LBP in athletes (4). Similarly, the mean BMI and height of the participants, who experienced LBP in our study, were higher compared to the asymptomatic players (BMI = 22.03 ± 1.21 vs. 21.6 ± 1.15), (height = 179.07 ± 3.72 vs. 175.96 ± 8.30). However, the statistical relation between LBP and BMI was not statistically significant. In contrast, the case-control study by Grosdent et al. (30) illustrated a significant relationship between LBP and BMI among soccer players with and without LBP (BMI = 22.6 ± 1.6 vs. 21.2 ± 1.3), (height = 182.2 ± 7.3 vs. 177.3 ± 5.3). Even though the BMI and height differences between the mentioned studies were similar, the number of participants was balanced between the two groups (with LBP and without LBP) in the latter study, and it could be the reason for the significance of the results.
The thickness of trunk muscles (TrA, IO, EO, and LM), which have been measured by the ultrasonography method in both resting and contraction positions did not show a statistically significant difference between players with or without LBP at the baseline of this cohort study. Previous studies have shown that there is a relationship between LBP and trunk muscles’ size and contraction ability in different athletes (6, 31). In the study of Hides et al. (6), the CSA of the trunk at the L3-4 disc level was measured by using magnetic resonance imaging (MRI), at the beginning and end of the drawing-in maneuver in Australian footballers with LBP. Their results illustrated that there was a significant decrease in the CSA of the trunk in athletes with LBP (6). Also, Hides et al. (6) revealed that in elite soccer players with LBP at the start of the preseason, CSA of LM at L4-L5 level was lower in comparison with players without LBP, and with decreasing the LBP, the CSA of LM was improved (31). The thickness of IO and TrA muscles in contraction were improved significantly in elite cricket players, with and without LBP, who participated in a staged core stabilization training program (32). This cohort study was conducted for assessing the role of trunk muscles’ thickness in the incidence of LBP, and its findings could not confirm the role of these muscles’ thickness as a risk factor for the development of LBP in elite soccer players. It could be hypothesized that after experiencing an episode of LBP, possibly due to disuse or changes in trunk neuromuscular control, the thickness of these muscles decreased, which led to the recurrence of LBP later. Considering the fact that cross-sectional studies cannot investigate the cause and effect relationship between several variables; the contradiction between our study and previous studies could be due to the different designs of these studies.
Furthermore, hamstring flexibility, back flexibility, and back muscles’ endurance (Sorensen test) did not differ between the two groups in this study. In the study of Rostami et al. (7), the lower thickness of TrA and CSA of LM was observed in cyclists with LBP compared to cyclists without LBP. In the same study, no relation was detected in the isometric back strength of the athletes with LBP compared to the ones without LBP. In accordance with our study, Moradi et al. (4), in a systematic review, found insufficient evidence for a possible relation between the forward bending (which consists of both hamstrings) and back flexibility.
Considering the findings of the studies accomplished so far, there are many gaps in discovering the etiology of LBP in soccer players. To the best of our knowledge, this study is the first cohort study designed to discover the effect of lateral abdominal muscles’ size and CSA of LM as risk factors of the incidence of LBP in adult soccer players. As mentioned previously, most of the previous studies on athletes’ LBP are based on a cross-sectional design that has several limitations, such as not specifying causal relations, or in other words, an unclear direction from risk factors to outcome. These studies mainly show an association with no specific cause and effect relation. Furthermore, in such studies, the process leading to a disease/disability or the causal factors mentioned as risk factors rest in the past. Together, the aforementioned limitations increase the value of the present study because cohort studies are designed to discover causal links between possible risk factors and outcomes (cause and effect relationships). It is possible that a cohort study can reject the findings obtained by cross-sectional studies. As results in the present study show, there may be an opposite direction between the relation of LBP and trunk muscles’ thickness. It seems that while some studies consider the effectiveness of various movements in the activation of trunk muscles and prevention of low back pain (33, 34), this study could not support the role of these muscles in the incidence of low back pain in male soccer players. Maybe other factors such as overtraining and psychological factors should also be investigated in parallel (35).
As the present study is aimed to explore the etiology of LBP in soccer players, it can be considered as a base for further longitudinal studies. Indeed, we need to establish a standard protocol (valid and reliable) for future cohort studies. Based on the findings from our literature review and also observations, we summarized some recommendations to improve the quality of future studies examining the incidence and probable risk factors of LBP in athletes:
The definition of LBP should be clear and exact, and the same definition should be used in all related studies. A standard definition could be “low back pain is pain between the last rib and lower gluteal fold, which is bad enough to limit or change athletes’ daily routine or sports activities for more than one day” (2).
For more generalizability in cohort studies, following a large sample size considering both genders could be more effective regarding loss to follow-up ratios.
Long term follow-up (at least one year), which covers pre-season, in-season and off-season periods can be more reliable for discovering risk factors in different spans of athletes’ sports history. According to the previous studies, overuse and traumatic injury during a season (31) and in off-season periods, different lifestyles, and training can affect the incidence rate of LBP in athletes.
Investigation of other outcomes beyond LBP incidence, such as neuromuscular injuries and performance could be beneficial.
Evaluation of possible markers involved in LBP could be useful during cohort studies to detect possible mechanisms of LBP.
Measurements such as ultrasonography method and further functional assessments should be done under standardized protocols (see previous references in method) to minimize errors.
It would be better if measurements are performed consecutively (e.g., every week or month) during follow up periods in case of detecting any LBP incidence and related changes in muscles’ size or physical function.
Detection of intrinsic risk factors of LBP (including weight, BMI, change in lumbar range of motion, hip flexor tightness, previous history of LBP and participation in more than one type of sports) and other probable extrinsic risk factors (such as duration of participation in competitive sport, training hours per week and playing position and the type of field, e.g. natural vs. artificial grass) should be evaluated before and during the study (4).
The recurrence rates of LBP during the follow-up period should be evaluated with possible causes.
The effect of different sport-specific movements such as dribbling, jumping, heading during soccer could be considered as risk factors for LBP, and their evaluation could be helpful.
Qualitative studies based on individual interviews with the athletes could further help in discovering the possible mechanisms of LBP in soccer players.
This study aims to cover these considerations as much as possible; however, it has several limitations including studying male players which could affect the generalizability of results, and short follow-up period (only a one-season period), which may have affected the results. Besides, we did not evaluate the type of playing field and participation in other sports. To minimize loss to follow-up of participants, free of charge therapeutic services were offered to players during the follow-up period. Furthermore, the participants were assured that the study’s data would be confidential and only the examiners had access to it.
5.1. Conclusions
While seven participants (18.91%) experienced LBP during the follow-up period, this study showed that soccer players who experienced LBP during the study had no statistically significant differences in their baseline characteristics including abdominal muscles’ thickness, CSA of the LM, hamstring flexibility, back flexibility, muscle endurance, and leg length.