Abstract
Background:
The most common musculoskeletal disorder among military personnel, especially office workers, is chronic low back pain due to lumbar disc herniation.Objectives:
This study aimed to investigate the effect of selected motor control retraining exercises after conventional treatments on the persistence of changes in pain, functional disability, and range of motion in male military personnel with lumbar disc herniation.Methods:
Military personnel with lumbar disc herniation were divided into two groups of intervention (N = 18) and control (N = 18) after 10 sessions of conventional exercises. The intervention group performed 60 minutes of motor control retraining exercises three times a week for eight weeks, while the control group continued the usual stretching for back pain.Results:
The average scores of pain intensity, functional disability, and range of motion after conventional and selected motor control retraining exercises showed a significant difference (P < 0.001).Conclusions:
Motor control retraining exercises after conventional treatments can improve pain, functional disability, and range of motion in male military personnel with chronic back pain caused by lumbar disc herniation. This technique may improve the quality of life and function for military personnel who are at high risk of this disorder. More research is needed to confirm these findings and examine the intervention's long-term effects. These physical exercises may be appropriate for treating people with similar symptoms.Keywords
Chronic Low Back Pain Lumbar Disc Herniation Male Military Personnel Pain Selected Motor Control Retraining Exercises
1. Background
Low Back Pain (LBP), defined as the pain, strain, or stiffness of subchondral or supra-gluteal muscles with or without sciatic pain, is one of the most prevalent musculoskeletal disorders in various populations (1, 2). LBP is also a common problem among military personnel, especially office clerks with a sedentary and sitting position for 7 to 8 working hours a day (3, 4). One of the reasons for LBP and radicular leg pain is intervertebral disc herniation-associated radiculopathy, which compresses the spinal nerve roots (5). Nearly 5% of people with LBP suffer from disc herniation (6). Bulging or herniation of intervertebral discs is one of the leading causes of pain and dysfunction of core stabilizing muscles. Although the precise mechanism behind this dysfunction has not yet been discovered (7), factors such as poor posture, non-standard chairs, and long-time sitting positions may accelerate disc degeneration and atrophy of core stabilizing muscles (7). Increased pressure on the intervertebral discs can result in an alteration of their structure and metabolic function. Thus, the height of intervertebral discs is decreased due to disc dehydration, leading to contact between articular surfaces and, consequently, decreased range of motion (8). This process alters the function of core stabilizing muscles, including rectus abdominalis, transverse abdominalis, internal and external obliques, diaphragm, and pelvic floor muscles (9). It has been reported that the height of intervertebral discs is decreased by one to four millimeters following a continuous 30-minute sitting position (10). So, these consequent changes of long-time sitting can be considered the main reasons for LBP, intervertebral canal stenosis, and radicular pain in the legs (11, 12). Researchers should seek an appropriate solution for managing and preventing intervertebral disc degeneration and dysfunction of core stabilizing muscles in people with sedentary jobs (13-15).
Previous studies have suggested interventions like physiotherapy, aqua therapy, manual therapy, stretching, and therapeutic exercises for preventing disc degeneration or treating injured discs in people with sedentary jobs (16, 17). However, in these interventions, the lack of retraining to control the lumbar-pelvic position during daily activities and exercise has caused the return of pain. Also, the lack of control of muscle contraction in daily activities and training will cause less activation of the relevant muscles, and the improvement and persistence of the intervention will be less (18). Despite the availability of various studies on LBP, there is a controversy regarding the most appropriate therapeutic intervention (18). Moreover, most patients desire pain reduction and rapid return of functional abilities due to economic reasons, so researchers are investigating modern scientific methods for better outcomes, including motor control exercises. These exercises aim to motor control inefficient muscle groups and augment their efficacy by correcting movement patterns (19). It has been proven that motor control training is efficacious in patients with chronic low back pain (20-23). Previous research has shown a dysfunction in deep muscles (e.g., transverse abdominals and multifidus) control for preserving stability in people with LBP (24). In addition, motor control exercises use motor learning principles such as retraining core muscle control, body posture, and motor patterns, leading to pain and disability reduction (21, 25, 26).
However, these studies have been conducted on patients with nonspecific low back pain, and there is a lack of sufficient studies on the effects of motor control exercises on LBP. In addition, to the best of our knowledge, there are no studies assessing the effects of retraining exercises and, more importantly, retraining after conventional treatments such as physiotherapy on disc herniation, especially in military personnel.
2. Objectives
The present study aimed to provide a comprehensive and safe protocol for using motor control retraining exercises at work and home to persistently manage intervertebral disc herniation-related low back pain. We hypothesized that patients with radicular discographies who perform motor control retraining exercises after conventional physiotherapy have more persistent improvements than those who receive conventional physiotherapy treatments alone, And the present study answers whether selected motor control retraining exercises after ten sessions of conventional treatments have an effect on the persistence of changes in pain, functional disability, and range of motion in male military personnel with lumbar disc herniation.
3. Methods
3.1. Study Design and Subjects
The present study was a randomized controlled trial with a pre- and post-test design consisting of intervention and control groups during the months of April–December 2022. It was conducted on male military personnel with chronic low back pain due to intervertebral disc herniation. The sample was selected from a list of patients referred to the special armed forces clinic in Tehran, Iran, who were visited by an experienced neurologist. The protocol of this study was registered at the Ethics Committee of Baqiyatallah University of Medical Sciences, Tehran, Iran (Ethical No. IR.BMSU.BAQ.REC.1400.063).
Also, patients signed an informed consent form before entering the study. The sample size was calculated using G*Power software considering an effect size of 0.25, power of 95%, and α level of 0.05, amounting to a minimum of 15 patients in each group (27). 30% was added to the final volume of the sample due to the possible loss of the samples. A sports medicine specialist assessed the patients' eligibility based on their medical documents, including radiographic, Magnetic Resonance Imaging (MRI), and electromyography nerve conduction velocity (EMG). Finally, 40 men with chronic low back pain due to intervertebral disc herniation were selected according to inclusion criteria and clinical evaluation. We included patients with chronic low back pain due to herniated L4-L5 or L5-S1 discs. Their age range is between 30 and 55 years. BMI between 25 and 30, and history of a three-month LBP with a severity of 3 or more based on the 0 to 10 Visual Analog Scale (VAS) (28), lack of previous fracture or surgery in the spinal vertebrae, osteoarthritis, rheumatologic diseases, and those with no therapeutic interventions (e.g., physiotherapy) in the last three months before the study (18). We excluded patients who had worsened pain or taken medications after the first three sessions of physiotherapy, were unable to perform exercises, were not willing to take part in the study, were absent in two consecutive or three intermittent therapeutic sessions, and performed exercises other than the stretching exercises of the control group.
3.2. Instrument
Demographic information and past medical or drug history data were recorded in a pre-designed checklist. Pain scores, functional disability, and range of motion were recorded with the VAS (28), Oswestry disability index (29), and Modifed-Modifed Schober's Test (30, 31), respectively. After receiving 10 sessions of conventional exercises under the supervision of a sports medicine specialist and physiotherapist, all the indices were measured again. Patients were advised to take medications in case of severe pain and report it in the next session.
3.3. Intervention
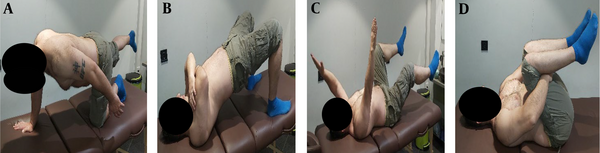
All patients previously received conventional physiotherapy exercises and electrotherapy. Conventional physiotherapy exercises included activating core muscles in the supine, sitting, standing, and crawl positions and usual stretching (32) (Figure 1).
Conventional Exercises
In electrotherapy, a Transcutaneous Electrical Nerve Stimulation (TENS) unit with a frequency of 20 Hz and a pulse width of 100 microseconds was used. Four 5 cm electrodes were placed bilaterally on the imaginary lines of the T12 and S1 vertebrae in the region of the lumbar paraspinal muscles (18, 33).
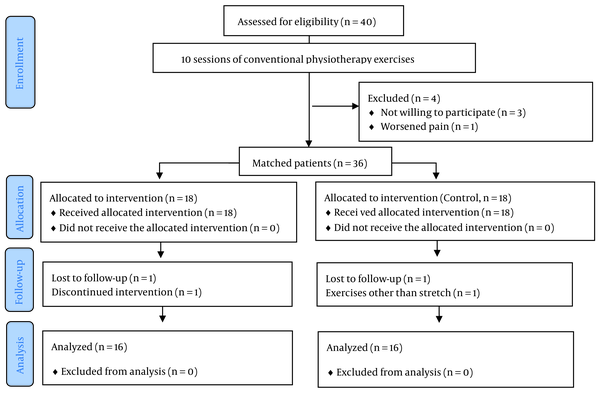
After completing the conventional physiotherapy treatments, 4 patients were excluded from the study. The reasons for leaving patients are listed in the flowchart. 36 patients who met the inclusion criteria were randomly divided into 2 groups: A control group (18 people) and an intervention group (n = 18). A balanced random block (1: 1) with a block size of 4 was used for random assignment. Randomization was done using the website www.randomization.com. To hide the random allocation sequence, numbered sealed envelopes containing groups A or B were used, and the envelopes were given to the clinic secretary. A was the experimental group, and B was the control group. In the present study, the participants and those assessing the outcomes were blinded, while the therapist was not.
The experimental group performed the motor control retraining program for eight weeks in three sessions of 45 to 60 minutes per week under the supervision of a sports medicine specialist. Each patient had five training sessions to practice at home and at work under the supervision of a therapist to have a modified and comprehensive exercise protocol. The control group received no exercise except regular stretching exercises for LBP. Motor control retraining exercises, including proprioception, coordination, and sensory-motor control exercises, were selected based on the principles of researchers such as Sahrmann, Comerford, and Richardson as follows:
a) Training to find the appropriate lumbosacral orientation at rest and control the desired direction during active movement of the femur and spine (18, 19, 34-36),
b) Retraining to activate deep pelvic muscles, including multifidus, transversus abdominalis, and pelvic floor (18, 36), and
c) Supplementary interventions to improve blood circulation, alignment of lumbar joints, and muscle release (18).
For part A, the health care provider taught orientations through visual or auditory routes and touch. First, the pelvis was placed in the correct position by the therapist, and then the proper orientation of the pelvis was taught to the patients during daily life. Each exercise was performed slowly for 2 minutes and 10 times, and the therapist controlled their speed. After four weeks, the patients received specific motor control exercises to learn to put the pelvis in the correct direction during active femur movement.
This section consisted of three stages: (1) In stage I, patients received an educational video clip and were asked to do the exercises twice or thrice daily. Patients were trained to kneel, sit, stand, and control lumbosacral movements with minimal effort during leg and arm movements. These exercises aim for patients to consider a new motor strategy in their daily lives. (2) In stage II, the movement pattern of the muscle was taught by using touch. These exercises aim to decrease the overuse and tightness of superficial muscles and improve the function of stabilizing muscles throughout the joint area. (3) Finally, in stage III, dynamic control of vertebral movements, from the neutral position to an active position for specific and necessary activities, was taught to patients. This stage mainly focused on vertebral movements in various dynamic activities and functional positions of daily life, for example, movements above the head (Figure 2).
Lumbosacral orientation

In part B, we focused on the multifidus, transverse abdominalis, and pelvic floor muscles exercises based on the proposed protocol of Richardson and Hides (18, 36). These exercises were specified for activation and retraining of deep muscle contraction, including common contraction of the pelvic floor, transverse abdominalis muscles, and common contraction of multifidus and transverse abdominals. During transverse abdominal contraction, the Anterior Superior Iliac Spine (ASIS) can be palpated in the medial region on both sides. Following proper activation of the transversus abdominalis, a gradually increasing deep tension is felt in the abdominal wall. The examiner can also place a hand under the lower back that the patient presses during proper contraction. Conversely, if this contraction occurs without proper training, it can lead to a prominent abdominal wall. In addition, the patient may feel a rapidly increasing surface tension in the abdominal wall due to the predominance of the obliques over the transversus abdominalis, and the posterior tilt of the pelvis can be observed. As a considered disorder, the asymmetry between the right and left sides of the abdominal wall during muscle contraction may be subtly expressed and detected by unilateral overactivation of the oblique muscles.
Multifidus muscle contraction is similar to transverse abdominals and occurs as an isometric contraction in the prone position. The examiner touches spinous processes on both sides and assesses the position of the right and left (even higher than lower) multifidus muscles. According to previous studies, the superficial part of this muscle plays a role in the extension of spinal vertebrates, and its contraction should occur segmentally or in each vertebrate. In a proper movement, tension occurs smoothly and deeply, while rapid and superficial tension shows the involvement of the superficial part of the muscle. Also, the prominence of the pectoral part of the muscle and the painful and anterior tilt of the pelvis are indicators of improper movement. The examiner can touch the anterior part of the abdominal wall when assessing multifidus activation. In this situation, the prominence of the abdominal wall indicates the contraction of abdominal muscles to overcome the extension of superficial fibers of the multifidus muscle.
Moreover, the overall condition of the abdomen is assessed in both sitting and standing positions. The superiority of the upper abdominal quadrant over the lower, transverse abdominalis fold and the prominence of the lateral abdominal wall are the indicators of external oblique muscle contraction. Concurrent contraction of the pelvic floor, transverse abdominalis, and multifidus muscles are necessary for stabilizing the spinal vertebrates. Patients who cannot relax internal and external oblique muscles can benefit from retraining pelvic floor muscle contraction. For this purpose, patients are asked to take a supine position with a filled bladder and contract the anterior part of the pelvic floor. In this position, the examiner feels a deep and smooth contraction while touching the inferior quadrant of the abdomen. This position can be repeated in sitting and standing positions during daily activities. Changes in tonicity or prominence of muscle during contraction were taught to patients by touching the considered points by themselves so that they could correctly perform exercises and monitor their progress. Contractions could be maintained for 10 seconds, which could be repeated 10 times to increase the endurance of muscles. The motor control exercise program consisted of a progression from isolated contraction of the transversus abdominis and/or isolated contraction of the multifidi to combined contraction of both transversus abdominis and multifidi muscles in different positions from supine or prone to bridging or four-point kneeling (Figure 4). Each participant was progressed on exercises when they have reached an independent activation of the transversus abdominis and multifidus without overactivity of superficial muscles in an individualized manner (visual observation by the therapist). If the patient could not concurrently contract two muscles, we continued single-muscle contraction exercises (Figure 3).
Also, during the intervention, the therapist alternated the movement combination depending on the tissue resistance and the patient's symptoms. The speed and amplitude of movement were adjusted such that no pain was produced during the technique.
(A) Retraining for isometric contraction of transverse abdominals in crawl position accompanied by touching the anterior abdominal wall. (B) Retraining for isometric contraction of transverse abdominalis is accompanied by touching the anterior abdominal wall, and retraining for isometric contraction of pelvic floor muscles is accompanied by touching the lower abdominal quadrant. (C) Retraining for isometric contraction of multifidus muscle accompanied by touching the lumbosacral side. (D) Retraining for concurrent contraction of transverse abdominalis and multifidus muscles in standing position accompanied by concurrent touching of the anterior abdominal wall and lumbosacral side. (E) Taught changes in tonicity or prominence of muscle during contraction (touching the considered points by themselves)
In part c, patients had five minutes of the bicycle and friction massage, manual therapy, decompression, and stretching of shortened muscles to reduce active trigger points.
3.4. Statistical Analysis
Data were analyzed using Statistical Package for Social Sciences (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp). Descriptive analysis was performed using mean, standard deviation, percentages, and frequencies. The Shapiro-Wilk test was used to check the normal distribution of data. The analysis of covariance test (ANCOVA) was used to compare variables between the groups, and a paired-t test was performed to compare changes before and after the intervention. The effect size was determined using Cohen's coefficient (37).
4. Results
Thirty-two patients met all the criteria, and 4 patients left the study; the reasons for leaving the patients are listed in the flowchart below (Figure 4). The subjects completed the exercises in two groups of 16 people, and the variables were evaluated again.
Table 1 summarizes the mean and standard deviation of individual characteristics such as age, weight, height, body mass index, a score of pain, functional disability, and range of motion following conventional exercises.
Study flowchart

| Variables | Control Group (N = 16) | Intervention Group (N = 16) | P-Value |
|---|---|---|---|
| Age (years) | 41.69 ± 7.57 | 42.88 ± 7.96 | 0.66 |
| Height (cm) | 177.25 ± 4.71 | 179.55 ± 4.28 | 0.12 |
| Weight (kg) | 81.25 ± 6.06 | 80.44 ± 6.16 | 0.71 |
| BMI (kg/m2) | 25.87 ± 0.38 | 25.15 ± 1.02 | 0.83 |
| VAS score | 4.37 ± 1.02 | 4.25 ± 1.06 | 0.73 |
| Oswestry disability index score | 20.12 ± 5.67 | 17.62 ± 5.72 | 0.22 |
| Modified-Modified Schober flexion test | 10.12 ± 4.06 | 4.18 ± 0.75 | 0.62 |
| Modified-Modified Schober extension test | 1.68 ± 0.47 | 1.62 ± 0.50 | 0.72 |
The mean scores of pain severity, functional disability, and range of motion were significantly improved following conventional exercises (P < 0.001). Three people, due to not being willing to participate, and one person, due to worsening pain, were excluded from the study (Table 2).
Mean and Standard Deviation of Pain, Functional Disability, and Range of Motion
Before the motor control intervention, patients were matched for pain, functional disability, and range of motion, and there was no significant difference in the variables between the two groups (P > 0.05). After the intervention, The ANCOVA Within-group assessments showed a significant improvement in the mean scores of pain, functional disability, and range of motion following retraining motor control exercises (P < 0.001); however, no significant improvements were reported in the control group. In addition, The ANCOVA between-group assessments showed a significant improvement in the mean scores of pain and range of motion with a medium effect size and in functional disability with a large effect size after selected retraining motor control exercises (P < 0.001). In the intervention group, two people due to loss to follow-up and discontinued intervention, and in the control group, two people due to loss to follow-up and exercises other than stretching were excluded from the study (Table 3).
Mean and Standard Deviation of Pain, Functional Disability, and Range of Motion
| Variables | Control Group (N = 16), 95% CI | MCRT Group (N = 16), 95% CI | Between P | Effect Size | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | MIC | Within P | Pre | Post | MIC | Within P | |||
| VAS score | 4.37 (1.02), 3 - 6 | 4.31 (1.35), 3 - 6 | 1% ↓ | 0.751 | 4.25 (1.06), 3-6 | 1.50 (1.21), 0-4 | 64% ↓ | 0.000 ¥ | 0.000 a | 0.770 |
| Oswestry disability | 20.12 (5.67), 8 - 27 | 19.06 (4.91), 10 - 26 | 5% ↓ | 0.252 | 17.62 (5.72), 8-26 | 5.4 (2.82), 1-11 | 69% ↓ | 0.000 ¥ | 0.000 a | 0.804 |
| Flexion test | 4.06 (10.12), 3 - 5 | 4.25 (11.16), 2 - 5 | 4% ↑ | 0.188 | 4.18 (0.75), 3-5 | 5.56 (0.62), 4-6 | 33% ↑ | 0.000 ¥ | 0.000 a | 0.708 |
| Extension test | 1.68 (0.47), 1 - 2 | 1.78 (0.34), 1 - 2 | 5% ↑ | 0.178 | 1.62 (0.50), 1-2 | 2.75 (0.44), 2-3 | 69% ↑ | 0.000 ¥ | 0.000 a | 0.768 |
5. Discussion
To the best of our knowledge, this is the first study assessing the persistence and improvement of symptoms following retraining motor control exercises in patients with lumbar radiculopathy. According to the findings of the present study, conventional exercises improve pain, functional disability, and range of motion in male military personnel with chronic low back pain due to lumbar disc herniation, which is in line with the results of Mohebbi Rad's study (2022) on the effect of core exercises on pain and range of motion in discopathy patients using McGill and modified Shoober's test (38). Kahnzadeh et al. (2020) evaluated the effect of conventional core exercises on pain in office personnel with discopathy and reported an improvement in VAS, which agrees with our study (32). Other similar studies by Gaowgzeh et al. (2020) and Ramos et al. (2018) reported the positive effect of core exercises on the management of lumbar disc prolapse using the VAS, Numeric Rating Scale (NRS), and Modified Oswestry Questionnaire (MOQ) (33, 39). The effect of 15 combined sessions of electrotherapy, deep friction massage, and core exercises was evaluated by Demirel et al., who reported a significant improvement in patients with lumbar discopathy using the VAS and MOQ (40). Also, Ganio et al. (2015) reported that combining acupuncture, core exercises, and 12 minutes of treadmill walking improved pain and range of motion in patients with discopathy undergoing surgery (41). On the other hand, Kuligowski et al. showed that core exercises decreased the range of motion in patients with discopathy. They concluded that this reduction in range of motion might be due to differences in the severity of discopathy and the type and duration of exercise (42).
Factors such as weak body position, inappropriate chair, and long-time sitting result in inflammation and atrophy of core muscles (rectus abdominalis, transverse abdominalis, internal and external obliques, diaphragm, and pelvic floor), as well as disc herniation (7). Muscle atrophy and increased pressure change discs' metabolic structure, reducing heights (8). These muscles guide the different movement patterns of joints, so their injury leads to alteration in joint function and, finally, pain or functional disabilities. Electrical stimulation and core exercises involve the spasmatic and inactive muscles more actively (43). This method increases the power and coordination of muscles and consequently decreases low back pain (44). Pain and dysfunction of spinal vertebrates and discs may decrease the range of motion (45). In addition, movement in patients with chronic LBP is believed to result in muscle spasms and decreased flexibility in the musculoskeletal system. So, these patients avoid movements to prevent pain, leading to a reduced range of motion (46).
Also, muscle imbalance changes the pelvic tilt and reduces the range of motion of spinal vertebrae flexion (47). Based on the studies of electrical stimulation and core exercises, it improves musculoskeletal system function and, as a result, improves muscle balance, functional strength, and optimal movement of the lumbopelvic joints (43, 48). Although the evidence regarding the efficacy of TENS is controversial, researchers have recently recognized that various factors may influence the clinical use of TENS, including parameter planning, tolerance to repeated application, stimulation intensity, electrode placement, population and outcome assessed, outcome measurement time, and adverse interactions with opioid use (49, 50). Various theories have been proposed to explain the action mechanism of TENS. Among them, the most popular theory is gate control (50).
Various interventions have been suggested for retraining movement patterns. The common feature of these interventions is using retraining exercises and strategies for modifying vertebral alignment (35, 51), movement patterns (19, 35, 51), and activating deep and superficial muscles (21, 52, 53). According to Shumway-Cook and Woollacott (2011), motor control is a method in which the Central Nervous System (CNS) organizes muscles in coordinated movements, sensory information is used for choosing and controlling movements, and movement patterns are affected by perceptions. In addition, there is no consensus on the superiority of each exercise (54). However, in a recently published study on the efficacy of motor control exercises, the authors concluded that specific or segmental exercises might be superior to other therapies (20).
Several clinical trials have compared the efficacy of various motor control exercises in patients with disc herniation; however, no studies have assessed the effect of retraining exercises on disc herniation, especially in military personnel. In addition, none of the previous studies have assessed the effects of rehabilitation programs, especially motor control retraining exercises following conventional therapies, on the improvement and persistence of symptoms in patients with disc herniation.
Based on the present study's findings, selected motor control retraining exercises following conventional treatments led to continuous improvement of pain intensity in the intervention group (18, 34), and (55). The study of Plaza-Manzano et al. aimed to investigate the effect of eight weeks of motor control exercises on the pain of patients with disc herniation and radicular pain using the Numeric Pain Rating Scale (NPRS) showed a significant improvement in pain intensity after motor control exercises (55). In another similar study, Franca et al. evaluated the efficacy of an eight-week motor control exercise program in patients with radicular discopathy using the VAS and McGill pain questionnaire (18). They reported a significant improvement in pain relief, pain quality, and pain sensational quality. Aasa et al. showed the benefits of eight-week motor control exercises and educational interventions for improving low back pain using the VAS, which is compatible with the present study (34). In a review study, Alvani et al. investigated the effect of neuromuscular exercises on pain intensity in military personnel with chronic back pain and showed a significant decrease in the average pain score after the intervention (56). Also, Suni et al. evaluated neuromuscular and therapeutic recommendations for reducing absenteeism among young soldiers with chronic low back pain. The authors demonstrated the preventive role of these interventions in managing chronic low back pain in military settings (57).
Low back pain is a common problem among military personnel due to previous excessive activities or prolonged stable body positions at work (58, 59). Biofeedback and electromyographical assessments have shown that control of deep (e.g., transverse abdominalis and multifidus) and superficial muscles of the trunk, which are responsible for stability, is altered in patients with low back pain (24). Motor control exercises benefit from learning basics for retraining trunk muscle control, body positions, and movement patterns, leading to pain reduction (21). The aim is the proper activation of pelvic floor muscles, correct performance of exercises, and appropriate motor control of the pelvis during functional activities (36), which supports our protocol. In this study, we concluded that conventional exercise improves pain intensity. However, this improvement may take longer without retraining and controlling hip movements during daily activities. In our study, some patients in the control group had more severe pain two months after the last conventional exercise session. It was also possible to find a significant change in pain intensity if the follow-up period was longer. Previous research has reported that conventional methods such as electrotherapy or core exercises do not improve musculoskeletal structures because they are not considered active learning mechanisms (18, 60). In the process of motor learning, the nervous system automatically performs coordinated body movements, leading to functional improvement and pain reduction (61, 62). Also, during the present study, the subjects focused on controlling the body position and muscle activation during movements and controlling and modifying the activities provoking their pain. In their first meeting with the researcher and the physical therapist, they were asked to perform the activities they were doing with pain. The movement strategy was modified to correct the spinal alignment or suboptimal movement pattern, and the subjects were taught how to activate and feel the coordination of muscles during movements without pain. This feedback is probably one of the most important factors for reducing pain.
The present study showed that selected motor control retraining exercises following conventional therapies significantly improved functional disability in military personnel with radicular discopathy. These findings are consistent with the research results of Plaza-Manzano et al. (55) and Franca et al. (18). Also, Alvani et al. showed a significant improvement in the functional disability of military personnel with chronic back pain following neuromuscular exercises (56). Musculoskeletal injuries are a significant cause of disability among military personnel (63). About 20% of military personnel's musculoskeletal disorders are related to past events (64). There is a controversy about the mechanism of disability; however, the findings suggest a close relationship between perception and disability (65). Studies have shown that pain in patients with chronic back pain changes movement control and fear of pain recurrence and increases disability and movement limitation, psychological limitations, and other aspects of life (66, 67). Changes in motor behavior are usually observed in patients with low back pain as a compatibility mechanism to minimize pain's actual or precepted danger. In fact, these patients use motor control for pain control. Motor training in this study uses retraining and enhancement learning for further compatibilities, which may lead to rearrangement of the cerebral cortex and sensory inputs and control of lumbar movement and function (22, 68).
In the present study, patients' flexion and extension range of motion improved following selected motor control retraining exercises. Thus, we may conclude that motor control retraining exercises increase the range of motion in male military personnel with herniated disc-related chronic low back pain. We found no similar studies with the same conclusion; however, the possible effect of pain training on function improvement was seen in the present study. Patients probably learned that the pain during and after exercises was not a sign of inactivation, so they continued their movements, improving their functional disability (69). In addition, more ideal movement patterns 19 and increased resistance of trunk flexor and extensor muscles can decrease the stress and pressure of the lumbar soft tissue and consequently lower their sensitivity, improving the function and range of motion (35). In motor control retraining exercises, the emphasis is on the joint and the direction where the movement is isometrically controlled (not where the movement is actively performed). For lumbar flexion training, the stabilizing muscles of the lumbar extensor are actively employed to isometrically control lumbar flexion during repetitions of the retraining exercise. A flexion movement at the hip joint or thoracic spine creates a flexion-loading challenge that the stabilizing back extensor muscles must work against. Also, in the lumbar extension, the stabilizing flexor muscles are activated. The present study emphasized training to activate these muscles in modifying movement patterns and exercises. During retraining movements, the deep and superficial stabilizing muscles are continuously activated to control the UCM. It has been shown that the movement control of inefficient muscle groups and the efficiency of the corrective movement pattern increase the range of motion more than the strengthening of the dominant muscles, which was emphasized in the present study by retraining movement control exercises (19).
5.1. Limitations
The present study has limitations, including a low sample size and geographical limitations. Also, according to special rules in the Iranian military organization, researchers could not measure factors in female patients. The other limitations were the lack of access to advanced laboratory equipment, time limitations, and insufficient financial support. Cultural limits of Iran and lack of access to military personnel due to the nature of their job and insufficient support may have affected the results of the present study. We had 205 patients with lumbar disc herniation attending our clinics, of whom only 20% were compatible with the condition of the study. Finally, these are short-term results, and future studies should be conducted with larger samples and longer follow-up durations to strengthen the clinical implications.
5.2. Conclusions
The present study's findings suggest that selected motor control retraining exercises following conventional therapies can probably have positive effects on the persistence of pain, functional disability, and range of motion improvements. Preventive actions should focus on decreasing lumbar injuries in military personnel to reduce the burden of musculoskeletal disorders in this population. According to the positive and remarkable effect of selected motor control retraining exercises in this study, their low cost, and the feasibility of being conducted at home and work, it can probably be concluded that they are ideal for military personnel. The present study used eight weeks of isometric control of movements, control of body posture, and precision in movements (proper orientation of the pelvis in the resting position and control of the optimal orientation during active movements of the femur). It also utilized visual and auditory feedback and touch with gentle repetition and manual therapy, massage, stretching of muscles and joint capsule, and light resistance exercises for the pelvic floor muscles, transversus abdominis, and multifidus muscles. Hence, we improved muscle recruitment and made proper pelvis kinematics, improving pain, function, and range of motion. But for a better conclusion, more research is needed in this field.
Acknowledgements
References
-
1.
Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581-5. [PubMed ID: 10470716]. https://doi.org/10.1016/S0140-6736(99)01312-4.
-
2.
Chou R. Low back pain (chronic). BMJ clinical evidence. 2010;2010.
-
3.
Aghilinejad M, Choobineh AR, Sadeghi Z, Nouri MK, Ahmadi AB. Prevalence of musculoskeletal disorders among Iranian steel workers. Iranian Red Crescent Medical Journal. 2012;14(4):198.
-
4.
Oha K, Viljasoo V, Merisalu E. Prevalence of musculoskeletal disorders, assessment of parameters of muscle tone and health status among office workers. Agron Res. 2010;8(1):192-200.
-
5.
Kanna RM, Shetty AP, Rajasekaran S. Patterns of lumbar disc degeneration are different in degenerative disc disease and disc prolapse magnetic resonance imaging analysis of 224 patients. Spine J. 2014;14(2):300-7. [PubMed ID: 24231779]. https://doi.org/10.1016/j.spinee.2013.10.042.
-
6.
Jegede KA, Ndu A, Grauer JN. Contemporary management of symptomatic lumbar disc herniations. Orthop Clin North Am. 2010;41(2):217-24. [PubMed ID: 20399360]. https://doi.org/10.1016/j.ocl.2010.01.003.
-
7.
Sms D, P D, R I. Effect of spinal mobilization with leg movement as an adjunct to neural mobilization and conventional therapy in patients with lumbar radiculopathy: Randomized controlled trial. Journal of Medical and Scientific Research. 2018;6(1):11-9. https://doi.org/10.17727/jmsr.2018/6-3.
-
8.
Embleton J, Lines L. Spinal decompression therapy: Vibroseis of the body. SEG Technical Program Expanded Abstracts 2018. 2018. p. 4787-91.
-
9.
Kocak FA, Tunc H, Tomruk Sutbeyaz S, Akkus S, Koseoglu BF, Yilmaz E. Comparison of the short-term effects of the conventional motorized traction with non-surgical spinal decompression performed with a DRX9000 device on pain, functionality, depression, and quality of life in patients with low back pain associated with lumbar disc herniation: A single-blind randomized-controlled trial. Turk J Phys Med Rehabil. 2018;64(1):17-27. [PubMed ID: 31453485]. [PubMed Central ID: PMC6709608]. https://doi.org/10.5606/tftrd.2017.154.
-
10.
Wegner I, Widyahening IS, van Tulder MW, Blomberg SE, de Vet HC, Bronfort G, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev. 2013;2013(8). CD003010. [PubMed ID: 23959683]. [PubMed Central ID: PMC6823219]. https://doi.org/10.1002/14651858.CD003010.pub5.
-
11.
Sorkin JD, Muller DC, Andres R. Longitudinal change in the heights of men and women: consequential effects on body mass index. Epidemiol Rev. 1999;21(2):247-60. [PubMed ID: 10682261]. https://doi.org/10.1093/oxfordjournals.epirev.a018000.
-
12.
Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med. 2006;7(2):143-50. [PubMed ID: 16634727]. https://doi.org/10.1111/j.1526-4637.2006.00112.x.
-
13.
van Tulder MW, Malmivaara A, Esmail R, Koes BW. Exercise therapy for low-back pain. Cochrane Database of Systematic Reviews. 2000. https://doi.org/10.1002/14651858.Cd000335.
-
14.
Cleland J, Schulte C, Durall C. The role of therapeutic exercise in treating instability-related lumbar spine pain: A systematic review. J Back Musculoskelet Rehabil. 2002;16(2):105-15. [PubMed ID: 22387407]. https://doi.org/10.3233/bmr-2002-162-309.
-
15.
Kolar K. Lumbar-Disk Herniations: Conservative Clinical Applications. Athletic Therapy Today. 2005;10(5):26-30. https://doi.org/10.1123/att.10.5.26.
-
16.
Barone Gibbs B, Hergenroeder AL, Perdomo SJ, Kowalsky RJ, Delitto A, Jakicic JM. Reducing sedentary behaviour to decrease chronic low back pain: the stand back randomised trial. Occup Environ Med. 2018;75(5):321-7. [PubMed ID: 29330230]. [PubMed Central ID: PMC8283944]. https://doi.org/10.1136/oemed-2017-104732.
-
17.
Benoist M. The natural history of lumbar disc herniation and radiculopathy. Joint Bone Spine. 2002;69(2):155-60. [PubMed ID: 12027305]. https://doi.org/10.1016/s1297-319x(02)00385-8.
-
18.
Franca FJR, Callegari B, Ramos LAV, Burke TN, Magalhaes MO, Comachio J, et al. Motor Control Training Compared With Transcutaneous Electrical Nerve Stimulation in Patients With Disc Herniation With Associated Radiculopathy: A Randomized Controlled Trial. Am J Phys Med Rehabil. 2019;98(3):207-14. [PubMed ID: 30247159]. https://doi.org/10.1097/PHM.0000000000001048.
-
19.
Comerford M,, Mottram S. Kinetic Control. The. Management of. Uncontrolled Movement. Elsevier Australia; 2012. p. 63-216.
-
20.
Bystrom MG, Rasmussen-Barr E, Grooten WJ. Motor control exercises reduces pain and disability in chronic and recurrent low back pain: a meta-analysis. Spine (Phila Pa 1976). 2013;38(6):E350-8. [PubMed ID: 23492976]. https://doi.org/10.1097/BRS.0b013e31828435fb.
-
21.
Macedo LG, Latimer J, Maher CG, Hodges PW, McAuley JH, Nicholas MK, et al. Effect of motor control exercises versus graded activity in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther. 2012;92(3):363-77. [PubMed ID: 22135712]. https://doi.org/10.2522/ptj.20110290.
-
22.
Searle A, Spink M, Ho A, Chuter V. Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials. Clin Rehabil. 2015;29(12):1155-67. [PubMed ID: 25681408]. https://doi.org/10.1177/0269215515570379.
-
23.
Wang XQ, Zheng JJ, Yu ZW, Bi X, Lou SJ, Liu J, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS One. 2012;7(12). e52082. [PubMed ID: 23284879]. [PubMed Central ID: PMC3524111]. https://doi.org/10.1371/journal.pone.0052082.
-
24.
Hodges PCJ, van DJ. Spinal control: The rehabilitation of back pain: State of the art and science. 1 ed. London, United Kingdom: Churchill Livingstone; 2013. p. 41-123.
-
25.
Franca FR, Burke TN, Caffaro RR, Ramos LA, Marques AP. Effects of muscular stretching and segmental stabilization on functional disability and pain in patients with chronic low back pain: a randomized, controlled trial. J Manipulative Physiol Ther. 2012;35(4):279-85. [PubMed ID: 22632587]. https://doi.org/10.1016/j.jmpt.2012.04.012.
-
26.
Hides JA, Jull GA, Richardson CA. Long-term effects of specific stabilizing exercises for first-episode low back pain. Spine (Phila Pa 1976). 2001;26(11):E243-8. [PubMed ID: 11389408]. https://doi.org/10.1097/00007632-200106010-00004.
-
27.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-91. [PubMed ID: 17695343]. https://doi.org/10.3758/bf03193146.
-
28.
Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. International Journal of Rehabilitation Research. 2008;31(2):165-9. https://doi.org/10.1097/MRR.0b013e3282fc0f93.
-
29.
Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the Iranian versions. Spine (Phila Pa 1976). 2006;31(14):E454-9. [PubMed ID: 16778675]. https://doi.org/10.1097/01.brs.0000222141.61424.f7.
-
30.
Williams R, Binkley J, Bloch R, Goldsmith CH, Minuk T. Reliability of the Modified-Modified Schöber and Double Inclinometer Methods for Measuring Lumbar Flexion and Extension. Physical Therapy. 1993;73(1):26-37. https://doi.org/10.1093/ptj/73.1.26.
-
31.
Tousignant M, Poulin L, Marchand S, Viau A, Place C. The Modified-Modified Schober Test for range of motion assessment of lumbar flexion in patients with low back pain: a study of criterion validity, intra- and inter-rater reliability and minimum metrically detectable change. Disabil Rehabil. 2005;27(10):553-9. [PubMed ID: 16019864]. https://doi.org/10.1080/09638280400018411.
-
32.
Khanzadeh R, Mahdavinejad R, Borhani A. The effect of suspension and conventional core stability exercises on characteristics of intervertebral disc and chronic pain in office staff due to lumbar herniated disc. Archives of Bone and Joint Surgery. 2020;8(3):445.
-
33.
Ramos LAV, Callegari B, Franca FJR, Magalhaes MO, Burke TN, Carvalho EA, et al. Comparison Between Transcutaneous Electrical Nerve Stimulation and Stabilization Exercises in Fatigue and Transversus Abdominis Activation in Patients With Lumbar Disk Herniation: A Randomized Study. J Manipulative Physiol Ther. 2018;41(4):323-31. [PubMed ID: 29751850]. https://doi.org/10.1016/j.jmpt.2017.10.010.
-
34.
Aasa B, Berglund L, Michaelson P, Aasa U. Individualized low-load motor control exercises and education versus a high-load lifting exercise and education to improve activity, pain intensity, and physical performance in patients with low back pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2015;45(2):77-85. B1-4. [PubMed ID: 25641309]. https://doi.org/10.2519/jospt.2015.5021.
-
35.
Sahrmann SH, St L, MO M. Diagnosis and Treatment of Movement Impairment Syndromes. 1 ed. Iran: Medicine Health Sciences; 2002. p. 51-190.
-
36.
Richardson C, Hodges P, Hides J. Therapeutic exercise for lumbopelvic stabilization. 2004. Elsevier; 2004.
-
37.
Cohen J. Statistical power analysis for the behavioral sciences. Academic press; 2013.
-
38.
Mohebbi Rad Y, Fadaei Chafy MR, Elmieh A. Is the novel suspension exercises superior to core stability exercises on some EMG coordinates, pain and range of motion of patients with disk herniation? Sport Sci Health. 2022;18(2):567-77. [PubMed ID: 34691266]. [PubMed Central ID: PMC8527285]. https://doi.org/10.1007/s11332-021-00848-2.
-
39.
Gaowgzeh RAM, Chevidikunnan MF, BinMulayh EA, Khan F. Effect of spinal decompression therapy and core stabilization exercises in management of lumbar disc prolapse: A single blind randomized controlled trial. J Back Musculoskelet Rehabil. 2020;33(2):225-31. [PubMed ID: 31282394]. https://doi.org/10.3233/BMR-171099.
-
40.
Demirel A, Yorubulut M, Ergun N. Regression of lumbar disc herniation by physiotherapy. Does non-surgical spinal decompression therapy make a difference? Double-blind randomized controlled trial. J Back Musculoskelet Rehabil. 2017;30(5):1015-22. [PubMed ID: 28505956]. https://doi.org/10.3233/BMR-169581.
-
41.
Ganiyu SO, Gujba KF. Effects of acupuncture, core-stability exercises, and treadmill walking exercises in treating a patient with postsurgical lumbar disc herniation: a clinical case report. J Acupunct Meridian Stud. 2015;8(1):48-52. [PubMed ID: 25660445]. https://doi.org/10.1016/j.jams.2014.08.002.
-
42.
Kuligowski T, Cieslik B, Kuciel N, Debiec-Bak A, Skrzek A. Effect of Core Stabilizing Training on Young Individuals Presenting Different Stages of Degenerative Disc Disease-Preliminary Report. Int J Environ Res Public Health. 2021;18(7). [PubMed ID: 33800555]. [PubMed Central ID: PMC8036822]. https://doi.org/10.3390/ijerph18073499.
-
43.
Wirth K, Hartmann H, Mickel C, Szilvas E, Keiner M, Sander A. Core Stability in Athletes: A Critical Analysis of Current Guidelines. Sports Med. 2017;47(3):401-14. [PubMed ID: 27475953]. https://doi.org/10.1007/s40279-016-0597-7.
-
44.
Letafatkar A, Nazarzadeh M, Hadadnezhad M, Farivar N. The efficacy of a HUBER exercise system mediated sensorimotor training protocol on proprioceptive system, lumbar movement control and quality of life in patients with chronic non-specific low back pain. J Back Musculoskelet Rehabil. 2017;30(4):767-78. [PubMed ID: 28453452]. https://doi.org/10.3233/BMR-150404.
-
45.
Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379(9814):482-91. [PubMed ID: 21982256]. https://doi.org/10.1016/S0140-6736(11)60610-7.
-
46.
Van Dieen JH, Selen LP, Cholewicki J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyogr Kinesiol. 2003;13(4):333-51. [PubMed ID: 12832164]. https://doi.org/10.1016/s1050-6411(03)00041-5.
-
47.
Retailleau M, Colloud F. New insights into lumbar flexion tests based on inverse and direct kinematic musculoskeletal modeling. J Biomech. 2020;105:109782. [PubMed ID: 32423539]. https://doi.org/10.1016/j.jbiomech.2020.109782.
-
48.
Bhadauria EA, Gurudut P. Comparative effectiveness of lumbar stabilization, dynamic strengthening, and Pilates on chronic low back pain: randomized clinical trial. J Exerc Rehabil. 2017;13(4):477-85. [PubMed ID: 29114516]. [PubMed Central ID: PMC5667628]. https://doi.org/10.12965/jer.1734972.486.
-
49.
Vance CG, Dailey DL, Rakel BA, Sluka KA. Using TENS for pain control: the state of the evidence. Pain Manag. 2014;4(3):197-209. [PubMed ID: 24953072]. [PubMed Central ID: PMC4186747]. https://doi.org/10.2217/pmt.14.13.
-
50.
Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971-9. [PubMed ID: 5320816]. https://doi.org/10.1126/science.150.3699.971.
-
51.
O'Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10(4):242-55. [PubMed ID: 16154380]. https://doi.org/10.1016/j.math.2005.07.001.
-
52.
Comerford MJ, Mottram SL. Functional stability re-training: principles and strategies for managing mechanical dysfunction. Man Ther. 2001;6(1):3-14. [PubMed ID: 11243904]. https://doi.org/10.1054/math.2000.0389.
-
53.
Costa LO, Maher CG, Latimer J, Hodges PW, Herbert RD, Refshauge KM, et al. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther. 2009;89(12):1275-86. [PubMed ID: 19892856]. https://doi.org/10.2522/ptj.20090218.
-
54.
Shumway-Cook A, Woollacott MH. Motor control: translating research into clinical practice. Lippincott Williams & Wilkins; 2007.
-
55.
Plaza-Manzano G, Cancela-Cilleruelo I, Fernandez-de-Las-Penas C, Cleland JA, Arias-Buria JL, Thoomes-de-Graaf M, et al. Effects of Adding a Neurodynamic Mobilization to Motor Control Training in Patients With Lumbar Radiculopathy Due to Disc Herniation: A Randomized Clinical Trial. Am J Phys Med Rehabil. 2020;99(2):124-32. [PubMed ID: 31464753]. https://doi.org/10.1097/PHM.0000000000001295.
-
56.
Alvani E, Shirvani H, Shamsoddini A. Neuromuscular exercises on pain intensity, functional disability, proprioception, and balance of military personnel with chronic low back pain. The Journal of the Canadian Chiropractic Association. 2021;65(2):193.
-
57.
Suni JH, Taanila H, Mattila VM, Ohrankammen O, Vuorinen P, Pihlajamaki H, et al. Neuromuscular exercise and counseling decrease absenteeism due to low back pain in young conscripts: a randomized, population-based primary prevention study. Spine (Phila Pa 1976). 2013;38(5):375-84. [PubMed ID: 22941095]. https://doi.org/10.1097/BRS.0b013e318270a12d.
-
58.
Cohen SP, Gallagher RM, Davis SA, Griffith SR, Carragee EJ. Spine-area pain in military personnel: a review of epidemiology, etiology, diagnosis, and treatment. Spine J. 2012;12(9):833-42. [PubMed ID: 22100208]. https://doi.org/10.1016/j.spinee.2011.10.010.
-
59.
To D, Rezai M, Murnaghan K, Cancelliere C. Risk factors for low back pain in active military personnel: a systematic review. Chiropr Man Therap. 2021;29(1):52. [PubMed ID: 34969400]. [PubMed Central ID: PMC8719410]. https://doi.org/10.1186/s12998-021-00409-x.
-
60.
Gottlieb GL, Corcos DM, Jaric S, Agarwal GC. Practice improves even the simplest movements. Exp Brain Res. 1988;73(2):436-40. [PubMed ID: 3215317]. https://doi.org/10.1007/BF00248235.
-
61.
Unlu Z, Tasci S, Tarhan S, Pabuscu Y, Islak S. Comparison of 3 physical therapy modalities for acute pain in lumbar disc herniation measured by clinical evaluation and magnetic resonance imaging. J Manipulative Physiol Ther. 2008;31(3):191-8. [PubMed ID: 18394495]. https://doi.org/10.1016/j.jmpt.2008.02.001.
-
62.
Patla AE, Ishac MG, Winter DA. Anticipatory control of center of mass and joint stability during voluntary arm movement from a standing posture: interplay between active and passive control. Exp Brain Res. 2002;143(3):318-27. [PubMed ID: 11889509]. https://doi.org/10.1007/s00221-001-0968-6.
-
63.
Rhon DI, Teyhen DS, Shaffer SW, Goffar SL, Kiesel K, Plisky PP. Developing predictive models for return to work using the Military Power, Performance and Prevention (MP3) musculoskeletal injury risk algorithm: a study protocol for an injury risk assessment programme. Inj Prev. 2018;24(1):81-8. [PubMed ID: 27884941]. [PubMed Central ID: PMC5800339]. https://doi.org/10.1136/injuryprev-2016-042234.
-
64.
Vining R, Minkalis A, Long CR, Corber L, Franklin C, Gudavalli MR, et al. Assessment of chiropractic care on strength, balance, and endurance in active-duty U.S. military personnel with low back pain: a protocol for a randomized controlled trial. Trials. 2018;19(1):671. [PubMed ID: 30518400]. [PubMed Central ID: PMC6280458]. https://doi.org/10.1186/s13063-018-3041-5.
-
65.
Swinkels IC, van den Ende CH, van den Bosch W, Dekker J, Wimmers RH. Physiotherapy management of low back pain: does practice match the Dutch guidelines? Aust J Physiother. 2005;51(1):35-41. [PubMed ID: 15748123]. https://doi.org/10.1016/s0004-9514(05)70051-9.
-
66.
Yang Q, Wang Z, Yang L, Xu Y, Chen LM. Cortical thickness and functional connectivity abnormality in chronic headache and low back pain patients. Hum Brain Mapp. 2017;38(4):1815-32. [PubMed ID: 28052444]. [PubMed Central ID: PMC6867133]. https://doi.org/10.1002/hbm.23484.
-
67.
Lehtola V, Luomajoki H, Leinonen V, Gibbons S, Airaksinen O. Efficacy of movement control exercises versus general exercises on recurrent sub-acute nonspecific low back pain in a sub-group of patients with movement control dysfunction. Protocol of a randomized controlled trial. BMC Musculoskelet Disord. 2012;13:55. [PubMed ID: 22494776]. [PubMed Central ID: PMC3353835]. https://doi.org/10.1186/1471-2474-13-55.
-
68.
Richardson CA, Jull GA. Muscle control-pain control. What exercises would you prescribe? Man Ther. 1995;1(1):2-10. [PubMed ID: 11327788]. https://doi.org/10.1054/math.1995.0243.
-
69.
Moseley GL. Evidence for a direct relationship between cognitive and physical change during an education intervention in people with chronic low back pain. Eur J Pain. 2004;8(1):39-45. [PubMed ID: 14690673]. https://doi.org/10.1016/S1090-3801(03)00063-6.