Abstract
Background:
By providing sports organizations with electronic records and instruments that can be accessed at any time or place, specialized care can be offered to athletes regardless of injury location, and this makes the follow-up from first aid through to full recovery more efficient.Objectives:
The aim of this study was to develop an electronic personal health record for professional Iranian athletes.Patients and Methods:
First, a comparative study was carried out on the types of professional athletes’existing handheld and electronic health information management systems currently being used in Iran and leading countries in the field of sports medicine including; Australia, Canada and the United States. Then a checklist was developed containing a minimum dataset of professional athletes’ personal health records and distributed to the people involved, who consisted of 50 specialists in sports medicine and health information management, using the Delphi method. Through the use of data obtained from this survey, a basic paper model of professional athletes' personal health record was constructed and then an electronic model was created accordingly.Results:
Access to information in the electronic record was through a web-based, portal system. The capabilities of this system included: access to information at any time and location, increased interaction between the medical team, comprehensive reporting and effective management of injuries, flexibility and interaction with financial, radiology and laboratory information systems.Conclusions:
It is suggested that a framework should be created to promote athletes’ medical knowledge and provide the education necessary to manage their information. This would lead to improved data quality and ultimately promote the health of community athletes.Keywords
Personal Electronic Health Records Sports Medicine Software Design
1. Background
Nowadays, modern documentation of sports medicine activities can face serious challenges. The first is the multiplicity and diversity of sports medicine providers, such as; sports medicine specialists, team physicians, tournament doctors, orthopedic surgeons, physical therapists, medical assistants, athletic trainers, and others who are involved in the care of the athlete. The other challenge is that many athletes are not treated in a physician’s office or hospital because diagnosis and treatment often occurs at the place of injury, which in many cases frequently occurs at the gym or on the sport field (1). For these reasons, the discipline of sports medicine could benefit from information technologies more than other specialties (2).
The evolution of technological advances has led to the availability of electronic health records for every athlete at the place of care (3). By providing physicians and sport organizations with electronic records and instruments at any time or location, high quality care could be offered to athletes regardless of the injury location and the process can be followed from first aid through to full recovery (4). Electronic storage of athletes’ health data can lead to improved organization and application of this data and that has many potential benefits such as scientific research, statistical records regarding diagnostic and therapeutic procedures, reporting and saving time and expense (5, 6).
An athlete’s personal health record (PHR) can contain their health status from novice to professional elite athlete level. In addition, the millions of amateur athletes who do not continue to play professional sports can also use the system. These athletes could be equipped with a comprehensive and portable summary of their health status that enables them to understand, communicate and receive the best treatment for chronic and long-term injuries during their sport careers (7-9). The key point of the PHR is that the athlete will be able to play a more active role as the owner of the record and as a result they would remain the center of attention (10, 11). According to a report in the American Journal of Adults Health Care, an athlete’s PHR contains information about the athlete's abilities and a health status assessment of musculoskeletal and cardio-pulmonary systems. In addition, it also includes a summary of their past medical history, allergies, medical conditions which required immediate treatment, and a history of hospitalizations (8).
In modern medicine, a large amount of data is produced, but there is always a gap between data gathering and understanding and interpreting the data. Moreover, the available data are usually bulky and confusing. For this reason, a minimum data set is collected which provides a standard method to collect key data elements and this facilitates understanding and comparison of the material. In addition, this meets state requirements and the needs of individual institutions along with the medical community (12, 13). Multiple studies have proposed minimum demographic data sets for athletes’ paper and electronic personal health records (including name, address, phone number, date of birth, blood group, people who should be contacted in case of emergency, etc.), physician’s name, type of sport, date, type and place of injuries, diagnoses, and treatments (4, 7, 8).
2. Objectives
Due to the lack of a comprehensive and complete heath record for Iranian athletes in either paper or electronic formats, athletic clinical and administrative forms are used only sporadically, so researchers decided to design an electronic personal health record according to authorities in sports medicine which is able to organize, store and retrieve related information, promote the participation of team members in treatment and improve their interactions with each other and with the athletes. Moreover, this system is expected to increase athletes’ perception of their health levels through recording, viewing and editing information that enhances the quality of information and ultimately promotes the health of the community’s athletes.
3. Patients and Methods
First, a comparative study was conducted regarding the health records of athletes (manual and electronic formats) in leading countries in the sports medicine field, including; Australia, Canada and the United States, through the countries’ official sports medicine websites. At the national level, we visited the Sports Medicine Federation of the Islamic Republic of Iran and reviewed the clinical forms used by this organization and collected the relevant data. After comparing the content of records in the above-mentioned countries and obtaining a minimum data set for athletes’ personal health records, a checklist was developed containing four sources of information, i.e. demographics, health history, assessment and treatment plan. This checklist was first reviewed and modified by a four-member team, including; a sports medicine specialist, a health information management specialist, a medical informatics specialist and an expert in health information technology, and its content validity was confirmed by the team.
Then, using the Delphi method, the checklist was distributed among the available participants who consisted of 50 specialists in sports medicine, health information management and medical informatics. They were asked to rate their agreement with the inclusion of each element in the final record on a five-item Likert scale and they commented at the end of the checklist in response to an open question, if applicable. Among the 50 distributed checklists, 45 were returned. Responders included 22 sports medicine specialists, 12 health information management specialists, and 11 medical informatics specialists. After the survey, a re-evaluation was carried out on the different elements by the team and decisions were made on the proposed items. Final elements were introduced as the minimum data set required for an Iranian athletic personal health record, subsequently, the researchers designed a prototype of the athletes’ personal health record in a paper format and then the electronic model was developed.
4. Results
Data elements collected from the survey that was considered to be the minimum dataset necessary for a professional athlete’s personal health record are specified in Table 1. The electronic personal health record designed for professional Iranian athletes is a web-based, object oriented and modular system, written with PHP programming language and a SQLite database management system.
Minimum Dataset of Iranian Professional Athletes’ Personal Health Record
| Data Element | Details |
|---|---|
| Demographics | Personal (name, date of birth, gender, address, phone number), Insurance (insurance type, number, expiry date, institute), athletic (type of sport, federation name, club, team) |
| Health history | Drug allergies, drugs currently used, past medical history, family history, history of surgery |
| General examinations | Chief complaint, present illness, review of important body systems |
| Injury report | Location, nature, severity, cause, activity at time of injury, diagnostic code, protective equipment, initial treatment, medical advices, referral state |
| Laboratory tests | Test name, result, advice |
| Medications | Drug name, type, prescription cause, start and stop dates of usage, duration of usage, side effects and drug-drug or drug-food interference |
| Surgeries | Surgeon’s diagnosis, surgery type, description |
| Physiotherapy | Physiotherapist’s diagnosis, procedures, modalities |
| Nutrition | Age, BMI, history of eating disorders, dietary history, food allergies, type of nutritional disorder, diet chart, advices |
| Dentistry | Type of lesion, location, procedure name |
| Immunization | Vaccine’s name, injection time |
4.1. Users
Users of the system include; athletes, team physicians, physiotherapists, athletic trainers, sport support personnel (psychologist, massage therapist, dietitian, orthopedic surgeon, cardiologist, etc.) and an expert in information management who plays the role of system administrator. These users are allowed to record or edit certain information according to the access level assigned to them (role-based access). The system manager is responsible for supervising all operations carried out and he/she has access to all parts of the system. To access the data, users log into the record through a portal. Athletes may use the portal for safe messaging to their medical team, filling the required checklists or questionnaires, request, re-schedule or cancel appointments, view online medical expenses and quick payment, and view their clinical information. Health care providers can also use the portal to send reminders for appointments, to provide new registration forms for athletes, to report laboratory findings, to perform electronic visits, and to send attachments (document or image).
4.2. Modules
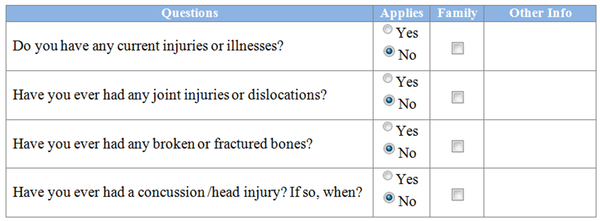
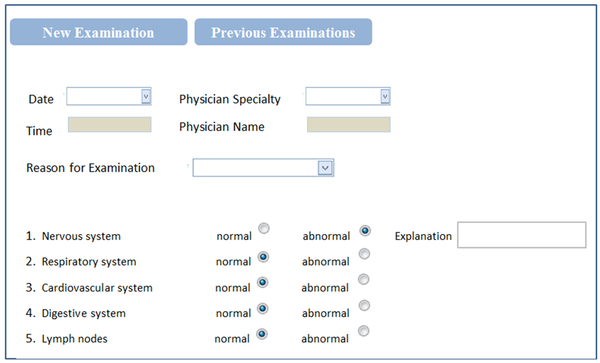
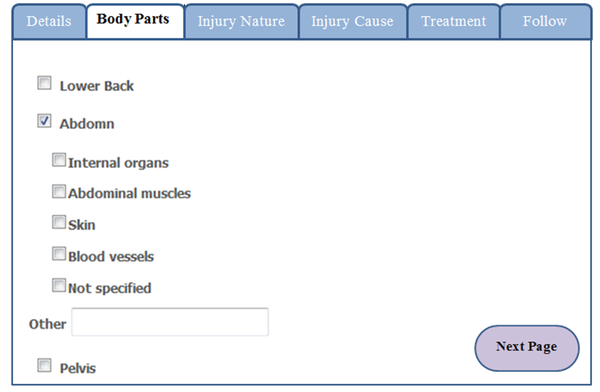
The system is comprised of modules that can be customized to the specific needs of each sports medicine organization. These modules include; athlete administration, health history, general physical examinations, injury reports, surgery, physiotherapy, immunizations, nutrition, drugs, dentistry, sports injury psychology and other procedures. Each module consists of two parts, "new record" and "previous case management". The athlete’s medical history (Figure 1) and physical examination (Figure 2) must be maintained and updated in every season of competition. Injury information can also be organized according to the nature, place, time and cause of injury (Figure 3). If physical therapy is required, it includes a module to record the type and duration of each physical therapy session. Information from multiple modules can be linked together; therefore, all providers have access to the most up-to-date information.
In the injury report module, the latest version of the Orchard Sport Injury Classification System (OSICS-10) was used to determine a diagnostic code for the injury and the latest version of Standard Nomenclature of Athletic Injuries (SNAI) was used to select a standard name along with the explanations about the nature of the injury. Use of these systems is considered to be an advantage of the designed EPHR. The OSICS is one of the most common systems used to code injury diagnoses in sports injury surveillance systems, and it was used for the first time in Australia. Widespread use, having specific codes for sports medicine, and free usage, are among the advantages of the OSICS (14). The American Medical Association established a list of standard names related to degrees and types of athletic injuries in 1964. In addition, the terms contain sufficient information to facilitate the possibility of statistical reporting and to determine causes and prevention measures of sports injuries. The second edition was published in 1976 and as yet no program has been considered for re-editing (15, 16).
Another strength of the system is the psychology injury questionnaire. The reason for the inclusion of this section in the record is that when an athlete is recruited to a club or team, data from this questionnaire may give useful information about the athlete’s mental health to medical team professionals, especially psychologists who may facilitate psychological support of the athlete. This section includes 15 questions and the athlete can choose multiple answers for each question. Questions were determined in consultation with a specialist in sports psychology, and by referring to relevant books and articles.
The "other procedures" module adds information related to other measures, such as; laboratory findings, x-ray, echocardiogram, etc. and the ability to attach multimedia files. Due to the variety of laboratory findings and several items in each para-clinical report, they have been included collectively in a separate item titled “other procedures” but the user can only view the attached images of these reports. In future editions, it is expected to be more interactive, so full access to the data may be possible via a network incorporating all laboratory and imaging reports.
Part of Health History Module
Part of General Physical Examinations
Injury Report Module
5. Discussion
Access to information through the internet has become very important in sports centers because athletes are often injured on the sport field and treated at the same place. Web based applications can give staff immediate access and review of medical information at any given location (17, 18). Many EHR systems are not appropriate for the athletes’ care providers because of the nature of the collaborative care received by athletes, which is very different from the care provided in hospitals and medical facilities (19). In a sports organization, there are coaches, assistant coaches, dietitians, physiotherapists, and team physicians that each play a role in the care process, but they require different tools and access levels. In addition, an athlete’s electronic health record focuses on both medical signs and symptoms as well as factors that influence the injury, such as; playing surface, weather conditions, equipment used by athletes, previous history of similar injuries, and other players involved in the injury process, so that sports officials can use the data to analyze trends and adjust strategies in order to prevent injuries from occurring (20, 21).
The design of the electronic record has the benefit of allowing access to information at any time or place in order to obtain accurate data, to make informed and timely decisions, to integrate data in a central and safe database, to facilitate communication and promote the participation of a medical team in treatment, to create complete reports from each module, to improve athletes' health knowledge through observation and review of their health information, to effectively manage injuries and accelerate the athlete’s return to play, it is also capable of displaying information in Persian and English, maintain flexibility and interaction with financial, radiology, laboratory information systems, and so on.
An electronic personal health record for professional Iranian athletes is a comprehensive, secure and role-based instrument which ensures that only authorized individuals can gain access to confidential medical data according to their qualifications and rights. Secure role-based access maintains the confidentiality of patient information and corresponds to standard medical privacy rules. The system can track the health of the athletes during their sport’s career and merge all related data that will be used and shared by medical staff, managers and researchers, across sport organizations and league competitions. This in turn provides the possibility of risk management, ensures the safety and competitive status of the athletes, allows customization of physical conditioning plans, and supports the aims of athlete, as well as league and sports organizations. The comprehensive electronic system includes work flows that are dedicated to instances such as clinical injury treatment, injury occurrence analysis, acceptance of the athlete by the club, insurance management, and following instructions and the use of clinical instruments.
Professional Iranian athletes’ electronic personal health record is web-based and it provides access to information at any time or place. It contains data elements that are introduced as the minimum data set of the Iranian athlete’s personal health record. The system has the potential to record, store and retrieve a large volume of personal, sport and health information in a central database. In our country a platform should be provided to promote athletes’ medical knowledge and create necessary training for them to learn this information management tool as this would allow the athlete to import necessary information into their record. This would lead to improved information quality and ultimately promote the health of the community’s athletes.
Acknowledgements
References
-
1.
Streator S, Buckley WE. Featured Article Clinical Outcomes in Sports Medicine. Int J Athlet Ther Train. 2000;5(5):57-61.
-
2.
Smith. Telehealth in sport medicine. 2011. Available from: http://www.mobile-telehealth.com/telehealth-in-sports-medicine.
-
3.
Anonymous. Henry Ford Health System; Electronic medical record technology aids marathon participants. Atlanta, NewsRx; 2010.
-
4.
Wells GL, 3rd, Higgins G3, Baumann MR. Implementing an electronic point-of-care medical record at an organized athletic event: challenges, pitfalls, and lessons learned. Clin J Sport Med. 2010;20(5):377-8. [PubMed ID: 20818197]. https://doi.org/10.1097/JSM.0b013e3181efada5.
-
5.
Janas MR. Making the case for sports medicine informatics. Alabama: United States Sport Academy; 2011.
-
6.
Deligiannis P, Deligiannis AS, Kouidi E. Trends in e-Health Monitoring Implementation in Sports. Sport med Präventivmed. 2011;41(2):34-7. https://doi.org/10.1007/s12534-011-0172-9.
-
7.
Campbell S. Introducing the Personal Health Record for Athletes. 2011. Available from: http://www.cerner.com/blog/introducing_the_personal_health_record_for_athletes/?langType=1033.
-
8.
Allen J. Personal health record for athletes. 2011. Available from: http://www.livestrong.com/article/341551-personal-health-record-for-athletes.
-
9.
Successful Launch of the Special Olympics Personal Health Record Pilot Program. 2010. Available from: http://healthoneglobalcomau.melbourneitwebsites.com/article/health-record-pilot-program.
-
10.
Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13(2):121-6. [PubMed ID: 16357345]. https://doi.org/10.1197/jamia.M2025.
-
11.
Eveillard P. [The electronic personal health record: the spirit of the law of March 4, 2002]. Rev Prat. 2004;54(17):1861-4. [PubMed ID: 15655907].
-
12.
Arfa I, Abid A, Malouche D, Ben Alaya N, Azegue TR, Mannai I, et al. Familial aggregation and excess maternal transmission of type 2 diabetes in Tunisia. Postgrad Med J. 2007;83(979):348-51. [PubMed ID: 17488867]. https://doi.org/10.1136/pgmj.2006.053744.
-
13.
Johns ML. Health information management technology: An applied approach. Chicago, IL: American Health Information Management Association; 2002.
-
14.
Orchard J, Rae K, Brooks J, Hagglund M, Til L, Wales D, et al. Revision, uptake and coding issues related to the open access Orchard Sports Injury Classification System (OSICS) versions 8, 9 and 10.1. Open Access J Sports Med. 2010;1:207-14. [PubMed ID: 24198559]. https://doi.org/10.2147/OAJSM.S7715.
-
15.
Safdari R. Disease nomenclature and classification systems and provide a model for the national classification of diseases. Tehran: Mirmah; 2003.
-
16.
Rachun A. Standard nomenclature of athletic injuries. American Medical Association; 1976.
-
17.
Glickman D. Choosing the Right Athlete Electronic Health Record System. 2012. Available from: http://www.presagia.com/2857.
-
18.
Shared online medical records for elite athletes. 2012. Available from: http://www.voluntis.com/en/see-our-solutions-at-work/215-shared-online-medical-records-for-elite-athletes.html.
-
19.
Johnson TC. Electronic health record implementation for an NCAA baseball team. The College of St. Scholastica; 2012.
-
20.
Howard RL, editor. The NCAA Injury Surveillance System- A Functional Tool for Athletic Trainers. NATA Annual Meeting and Clinical Symposium Anaheim. 2007; California.
-
21.
Dick RW. NCAA Injury Surveillance System: A Tool for Health and Safety Risk Management. Athletic Therapy Today. 2006;11(1):42-4.