Abstract
Background:
Functional ankle instability (FAI) is a common consequence of ankle sprain injury, especially in high-impact sports.Objectives:
To investigate the effect of six weeks of suspension training with total resistance exercises (TRX) on proprioception and muscle strength in female athletes with FAI.Methods:
Thirty female athletes with FAI (age: 21.9 ± 2.2 years, height: 169.3 ± 4.2 cm, and weight: 59.8 ± 6.1 kg) were randomly assigned to two equally numbered groups: TRX training and controls based on inclusion and exclusion criteria. In the pre-test, the anthropometric variables and also proprioception accuracy and muscle strength of subjects were evaluated by joint angle reset test (JART) and manual muscle testing (MMT) in both dorsiflexion and plantarflexion motions. The training group completed three sessions per week with progressive load for six weeks, and each training session lasted 15 - 20 minutes, whilst control subjects continued with their normal activity without special sport activities. After six weeks of training, all tests performed in the pre-test phase were also performed in the post-test phase. The t-test was used for statistic analysis (α ≤ 0.05).Results:
The findings showed that TRX training significantly improved the proprioception accuracy (P ≤ 0.001) and muscle strength (P ≤ 0.001) in the training group rather than the control group. No statistically significant difference was found in any of the tests between pre-test and post-test for the control group (P > 0.05).Conclusions:
Six weeks of TRX suspension training had a positive effect on strength and proprioception accuracy in female athletes with FAI.Keywords
Resistance Training Joint Instability Rehabilitation Sport Medicine
1. Background
Ankle sprain is the most common of all sports injuries. More than 20 % of patients with a history of ankle sprain suffer from residual problems. This problem is especially common in athletes who frequently perform functional tasks such as jumping, landing, cutting, pivoting, and quick movements (1).
Recurrent, symptomatic ankle sprain and the subjective feeling of ankle instability (or both) due to sensorimotor deficits are extremely common. The sensorimotor deficits and dysfunction of the proprioceptive accuracy in patients who have suffered ankle sprain is one of the most important consequences of FAI (2, 3). Several extrinsic and intrinsic factors may increase the risk of future sprain and proprioceptive system deficits. These include deficits in postural sway, range of motion, voluntary strength, proprioception, and previous sprains (4). There are several studies that have demonstrated that proprioception and muscle strength are strong predictors of ankle sprains (4-6).
Defective ankle sensorimotor systems disturb the postural control system functions, which can affect the accuracy of proprioceptive and muscle strength. Disturbances of muscle tone may, in turn, affect movement performance (7, 8). The proprioception system plays an important role in controlling the balance, and ankle proprioception accuracy is one of its important factors. For the athlete, they provide equilibrium, balance, postural, and motor control (7, 9). Ultimately, the muscle strength, postural stability, and mobility in athletic performance is reduced, which is associated with re-injury or multiple injuries, particularly in athletes with FAI and proprioceptive dysfunction (5).
Proprioceptive and sensorimotor training are techniques for improving the proprioceptive system, especially in athletes with FAI (5). In recent years, TRX training has received the interest of the sports community. The ease of implementation, diversity of exercises, and applicability in different places for different age groups is among the factors that add to the attractiveness of this training method. The proper activation of the core stability muscles is another prominent feature of this training (10).
The results indicated that the core stability is essential for force transmission from the trunk to the ground and in sports activities provides proximal stability for distal mobility (9, 11). In addition, due to the importance of pelvic stability in performing lower extremity functional tasks in FAI, the proximal region trunk muscles are used to compensate for the neuromuscular defect of the distal region muscles, such as in FAI (12). Accordingly, TRX training seems to have the ability to simultaneously develop mobility, strength, and joint stability on all anatomical planes.
However, the literature on the impact of TRX training on improving the FAI impairments, such as proprioceptive accuracy and muscle strength deficit, is not very rich. As mentioned earlier, in athletes with FAI, motor control programs and the sensorimotor system are impaired. Furthermore, female athletes are more likely to suffer ankle injuries compared to males (5). Therefore, it is important to evaluate the effectiveness of training methods to reduce the risk of ankle sprains, especially in female athletes.
2. Objectives
Hence, this study investigates the effects of six weeks of TRX suspension training on proprioception and muscle strength in female athletes with FAI. We hypothesized that (1) TRX training improves the accuracy of proprioception in the ankle joint in both dorsiflexion/plantarflexion; and (2) TRX increases the strength of the dorsiflexor and plantar flexor muscles.
3. Methods
3.1. Study Design and Ethics
The present study was a pretest-posttest control group experimental design with two groups. Ethical principles are based on the Declaration of Helsinki. This single-blinded randomized controlled trial was approved by the ethical committee of Qazvin Medical University (code: IR.QUMS.REC.1398.029).
3.2. Participants
Female subjects aged 18 - 25 years and suffering from FAI volunteered to participate in this study. The sample size was estimated using G power software (G-Power for Windows, version 3.1, Duesseldorf, Heinrich-Heine University) with a statistical power of 95%, effect size of 0.5, and alpha of 0.05. Then, out of 50 volunteers, 30 were selected after screening tests (see Figure 1). The purposive sampling method was applied to select the study participants from basketball, volleyball, and handball team players. In total, subjects were 15 female athletes with FAI who did the TRX protocol (experimental group) and 15 female athletes with FAI who were asked not to do any special sports activities during the study period and only do their usual daily activities (control group). Subjects in both FAI and control groups were matched on the anthropometric variables.
Flowchart of the study design
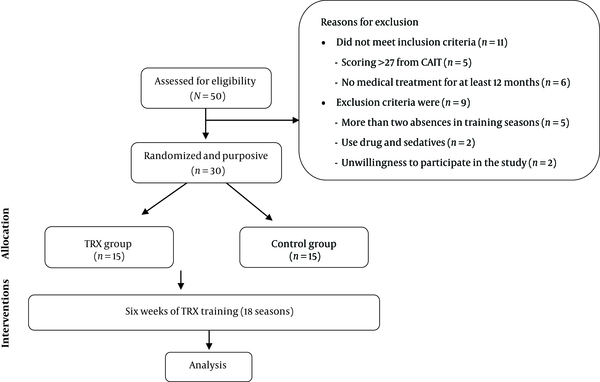
The criteria for participants’ inclusion were: A history of at least two ankle sprain injuries that needed treatment and inactivity in the last two years, at least 3 years of experience in the sport, no medical treatment for at least twelve months prior to the study, full weight-bearing ability, normal walking with full range of motion (ROM) in the ankle joint, scoring ≤ 27 from the cumberland ankle instability tool (CAIT), no pain, weakness, and functional limitation in the affected ankle compared to the other ankle, no disorders in nervous or vestibular systems, or head injury, no histories of participation in any ankle rehabilitation programs over the past 6 months, and a body mass index (BMI) of between 18 and 25 (13). Exclusion criteria were: more than two absences in training sessions, use of drug and sedatives within 48 hours before the study, unwillingness to participate in the study, feeling of severe pain during the study. Also, written informed consent was received from participants prior to inclusion in the study (Figure 1).
3.3. Procedure
Testing sessions were performed at the same time of day for each participant under the same environmental condition (~25°C and ~40% humidity). Body weight and height were measured with a digital scale (0.1 kg and 0.1 cm of accuracy, Health Measuring, model H-300G, China). Percentage of body fat (PBF) was determined using a caliper device (1 mm of accuracy, Lafayette skinfold, model 01127, USA). PBF was calculated by using the Jackson and Pollock formula (14).
3.4. Analysis of Proprioception Accuracy in Ankle Joint
Digital imaging was used to measure the proprioception of the ankle joint with a Sony HD Video Cam. This method is one of the newest methods used to measure the proprioception accuracy in the reset of the ankle joint ROM. This test has acceptable validity and reliability (15). Foot marker placements were: (A) head of fibula; (B) lateral malleolus; (C) lateral calcaneus (just below the lateral malleolus); (D) head of the 5th metatarsal (16). The joint angle reset test (JART): The subject sat on the chair and wore goggles, and her foot did not touch the ground. Proprioceptive differences were measured in the dominant ankle joint. Initially, the subject had 10° passive dorsiflexion (with examiner assistance and measurement by a goniometer). Subjects were asked to maintain the angle for five seconds and to pay attention to the joint position (17). In this position, the first photo was taken from the outside of the ankle, and then the ankle was returned to the resting position. Then, after seven seconds of rest, the subject moved actively to reset the former angle. This action was tested three times, and with each repetition, the reset angle was photographed to record the mean error of the three ankle joint dorsiflexions. The differences between the three angles were compared as an index of proprioception accuracy in the ankle joint. All of the above was done during the plantar flexion movement with the difference that the subject had 20° passively plantar flexion by examiner. All photos are taken from a distance of 185 cm from the subject’s seat, and the camera lens is at ankle height. The photos are then transferred to a computer and analyzed by the KINOVEA software (an open-source software; https://www.kinovea.org) for the ankle angle reset error (18, 19).
3.5. Ankle Muscle Strength Measurement
Manual muscle test (MMT) is used to determine the extent and degree of muscular weakness resulting from disuse or injury. MMT assessment was used to evaluate the strength of the dorsiflexor and plantar flexor muscles. This test has acceptable validity and reliability (20). In this method, the evaluation examines the strength of the dorsiflexor and plantarflexor muscles by applying resistance to dorsiflexion and plantar flexion of the ankle. A handheld dynamometer (Lafayette Instrument, model 01165, USA) was used to assess strength. The instrument was calibrated and remained unused before the test (21). To conduct a MMT, the subject was in supine position for isolating the muscle and positioning so that the muscle works against manual resistance. The test was performed by asking the subject to move the ankle (dorsi/plantar flexion) through the full available ROM. To perform the test, the examiner stabilizes the joint with one hand and resists the movement of the subject’s limb with the other hand, and the subject must move her limb against the resistance with utmost force. Grades are assigned on a 0 - 5 scale (1 = trace score, 2 = poor, 3 = fair, 4 = good, 5 = normal). Grades > 1 demonstrate motion, and grades > 3 are against manual resistance. The examiner must have sufficient experience and perform this test based on the demographic characteristics of the subjects (21, 22).
3.6. TRX Protocol
After the initial test (pre-test), the experimental group trained three times per week for six weeks for non-consecutive days and at the same time of the day. The rest interval was one or two minutes between the two exercises. The first 10 minutes of the session were devoted to warm-up followed by 15 to 20 min of selected TRX exercises under the supervision of the researcher, and the last 5 minutes of the session was devoted to stretching for cool-down (23). Before starting the program, two sessions were intended to familiarize the participants with the exercises. TRX exercises were based on related references and articles published in the field of suspension TRX exercises (10, 23). The training program was a combination of exercises for large muscle groups and several anatomical planes. The TRX training program was performed using the TRX device (TRX PRO3 Suspension Trainer System, USA). The TRX device was mounted on a rod connected 2.44 meters above the ground (10). According to common training principles, the progression of intensity and difficulty is realized through 5 - 6 progressively advancing stages of difficulty (level 1 or 2: easiest level; level 5 or 6: most difficult level) for each exercise. With respect to the different levels, increasing difficulty is achieved through the principles of FITT (frequency, intensity, time spent, and type of exercise) and then confirmed by a specialist physician (24). Tables 1 and 2 presented the level of movement along with the TRX training protocol.
Movement Level for TRX Protocol
| Movement | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Level 6 |
|---|---|---|---|---|---|---|
| (A) Squat | Squat | Squat-ankle plantar | Fixed squat- ankle plantar | |||
| (B) Hamstring | Hamstring | Hamstring-abduction | Hamstring curl | S.L. hamstring | ||
| (C) Lunge | Forward lunge | Forward lunge | S.L. lunge | S.L. lung with ball | ||
| (D) Single leg squat | S.L. squat | S.L. squat with leg swing | S.L. squat to lateral | |||
| (E) Jump landing | Squat jump | Squat jump F-B | Squat jump with Ball | S.L. squat Jump | S.L. squat Jump F-B | S.L. squat jump with ball |
| (F) Cutting | Squat jump | S.L. squat jump R-L | S.L. squat jump with ball |
TRX Training Session Protocol
| Seasons | Movement Type and Difficulty Levels (Sets × Seconds) | |||||
|---|---|---|---|---|---|---|
| 1 | A1 (3 × 30) | B1 (3 × 25) | C1 (3 × 25) | |||
| 2 | A1 (3 × 30) | B1 (3 × 25) | C1 (3 × 25) | |||
| 3 | A1 (3 × 35) | B1 (3 × 30) | C1 (3 × 35) | |||
| 4 | A2 (3 × 35) | B2 (3 × 30) | C2 (3 × 35) | |||
| 5 | A2 (3 × 35) | B2 (3 × 30) | C2 (3 × 35) | |||
| 6 | A3 (3 × 35) | B3 (3 × 30) | C2 (3 × 35) | |||
| 7 | A3 (3 × 35) | B3 (3 × 30) | C3 (3 × 35) | D1 (3 × 25) | ||
| 8 | B4 (3 × 25) | C3 (3 × 35) | D1 (3 × 25) | D2 (3 × 20) | E1 (3 × 20) | |
| 9 | B4 (3 × 25) | C3 (3 × 40) | D1 (3 × 30) | D2 (3 × 25) | E1 (3 × 25) | |
| 10 | C4 (3 × 40) | D2 (3 × 30) | E1 (3 × 25) | E2 (3 × 25) | E3 (3 × 25) | |
| 11 | C4 (3 × 45) | D2 (3 × 30) | E2 (3 × 25) | E3 (3 × 25) | E4 (3 × 25) | F1 (3 × 30) |
| 12 | C4 (3 × 45) | E2 (3 × 30) | E3 (3 × 30) | E4 (3 × 25) | E5 (3 × 25) | F1 (3 × 20) |
| 13 | E3 (3 × 35) | E4 (3 × 30) | E5 (3 × 20) | E6 (3 × 35) | F1 (3 × 20) | F2 (3 × 20) |
| 14 - 18 | E4 (3 × 30) | E5 (3 × 25) | E6 (3 × 25) | F1 (3 × 40) | F2 (3 × 20) | F3 (3 × 25) |
3.7. Statistical Analysis
Statistical analysis was performed using SPSS (SPSS 19 for Windows, USA). Data were analyzed and confirmed for normality using the Shapiro-Wilk test. Therefore, parametric methods were used for data analysis. To determine the similarity between the groups in baseline, the anthropometric variables were compared using independent t-tests. The independent t-test was used to examine differences between the groups. Statistical significance was set at P < 0.05.
4. Results
Table 3 shows the demographic characteristics of the subjects. There was no significant difference between subjects in both groups concerning age, weight, height, BMI, and PBF (P > 0.05).
Based on the results of t-test as shown in Table 3, a significant improvement was found in the experimental group over the control group that for JART in dorsiflexion (t = 4.63, df = 28, P < 0.001), in plantar flexion (t = 10.25, df = 28, P < 0.001), for MMT in dorsiflexion (t = 5.25, df = 28, P < 0.001), and in plantar flexion (t = 8.04, df = 28, P < 0.001). Also, significant improvement was observed in the experimental group before and after TRX intervention for JART in dorsiflexion (t = 8.03, df = 14, P < 0.001), in plantar flexion (t = 8.15, df = 14, P < 0.001), for MMT in dorsiflexion (t = 6.76, df = 14, P < 0.001), in plantar flexion (t = 7.32, df = 14, P < 0.001), which means TRX training improves the accuracy of proprioception and ankle joint muscle strength in both dorsiflexion/plantarflexion motions.
Characteristics of Randomized Women, JART and MMT Scores (Mean ± SD)
| Variable | Experimental (N = 15) | Control (N = 15) | P-Valuea |
|---|---|---|---|
| Age, y | 22.01 ± 1.75 | 21.83 ± 2.05 | 0.798 |
| Weight, kg | 60.38 ± 6.15 | 59.20 ± 5.37 | 0.580 |
| Hight, cm | 170.03 ± 4.49 | 168.33 ± 3.89 | 0.277 |
| BMI, kg/m2 | 20.89 ± 0.33 | 20.97 ± 0.21 | 0.435 |
| PBF, % | 24.73 ± 0.69 | 24.79 ± 0.75 | 0.821 |
| JART for anke dorsiflexion, degrees | |||
| Baseline | 4.67 ± 0.64 | 5.01 ± 0.88 | 0.185 |
| Post intervention | 2.33 ± 0.93 | 3.97 ± 1.01 | < 0.001b |
| P-valuec | < 0.001b | 0.122 | |
| JART for ankle plantar flexion, degrees | |||
| Baseline | 6.12 ± 1.44 | 7.01 ± 0.59 | 0.371 |
| Post intervention | 2.33 ± 1.08 | 6.0 ± 0.87 | < 0.001b |
| P-valuec | < 0.001b | 0.220 | |
| MMT for anke dorsiflexion, scores | |||
| Baseline | 3.1 ± 0.85 | 3.4 ± 0.61 | 0.320 |
| Post intervention | 5.3 ± 0.93 | 3.4 ± 1.05 | < 0.001b |
| P-valuec | < 0.001b | 0.160 | |
| MMT for ankle plantar flexion, scores | |||
| Baseline | 3.3 ± 0.75 | 2.0 ± 0.83 | 0.240 |
| Post intervention | 5.2 ± 0.67 | 3.4 ± 0.55 | < 0.001b |
| P-valuec | < 0.001b | 0.160 |
5. Discussion
The aim of this investigation was to determine whether six weeks of TRX suspension training would improve the accuracy of proprioception and ankle joint muscle strength in both dorsiflexion/plantarflexion motions in female athletes with FAI. The main finding in this study is that six weeks of TRX suspension training can significantly improve the accuracy of proprioception and ankle joint muscle strength in both dorsiflexion/plantarflexion motions. Similarly, a previous study showed that deficits in strength, proprioception, balance, muscular imbalance, and functionality in athletes with FAI have a positive effect through training programs that have an essence of strength, stability, and accuracy of proprioception (25-28). A systematic review of proprioceptive exercises resulted in significant improvement in ankle function, and also have shown that using exercises that involve the neuromuscular system improves the links between neuromuscular pathways and, by reducing the delay in proprioceptive sensory function, significantly reduces the acute injuries in knees and ankles (26, 29).
Before and during a motor command (athletes in all sports that involve jumping and side-stepping), the motor control system must consider the different positions of the joint and consider the complex mechanical regulation of the musculoskeletal system (30). Motor programs should be re-adjusted for unexpected disorders or changes in external stimuli. Although the visual sense is considered the main source of input information, the proprioceptive source of information is rather accurate (31). The central nervous system (CNS) uses proprioceptive sensory information to construct a representation of body position and muscle activity that is critical in initiating and refining centrally driven motor control. Proprioceptive information influences voluntary commands in supraspinal motor centers necessary for neuromuscular control of postural mobility (32). In other words, any change or modification of pre-stored motor control programs depends on proprioception (6). Proprioception relates primarily to the position sense of mechanoreceptors. Mechanoreceptors convert mechanical changes into nerve signals and send them to the CNS through the sensory pathways (19). The high accuracy of proprioception and sensory information received from articular receptors are important because the nervous system uses sensory information to maintain stability and safety in the joint by sensory triggering either in feedback or feedforward mechanisms (13). Proprioception with the complex neuromuscular process maintains motor stability and orientation along with stability during activities (26). Muscle spindles and tendon organs are proprioceptive sensors that play an important role in motor control (19). The nervous system, along with proprioceptive information, has the ability to correct and restore the motor control programs that were disturbed and, when necessary, send the correct movement instructions to the muscles responsible for controlling and performing movement in different joints (13, 29). It seems that the TRX training while enhancing the accuracy of the proprioceptive information affects the motor control system outputs and has a significant role in improving the movements’ accuracy.
Another factor that can play a major role in creating dynamic joint stability, especially when sudden forces are applied to the joint, is increased muscle tone around the joint or increased muscle stiffness. Moreover, proprioception represents the discriminating ability of joint muscle strength (19). It seems that the contribution of various exercises in improves the proprioceptive sense, and only in dynamic conditions, all muscle receptors are activated, and the proprioceptive sense is strengthened (13). The positive effects of strength training have been highlighted in the rehabilitation of injured athletes and their return to sports (30). Athletes with ankle sprain injuries, followed by FAI, have impaired muscle activation control programs, and this affects the extent and manner of activation of the ankle muscles. Therefore, it has been reported that these athletes encounter muscle weakness and impaired accuracy of the ankle joint. The TRX training can play a great role in improving the strength of the lower-limb muscles due to their suspension-strength nature. Comparing the TRX and traditional strength training, Janot et al. found that as a result of the five weeks training, the balance of subjects is increased by increasing the strength of the lower-limb muscles and increasing the activity of the core stability muscles through the TRX training (24).
Johnson et al. suggested that the exercises involving core muscle stability can increase the awareness of the overall proprioception. By activating articular receptors and proprioception, it modifies the motor control programs sent by the CNS (5, 33).
In athletes, for compensating the icurred instability, higher levels of ankle muscle co-contractions are required to maintain their ankle stability. However, due to weakness in the ankle muscles, disturbances in the transmission of sensory information, as well as motor information, they have to rely more on the hip strategy to correct their movements (13). Athletes with FAI change the patterns of lower limb muscle activity in unexpected and unstable conditions, and it seems that the proximal muscles work harder and faster than the distal muscles of the lower limbs (34). The evidence presented in previous studies shows that the antagonist muscles have the ability to better maintain the joint in conditions of disorder when the muscles have the strength and tension necessary to maintain the joint (22). Strength training can play an important role in promoting antagonistic muscles and maintaining joint stability, even without deliberately changing the athlete’s motion patterns. The contraction of the ankle antagonist muscles also increases the stiffness of the joint and can increase the stability of the ankle joint and prepare it to control the rapid and intense change in the length of the tendon-muscle complex and rapid movements (21, 22). Considering the previous studies, exercises with traction-contraction mechanisms can improve and change the start of muscular activity and may also indirectly affect the feedforward. This mechanism is considered in the treatment and prevention of lower limb injuries (32).
A great deal of research suggests that TRX suspension training programs include exercises that involve and improve components such as balance, strength, endurance, strength, proprioceptive sensory function, motor function, and ROM by changing the center of gravity, body weight load and open and closed kinetic chain, and can be useful for athletes with FAI (23, 33). The lower limb proximal muscles act better and more accurately to compensate for ankle injuries and delays in starting activity during perturbation with different orientations and speeds (34). It should also be noted that the neuromuscular, proprioception system, and motor control disorders are not limited to the ankle joint and depend on the entire lower kinetic chain (35). Closed kinetic chain exercises are considered the best way to maximize the output of mechanical receptors. Researches have shown that closed chain exercises have the best effect on retraining reflex responses and sensorimotor facilitation of the lower limbs (11). It seems, the exercises designed in this study may be able to improve joint stability by improving the efficiency of sensory receptors and neuromuscular facility and muscle strength while improving the proprioceptive sense of the joints.
5.1. Conclusions
The improvement of proprioceptive accuracy and muscle strength in the training group can be attributed to the improved quality of information sent from the ankle joint proprioceptive mechanoreceptors to the CNS, which controls the movement patterns of the ankle joint. The TRX suspension training program used in this study had a positive effect on proprioception and muscle strength in female athletes with FAI. It seems that TRX suspension training can be a good method to rehabilitate athletes with FAI due to their weight bearing and closed kinetic chain in different ROMs in the ankle.
5.2. Limitations
Although this study has considerable practical application, a limitation of the study was the low number of subjects. The subjects were recruited from only three ball sports. The duration of training interventions was short. The poor description of the subjects’ characteristics, in particular, was a measure of the severity of the FAI and how the subjects were selected. Further, fully powered studies were required to investigate efficacy and its validity.
Regarding the study’s results, we recommend that it is better for female athletes with a history of FAI to use TRX suspension training as a great complement in rehabilitation and physical fitness, reducing the risk of ankle re-injury and sport deprivation.
Acknowledgements
References
-
1.
Tropp H. Commentary: Functional Ankle Instability Revisited. J Athl Train. 2002;37(4):512-5. [PubMed ID: 12937576]. [PubMed Central ID: PMC164386].
-
2.
Li HY, Zheng JJ, Zhang J, Hua YH, Chen SY. The Effect of Lateral Ankle Ligament Repair in Muscle Reaction Time in Patients with Mechanical Ankle Instability. Int J Sports Med. 2015;36(12):1027-32. [PubMed ID: 26212242]. https://doi.org/10.1055/s-0035-1550046.
-
3.
Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E. Single-leg drop landing motor control strategies following acute ankle sprain injury. Scand J Med Sci Sports. 2015;25(4):525-33. [PubMed ID: 24975875]. https://doi.org/10.1111/sms.12282.
-
4.
de Noronha M, Refshauge KM, Herbert RD, Kilbreath SL, Hertel J. Do voluntary strength, proprioception, range of motion, or postural sway predict occurrence of lateral ankle sprain? Br J Sports Med. 2006;40(10):824-8. discussion 828. [PubMed ID: 16920769]. [PubMed Central ID: PMC2465053]. https://doi.org/10.1136/bjsm.2006.029645.
-
5.
Caldemeyer LE, Brown SM, Mulcahey MK. Neuromuscular training for the prevention of ankle sprains in female athletes: a systematic review. Phys Sportsmed. 2020;48(4):363-9. [PubMed ID: 32067546]. https://doi.org/10.1080/00913847.2020.1732246.
-
6.
Hastings M, Nixon D, McCormick J. Baxter's The Foot and Ankle in Sport. 3rd ed. Elsevier; 2020.
-
7.
Ivanenko Y, Gurfinkel VS. Human Postural Control. Front Neurosci. 2018;12:171. [PubMed ID: 29615859]. [PubMed Central ID: PMC5869197]. https://doi.org/10.3389/fnins.2018.00171.
-
8.
Kemler E, van de Port I, Backx F, van Dijk CN. A systematic review on the treatment of acute ankle sprain: brace versus other functional treatment types. Sports Med. 2011;41(3):185-97. [PubMed ID: 21395362]. https://doi.org/10.2165/11584370-000000000-00000.
-
9.
Irandoust K, Taheri M, Mirmoezzi M, H'Mida C, Chtourou H, Trabelsi K, et al. The Effect of Aquatic Exercise on Postural Mobility of Healthy Older Adults with Endomorphic Somatotype. Int J Environ Res Public Health. 2019;16(22). [PubMed ID: 31717625]. [PubMed Central ID: PMC6888232]. https://doi.org/10.3390/ijerph16224387.
-
10.
Dawes J. Complete guide to TRX suspension training. Human Kinetics; 2017.
-
11.
Mirmoezi M, Taheri M. Effects of Closed and Open Kinetic Chain Exercise Induced-Localized Fatigue on Static and Dynamic Balance in Trained Individuals. Asian J Sports Med. 2018;In Press(In Press). https://doi.org/10.5812/asjsm.80069.
-
12.
Gribble PA, Hertel J, Denegar CR, Buckley WE. The Effects of Fatigue and Chronic Ankle Instability on Dynamic Postural Control. J Athl Train. 2004;39(4):321-9. [PubMed ID: 15592604]. [PubMed Central ID: PMC535524].
-
13.
Kalantariyan M, Minoonejad H, Rajabi R, Seidi F. Effects of Functional Ankle Instability on Balance Recovery Strategy in Athletes. Phys Treat. 2018:99-106. https://doi.org/10.32598/ptj.8.2.99.
-
14.
Reilly T. Kinanthropometry and Exercise Physiology Laboratory Manual: Tests, Procedures and Data. 2. Routledge; 2013. https://doi.org/10.4324/9780203868737.
-
15.
Deshpande N, Connelly DM, Culham EG, Costigan PA. Reliability and validity of ankle proprioceptive measures. Arch Phys Med Rehabil. 2003;84(6):883-9. [PubMed ID: 12808543]. https://doi.org/10.1016/s0003-9993(03)00016-9.
-
16.
Kim EJ, Shin HS, Lee JH, Kyung MG, Yoo HJ, Yoo WJ, et al. Repeatability of a Multi-segment Foot Model with a 15-Marker Set in Normal Children. Clin Orthop Surg. 2018;10(4):484-90. [PubMed ID: 30505418]. [PubMed Central ID: PMC6250958]. https://doi.org/10.4055/cios.2018.10.4.484.
-
17.
Khanmohammadi R, Someh M, Ghafarinejad F. The effect of cryotherapy on the normal ankle joint position sense. Asian J Sports Med. 2011;2(2):91-8. [PubMed ID: 22375224]. [PubMed Central ID: PMC3289203]. https://doi.org/10.5812/asjsm.34785.
-
18.
Hisham NAH, Nazri AFA, Madete J, Herawati L, Mahmud J. Measuring ankle angle and analysis of walking gait using kinovea. International Medical Device and Technology Conference. 2017. p. 247-50.
-
19.
Li L, Ji ZQ, Li YX, Liu WT. Correlation study of knee joint proprioception test results using common test methods. J Phys Ther Sci. 2016;28(2):478-82. [PubMed ID: 27065533]. [PubMed Central ID: PMC4792994]. https://doi.org/10.1589/jpts.28.478.
-
20.
Cuthbert SC, Goodheart GJ. On the reliability and validity of manual muscle testing: a literature review. Chiropr Osteopat. 2007;15:4. [PubMed ID: 17341308]. [PubMed Central ID: PMC1847521]. https://doi.org/10.1186/1746-1340-15-4.
-
21.
Hall EA, Docherty CL, Simon J, Kingma JJ, Klossner JC. Strength-training protocols to improve deficits in participants with chronic ankle instability: a randomized controlled trial. J Athl Train. 2015;50(1):36-44. [PubMed ID: 25365134]. [PubMed Central ID: PMC4299733]. https://doi.org/10.4085/1062-6050-49.3.71.
-
22.
Durfee WK, Iaizzo PA. Rehabilitation and Muscle Testing. Encyclopedia of Medical Devices and Instrumentation. 2006. https://doi.org/10.1002/0471732877.emd226.
-
23.
Gaedtke A, Morat T. TRX Suspension Training: A New Functional Training Approach for Older Adults - Development, Training Control and Feasibility. Int J Exerc Sci. 2015;8(3):224-33. [PubMed ID: 27182415]. [PubMed Central ID: PMC4833470].
-
24.
Aslani M, Minoonejad H, Rajabi R. Comparing the Effect of TRX Exercise and Hoping on Balance in Male University Student Athletes. Phys Treat. 2018:241-50. https://doi.org/10.32598/ptj.7.4.241.
-
25.
Holm I, Fosdahl MA, Friis A, Risberg MA, Myklebust G, Steen H. Effect of neuromuscular training on proprioception, balance, muscle strength, and lower limb function in female team handball players. Clin J Sport Med. 2004;14(2):88-94. [PubMed ID: 15014342]. https://doi.org/10.1097/00042752-200403000-00006.
-
26.
Postle K, Pak D, Smith TO. Effectiveness of proprioceptive exercises for ankle ligament injury in adults: a systematic literature and meta-analysis. Man Ther. 2012;17(4):285-91. [PubMed ID: 22459604]. https://doi.org/10.1016/j.math.2012.02.016.
-
27.
Sekir U, Yildiz Y, Hazneci B, Ors F, Aydin T. Effect of isokinetic training on strength, functionality and proprioception in athletes with functional ankle instability. Knee Surg Sports Traumatol Arthrosc. 2007;15(5):654-64. [PubMed ID: 16770637]. https://doi.org/10.1007/s00167-006-0108-8.
-
28.
Thompson KR, Mikesky AE, Bahamonde RE, Burr DB. Effects of physical training on proprioception in older women. J Musculoskelet Neuronal Interact. 2003;3(3):223-31. [PubMed ID: 15758345].
-
29.
Hubscher M, Zech A, Pfeifer K, Hansel F, Vogt L, Banzer W. Neuromuscular training for sports injury prevention: a systematic review. Med Sci Sports Exerc. 2010;42(3):413-21. [PubMed ID: 19952811]. https://doi.org/10.1249/MSS.0b013e3181b88d37.
-
30.
Ismail MM, Ibrahim MM, Youssef EF, El Shorbagy KM. Plyometric training versus resistive exercises after acute lateral ankle sprain. Foot Ankle Int. 2010;31(6):523-30. [PubMed ID: 20557819]. https://doi.org/10.3113/FAI.2010.0523.
-
31.
Riemann BL, Lephart SM. The Sensorimotor System, Part II: The Role of Proprioception in Motor Control and Functional Joint Stability. J Athl Train. 2002;37(1):80-4. [PubMed ID: 16558671]. [PubMed Central ID: PMC164312].
-
32.
Lederman E. Neuromuscular rehabilitation. Neuromuscular Rehabilitation in Manual and Physical Therapy. 2010. p. 169-71. https://doi.org/10.1016/b978-0-443-06969-7.00014-0.
-
33.
Chen ET, Borg-Stein J, McInnis KC. Ankle Sprains: Evaluation, Rehabilitation, and Prevention. Curr Sports Med Rep. 2019;18(6):217-23. [PubMed ID: 31385837]. https://doi.org/10.1249/JSR.0000000000000603.
-
34.
Kazemi K, Arab AM, Abdollahi I, Lopez-Lopez D, Calvo-Lobo C. Electromiography comparison of distal and proximal lower limb muscle activity patterns during external perturbation in subjects with and without functional ankle instability. Hum Mov Sci. 2017;55:211-20. [PubMed ID: 28843163]. https://doi.org/10.1016/j.humov.2017.08.013.
-
35.
Webster KA, Pietrosimone BG, Gribble PA. Muscle Activation During Landing Before and After Fatigue in Individuals With or Without Chronic Ankle Instability. J Athl Train. 2016;51(8):629-36. [PubMed ID: 27626836]. [PubMed Central ID: PMC5094841]. https://doi.org/10.4085/1062-6050-51.10.01.
