Abstract
Background:
Racquet sports, especially lawn tennis and badminton have been gaining popularity in Asian countries like India. With this increase in popularity, the injury rate in the sport has also increased.Objectives:
The study will help detect the presence of gleno-humeral movement dysfunction and scapular resting position abnormality in asymptomatic racquet players, thus providing basis for screening the players and allow the clinician to determine if the asymmetry is a normal adaptation in the player or an abnormal change associated with injury.Materials and Methods:
46 asymptomatic professional players were divided into a study group of 23 players (16 tennis and 7 badminton) and control group of 23 football players. Assessment of passive gleno-humeral range of motion and distance of spine and inferior angle of scapula from corresponding spinous process were measured bilaterally and between groups.Results:
There was statistically significant reduction in range of internal rotation (62.17 ± 8.09), extension (39.78 ± 4.12) and an increase in the external rotation (106.95 ± 7.49) of dominant compared to non-dominant arm of racquet players and a statistically significant decrease in internal rotation (78.69 ± 10.24), extension (44.78 ± 3.19), adduction (37.39 ± 6.54) and an increase in external rotation (102.6 ± 5.19) of dominant arm of racquet players compared to football players. Study also showed statistically significant increase in the spino-scapular distance at the level of inferior angle of scapula (10.23 ± 1.43) on dominant side compared to non-dominant.Conclusions:
The dominant side scapula of asymptomatic racquet players showed increased external rotation and elevation as compared to the non-dominant side. Also, reduced shoulder internal rotation, extension and adduction and gain in shoulder external rotation was observed on the dominant side of racquet players when compared to the control group.Keywords
1. Background
Racquet sports, especially lawn tennis and badminton have been gaining popularity in Asian countries like India. With this increase in popularity, the injury rate in the sport has also increased. The injury rate in tennis varies from 0.04 injuries/1000 hours to 21.5 injuries/1000 hours (1). Different overhead sports show different characteristics, but have similar movement patterns. In each, the dominant upper limb is subjected to repeated overhead movements (2, 3). The mechanics of an overhead stroke or serve in racquet sports are similar to that of an overhead throw (4), wherein the shoulder has to be lax enough to allow the extra degrees of external rotation necessary for an adequate serve and at the same time has to be stable enough to prevent any subluxations. This delicate balance between mobility and stability is referred to as ‘throwers paradox’ (3) and if compromised, can lead to injury (5). A racquet serve/stroke is a combination of true gleno-humeral rotation, trunk hyperextension and scapulo-thoracic motion. The cocking phase maintains the dominant arm in 90° abduction and external rotation which reaches a maximum of 172° to 180° during the late cocking phase (6-8). It ends with internal rotation and forward flexion of the dominant shoulder along with upper torso and pelvic rotation during the follow through phase. Each phase places an asymmetric load between the two shoulders, with the dominant shoulder exposed to maximum stress (9). Studies have shown a significant difference in the gleno-humeral internal rotation range of motion between dominant and non-dominant shoulders of overhead sport players (2, 3, 10-14). This is defined as ‘Gleno-humeral internal rotation deficit’ (GIRD), which is the loss in degrees of the gleno-humeral internal rotation of the throwing shoulder compared with the non-throwing shoulder (15). An accepted level of GIRD is less than 20° deficit of gleno-humeral internal rotation or less than 10% deficit of the total rotation seen in throwing shoulder as compared to the non-throwing shoulder (15). The scapula provides a stable base to the movement of humeral head during an overhead motion. The stability of the scapula becomes important in these movement patterns (9). An asymmetry develops in the scapular posture of overhead athletes like tennis players, where the dominant scapula is more protracted than the non-dominant side (16). The acronym SICK scapula (scapular malposition, inferior medial border prominence, coracoid pain and malposition and dyskinesis) is used to describe this asymmetry of scapula (17). This asymmetry is accentuated in unilateral overhead athletes who use their dominant shoulder repetitively in a forceful manner (16). Many authors suggest that this increased scapular protraction along with GIRD, increases the likelihood of shoulder injuries in these players (18-20). Shoulder girdle injuries account for 17.27% in racquet players with 43.4% of elite tennis players presenting with scapular dyskinesia (21, 22). Most of the studies on overhead sports have been conducted on baseball players with very limited studies on asymptomatic racquet players. With the increasing popularity of racquet sports and an increase in its injury rate, it is essential to determine the predisposing risk factors in these overhead sports. Not much attention is paid to evaluation of movement dysfunction during periodic evaluation and screening of elite players. Thus, a meticulous examination of the shoulder girdle in asymptomatic players will prevent them from becoming symptomatic in the near future.
2. Objectives
With the aim of studying the presence of scapular resting position abnormality and gleno-humeral movement dysfunction in asymptomatic racquet players, the objectives of the study were to compare the scapular resting position and gleno-humeral range of motion between the dominant and non-dominant shoulder of the asymptomatic racquet players and to compare the scapular resting position and gleno-humeral range of motion of the dominant shoulder between the asymptomatic racquet players and non-racquet players.
3. Materials and Methods
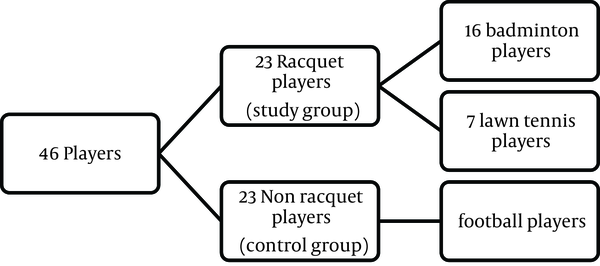
A case-control, observational, single-blind study was designed and approved from Institutional Ethics Committee. Asymptomatic volunteers in the age group of 15 - 25 years, playing badminton, lawn tennis or football regularly for more than 1 year at professional competitive level were recruited by a process of simple randomization. Players with history of shoulder pain or injury, neck pain, surgery or deformity near shoulder complex were excluded. A sample of 46 players was included in the study (Figures 1 and 2).
Demographic Data
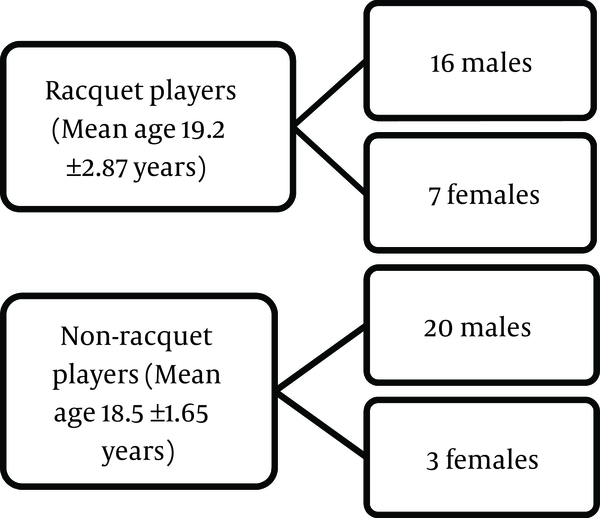
Division of Groups
The purpose of the study was explained to the coach and the players and written informed consent was obtained prior to testing. Subjects were given a questionnaire to obtain demographic data and rule out exclusion criteria. The assessment included:
1) Spino-scapular distance: (a) at the spine of the scapula bilaterally; (b) at the inferior angle of the scapula bilaterally.
2) Level of the Scapula: (a) at the spine of the scapula bilaterally; (b) at the inferior angle of the scapula bilaterally.
Scapular assessment (23-25): Was performed by one assessor (author 2), wherein, the subjects were made to stand with the back facing the assessor. The spine of the scapula was palpated from the acromion process and the medial end of the spine of the scapula was marked with a marker. The inferior angle was palpated and marked with a marker. The spinous processes of the vertebral column were palpated starting from C7 to T10. The subject was asked to flex his/her neck to find the prominent C7 spinous process and then with deep postero-anterior pressure the remaining thoracic spinous processes were palpated and marked with the marker. The levels of the spine of the scapula and the inferior angle were noted and then the spino-scapular distance at the spine of the scapula and at the inferior angle was measured using a measuring tape.
3) Shoulder range of motion (ROM) assessment (15, 26): Bilateral gleno-humeral range of motion was measured passively with standard goniometer by the same assessor (author 2) (Table 1). Data decoding and chart preparation was done by another assessor (authors 1 and 3 respectively). Statistical analysis was done by SPSS version 12.0. Comparison of the dominant and non-dominant side of the racquet players was done using 2-tailed, dependent-sample paired t test. Comparison of the dominant side of racquet and non-racquet players was done by unpaired t test. Alpha level of P ≤ 0.05 was set.
Assessment of ROM
| Shoulder ROM | Patient Position | Fulcrum | Starting Position of the Limb |
|---|---|---|---|
| Flexion | Supine | Greater tuberosity | Arm by the side of the body |
| Abduction | Supine | Coracoid process | Arm by the side of the body |
| Adduction | Supine | Coracoid process | Arm by the side of the body |
| External rotation | Supine | Olecranon process | Shoulder in 90° abduction and elbow in 90° flexion |
| Internal rotation | Supine | Olecranon process | Shoulder in 90° abduction and elbow in 90° flexion |
| Extension | Prone | Greater tuberosity | Arm by the side of the body |
4. Results
Results from statistical analysis are included in Tables 2 - 5.
Comparison of Scapular Resting Position in Racquet Players Between Dominant and Non-dominant Sides a
| Spino-Scapular Distance, cm | Groups | ||
|---|---|---|---|
| Dominant Side | Non-Dominant Side | P Value | |
| At level of spine of scapula | 8.52 ± 1.38 | 8.34 ± 1.43 | > 0.05 |
| At level of inferior angle of scapula | 10.23 ± 1.43 | 9.86 ± 1.40 | < 0.05 |
Comparison of Scapular Resting Position in Dominant Shoulder Between Racquet and Non-Racquet Players a
| Spino-Scapular Distance, cm | Groups | ||
|---|---|---|---|
| Racquet Players | Non Racquet Players | P Value | |
| At level of spine of scapula | 8.52 ± 1.38 | 8.15 ± 0.88 | > 0.05 |
| At level of inferior angle of scapula | 10.23 ± 1.43 | 9.91 ± 0.68 | > 0.05 |
Comparison of ROM in Racquet Players Between Dominant and Non-Dominant Sides a
| ROM, Degrees | Groups | ||
|---|---|---|---|
| Dominant Side | Non-Dominant Side | P Value | |
| Flexion | 180 | 180 | > 0.05 |
| Extension | 39.78 ± 4.12 | 41.3 ± 4.05 | < 0.05 |
| Abduction | 180 | 180 | > 0.05 |
| Adduction | 29.78 ± 1.83 | 30 | > 0.05 |
| Internal rotation | 62.17 ± 8.09 | 76.39 ± 7.16 | < 0.05 |
| External rotation | 106.95 ± 7.49 | 99.78 ± 5.93 | < 0.05 |
Comparison of ROM in Dominant Shoulder Between Racquet and Non-Racquet Players a
| ROM, Degrees | Groups | ||
|---|---|---|---|
| Racquet Players | Non-Racquet Players | P Value | |
| Flexion | 180 | 180 | > 0.05 |
| Extension | 39.78 ± 4.12 | 44.78 ± 3.19 | < 0.05 |
| Abduction | 180 | 180 | > 0.05 |
| Adduction | 29.78 ± 1.83 | 37.39 ± 6.54 | < 0.05 |
| Internal rotation | 62.17 ± 8.09 | 78.69 ± 10.24 | < 0.05 |
| External rotation | 106.95 ± 7.49 | 102.6 ± 5.19 | < 0.05 |
5. Discussion
Many studies have reported similar findings in overhead sport players (6, 16-20). Studies have also shown a positive association between a dyskinetic scapula with posterior shoulder tightness and GIRD in the dominant arm of overhead players (17-19, 27, 28). During the follow through phase, the scapula has to protract around the thoracic wall in order to help dissipate the energy (18, 19, 25, 29). In the presence of considerable GIRD, the players have to bring about increased scapular protraction to compensate for the reduced internal rotation in order to maintain the velocity of the overhead stroke (18, 19). With time, this continuous stress causes soft tissue adaptations and leads to weakness of the scapular stabilizers, mainly the lower fibres of rhomboids causing an upward rotation (18, 19). Thus, the scapula cannot provide a stable base of support for the rotator cuff to function, which reduces its efficiency and increases stress on the static restraints of the dominant shoulder (19). So, rather than compressing the humeral head into the glenoid fossa, the rotator cuff pulls the scapula upward and laterally resulting in greater scapular protraction and external rotation (24). The present study suggests an upward rotation of the dominant scapula in racquet players (Tables 2 and 3). Results of the present study also show significant reduction in the internal rotation and extension ROM and a gain in the external rotation of the dominant shoulder compared to the non-dominant shoulder of racquet players (Table 4). Also, there was a significant reduction in internal rotation, extension and adduction and an increase in external rotation of the dominant shoulder of racquet players when compared to dominant shoulder of non-racquet players (Table 5). During the follow through phase of an overhead motion, the shoulder joint is subjected to distractive forces of up to 750N which is mainly resisted by the postero-inferior capsule (6, 15). With repetitive loading, the posterior capsule is said to undergo micro trauma causing hypertrophy and increased fibroblastic activity during the healing process, leading to contracture and thickening of the capsule (2, 18). This reduces the capsular pliability causing restriction of internal rotation, extension and horizontal adduction (2, 6, 18). Similar findings were obtained in the present study. Another study had shown GIRD to be a common finding in tennis players and swimmers, being more common in tennis players than swimmers because of the impact of the game (2). A posterior capsule stretching program incorporated in the rehabilitation and training of overhead players is reported to reduce the incidence of GIRD. It also reduces the incidence of shoulder injuries like Superior Labrum Anterior Posterior (SLAP) lesions in these players (15). Arthroscopic studies have also shown increased thickness and hypertrophy of capsule in the postero-inferior recess of dominant arm of throwers and its positive association with GIRD, external rotation and scapular upward rotation (15, 30). Studies have shown that for a 4° decrease in internal rotation, there is 1cm decrease in horizontal adduction, which is an indicator of posterior capsule tightness (2). This study also showed a significant increase in the external rotation of the dominant shoulder compared to non-dominant side in racquet players and when compared to dominant side of non-racquet players. One of the causes can be attributed to the contracted or shortened posterior band of the inferior gleno humeral ligament (IGHL) which primarily provides restraint to further movement in position of maximum abduction and external rotation during late cocking phase. It prevents posterior migration of humeral head, thus centering it in the glenoid fossa allowing a normal arc of movement (6, 15). Arthroscopic findings in overhead players show contractures and thickening in the zone of the posterior band of IGHL. The tethered posterior band draws the humeral head postero-superiorly to a new point of rotation on the glenoid, thus causing an abnormal increase in the external rotation due to easier clearance of the greater tuberosity (6, 15). The postero-superior migration of humeral head also reduces the cam effect of the humeral head and antero-inferior humeral calcar on the antero-inferior capsule leading to redundancy in the antero-inferior capsule, allowing hyper external rotation of the dominant arm (15). Another explanation for the increased external rotation can be possibly attributed to increased humeral retroversion which is a common finding in players playing overhead sports (31-33). Studies have shown an increase in humeral retroversion in the dominant arm of professional pitchers (12, 16, 34, 35). In young pre-adolescent overhead sports players, with long years of play, these adaptive changes occur as the proximal humeral epiphysis is not fused (31). This change in the humeral head causes a shift in the arc of rotation of the dominant shoulder favoring external rotation (31, 32, 36). However, the studies suggest that the total arc of rotation remains the same, as any increase in the external rotation will require a corresponding decrease in the internal rotation, which will be permanent (36). The capsule and ligamentous changes mentioned above superimpose on these osseous changes (31). Similar changes may have occurred even in the present studied population, thus affecting their ROM. In the present study, confounders were the technique of measuring the movements manually. The scapular position and gleno-humeral motions could have been measured using 3-Dimensional software equipment. But the present methods of assessment are universal methods which can be obtained with minimal resources and evaluations carried out in the fields rather than in laboratories. This makes the present study and methods of evaluations more clinically relevant. Also, as all participants in this study were asymptomatic, the presence of postural asymmetry may be normal in the population of unilateral overhead athletes and may not necessarily be related to presence of injury. Injured overhead athletes may display more asymmetry than healthy overhead athletes, and there may be a pathologic threshold for scapular posture asymmetry at which an asymmetry becomes problematic. A comparison between symptomatic and asymptomatic players could help determine this threshold. There is presence of abnormal scapular resting position in asymptomatic racquet players on the dominant side in the form of scapular external rotation and elevation on the dominant side as compared to their non-dominant side. There is also presence of gleno-humeral movement dysfunction in the form of reduced internal rotation, extension and adduction and gain in external rotation on the dominant side when compared to the control group. Thus, ROM and scapular resting position can be used as a screening tool for injury prevention in overhead racquet players. This study highlights the need of specific stretching and strengthening as a part of the pre-season training of racquet athletes to address muscular imbalances to provide optimum scapular and gleno-humeral stability to the shoulder to endure the demands of the game.
Acknowledgements
References
-
1.
Pluim BM, Staal JB, Windler GE, Jayanthi N. Tennis injuries: occurrence, aetiology, and prevention. Br J Sports Med. 2006;40(5):415-23. [PubMed ID: 16632572]. https://doi.org/10.1136/bjsm.2005.023184.
-
2.
Torres RR, Gomes JL. Measurement of glenohumeral internal rotation in asymptomatic tennis players and swimmers. Am J Sports Med. 2009;37(5):1017-23. [PubMed ID: 19261903]. https://doi.org/10.1177/0363546508329544.
-
3.
Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the over-head throwing athlete. Am J Sports Med. 2002;30:131-51.
-
4.
Craig A. The shoulder complex. In: Maria Z, Christopher B, John C, editors. Sports Physiotherapy: Applied Science and Practice. Churchill Livingstone; 1995.
-
5.
Downar JM, Sauers EL. Clinical Measures of Shoulder Mobility in the Professional Baseball Player. J Athl Train. 2005;40(1):23-9. [PubMed ID: 15902320].
-
6.
van der Hoeven H, Kibler WB. Shoulder injuries in tennis players. Br J Sports Med. 2006;40(5):435-40. discussion 440. [PubMed ID: 16632575]. https://doi.org/10.1136/bjsm.2005.023218.
-
7.
Fleisig GS, Barrentine SW, Escamilla RF, Andrews JR. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21(6):421-37. [PubMed ID: 8784962].
-
8.
Fleisig G, Nicholls R, Elliott B, Escamilla R. Kinematics used by world class tennis players to produce high-velocity serves. Sports Biomech. 2003;2(1):51-64. [PubMed ID: 14658245]. https://doi.org/10.1080/14763140308522807.
-
9.
Jason A. Biomechanics of common sporting injuries. In: Peter B, Karim K, editors. Clinical Sports Medicine. 3th ed. McGraw-Hill Professional; 2007. 68 p.
-
10.
Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25(5):609-13. [PubMed ID: 9302464].
-
11.
Borsa PA, Wilk KE, Jacobson JA, Scibek JS, Dover GC, Reinold MM, et al. Correlation of range of motion and glenohumeral translation in professional baseball pitchers. Am J Sports Med. 2005;33(9):1392-9. [PubMed ID: 16002489]. https://doi.org/10.1177/0363546504273490.
-
12.
Crockett HC, Gross LB, Wilk KE, Schwartz ML, Reed J, O'Mara J, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30(1):20-6. [PubMed ID: 11798991].
-
13.
Johnson L. Patterns of shoulder flexibility among college baseball players. J Athl Train. 1992;27(1):44-9. [PubMed ID: 16558130].
-
14.
Meister K. Injuries to the shoulder in the throwing athlete. Part one: Biomechanics/pathophysiology/classification of injury. Am J Sports Med. 2000;28(2):265-75. [PubMed ID: 10751008].
-
15.
Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404-20. [PubMed ID: 12671624]. https://doi.org/10.1053/jars.2003.50128.
-
16.
Oyama S, Myers JB, Wassinger CA, Daniel Ricci R, Lephart SM. Asymmetric resting scapular posture in healthy overhead athletes. J Athl Train. 2008;43(6):565-70. [PubMed ID: 19030133]. https://doi.org/10.4085/1062-6050-43.6.565.
-
17.
Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641-61. [PubMed ID: 12861203].
-
18.
Thomas SJ, Swanik KA, Swanik CB, Kelly JD. Internal rotation and scapular position differences: a comparison of collegiate and high school baseball players. J Athl Train. 2010;45(1):44-50. [PubMed ID: 20064047]. https://doi.org/10.4085/1062-6050-45.1.44.
-
19.
Thomas SJ, Swanik KA, Swanik CB, Kelly J. Internal rotation deficits affect scapular positioning in baseball players. Clin Orthop Relat Res. 2010;468(6):1551-7. [PubMed ID: 19841995]. https://doi.org/10.1007/s11999-009-1124-z.
-
20.
Wilk KE, Obma P, Simpson CD, Cain EL, Dugas JR, Andrews JR. Shoulder injuries in the overhead athlete. J Orthop Sports Phys Ther. 2009;39(2):38-54. [PubMed ID: 19194026]. https://doi.org/10.2519/jospt.2009.2929.
-
21.
Borsa PA, Laudner KG, Sauers EL. Mobility and stability adaptations in the shoulder of the overhead athlete: a theoretical and evidence-based perspective. Sports Med. 2008;38(1):17-36. [PubMed ID: 18081365].
-
22.
Kondric M, Matkovic BR, Furjan-Mandic G, Hadzic V, Dervisevic E. Injuries in racket sports among Slovenian players. Coll Antropol. 2011;35(2):413-7. [PubMed ID: 21755712].
-
23.
Odom CJ, Taylor AB, Hurd CE, Denegar CR. Measurement of scapular asymetry and assessment of shoulder dysfunction using the Lateral Scapular Slide Test: a reliability and validity study. Phys Ther. 2001;81(2):799-809. [PubMed ID: 11235656].
-
24.
Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325-37. [PubMed ID: 9548131].
-
25.
Kibler WB. Role of the scapula in overhead throwing motion. Contemp Orthop. 1991;22(5):525-32.
-
26.
Norkin CC, White DJ. The shoulder. In: Norkin CC, White DJ, editors. Measurement of Joint Motion: A Guide to Goniometry. 3th ed. Philadelphia: FA Davis Company; 2003. p. 83-9.
-
27.
Laudner KG, Moline MT, Meister K. The relationship between forward scapular posture and posterior shoulder tightness among baseball players. Am J Sports Med. 2010;38(10):2106-12. [PubMed ID: 20595550]. https://doi.org/10.1177/0363546510370291.
-
28.
McClure P, Greenberg E, Kareha S. Evaluation and management of scapular dysfunction. Sports Med Arthrosc. 2012;20(1):39-48. [PubMed ID: 22311292]. https://doi.org/10.1097/JSA.0b013e31824716a8.
-
29.
Voight ML, Thomson BC. The role of the scapula in the rehabilitation of shoulder injuries. J Athl Train. 2000;35(3):364-72. [PubMed ID: 16558649].
-
30.
Thomas SJ, Swanik CB, Higginson JS, Kaminski TW, Swanik KA, Bartolozzi AR, et al. A bilateral comparison of posterior capsule thickness and its correlation with glenohumeral range of motion and scapular upward rotation in collegiate baseball players. J Shoulder Elbow Surg. 2011;20(5):708-16. [PubMed ID: 21167742]. https://doi.org/10.1016/j.jse.2010.08.031.
-
31.
Kibler WB, Chandler TJ, Shapiro R, Conuel M. Muscle activation in coupled scapulohumeral motions in the high performance tennis serve. Br J Sports Med. 2007;41(11):745-9. [PubMed ID: 17957010]. https://doi.org/10.1136/bjsm.2007.037333.
-
32.
Tokish JM, Curtin MS, Kim YK, Hawkins RJ, Torry MR. Glenohumeral internal rotation deficit in the asymptomatic professional pitcher and its relationship to humeral retroversion. J Sports Sci Med. 2008;7(1):78-83. [PubMed ID: 24150137].
-
33.
Kibler WB, Sciascia A, Thomas SJ. Glenohumeral internal rotation deficit: pathogenesis and response to acute throwing. Sports Med Arthrosc. 2012;20(1):34-8. [PubMed ID: 22311291]. https://doi.org/10.1097/JSA.0b013e318244853e.
-
34.
Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30(3):347-53. [PubMed ID: 12016074].
-
35.
Reagan KM, Meister K, Horodyski MB, Werner DW, Carruthers C, Wilk K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. Am J Sports Med. 2002;30(3):354-60. [PubMed ID: 12016075].
-
36.
Lintner D, Mayol M, Uzodinma O, Jones R, Labossiere D. Glenohumeral internal rotation deficits in professional pitchers enrolled in an internal rotation stretching program. Am J Sports Med. 2007;35(4):617-21. [PubMed ID: 17293473]. https://doi.org/10.1177/0363546506296736.