Abstract
Background:
A clinical outcome tool is needed for the assessment of young athletes with low back pain.Objectives:
To translate and culturally adapt the Micheli functional scale (MFS), a self-report questionnaire developed to evaluate young athletes with low back pain (LBP) into Persian language and examine the reliability and validity of the Persian MFS (PMFS).Materials and Methods:
A cross-sectional study was conducted to assess the psychometric properties of the PMFS. The PMFS was cross-culturally adapted into Persian language adopting forward/backward translation, expert panel review, and pre-testing. The PMFS was administered to young athletes with and without LBP. Main outcome measures were Persian MFS, Persian functional rating Index (PFRI), and visual analogue scale (VAS).Results:
A sample of 100 young athletes with LBP with a mean age of 16.5 ± 2.5 years participated. Fifty young athletes without LBP completed the PMFS. There was no missing responses and floor or ceiling effects. There was a significant difference for the total PMFS scores between young athletes with and without LBP. A significant correlation was found between the total PMFS score and the VAS (r = 0.92) or the PFRI (r = 0.82; P < 0.001). A high internal consistency reliability (Cronbach α = 0.73), and excellent test-retest reliability (ICCagreement = 0.99, P < 0.001) were demonstrated for the PMFS. Factor analysis indicated a single-factor model for PMFS scores.Conclusions:
The Persian MFS is valid and reliable for use in Persian-speaking young athletes with LBP.Keywords
1. Background
Low back pain (LBP) is a common condition in children and adolescents which can have significant impact on their daily life (1). Various epidemiological studies have identified a high prevalence of back pain in adolescents with a lifetime prevalence of 70% - 80% by the age of 20 (2). Young athletes involved in contact or noncontact sports may complain from LBP (3). The LBP occurs in sports involving repetitive spinal movements, such as gymnastics, and soccer. Overuse injuries are a common cause of LBP, although acute trauma is also included (4). Increased specialization, high level of physical activity, and participation in year-round sports competitions are reasons for a high incidence of injury among young athletes (5).
It is recognized that the health professionals should consider the patient’s perspective about their condition and measure factors important for them alongside with clinical data. Self-reported outcome measures are used to provide the patient’s perspective on the treatment effectiveness. These measures are commonly used as an important source of data also for patients with LBP in practice and for research purposes. There are many back specific tools for assessing the functional status in patients with LBP addressing the patient’s perceptions of their backache (6). Recently, efforts have been made to develop a back-specific questionnaire for adult athletes with LBP (7). All these functional assessment tools, however, have not included sports related dysfunctions designed for young athletes. It is therefore essential to use back-specific measures for young athletes to accurately assess the sports related functioning and symptoms in clinical practice and to monitor whether patients benefit from treatments.
In 2012, the Micheli functional scale (MFS) was developed as a back-specific tool for functional assessment in young athletes (8). The MFS originally developed in English, assesses pain and functional levels in the young athlete, and can be self-administered in a quicker time. This scale is a brief and reliable rating scale to quantify pain intensity and athletic function, and determines the degree of the back pain associated with sports activity limitations, back extension/or upright activities, sitting/or flexion activities, and jumping activity (8).
The MFS is a self-report questionnaire and contains 5 items consisting of a symptom question (0 - 5 points), 3 activity-related questions (extension, 0 - 4; flexion, 0 - 3; jumping, 0 - 3), and a visual analogue scale (VAS) [0 (no pain) to 10 (most severe pain)] for pain intensity. The total score is calculated by adding questionnaire responses (range 0 - 15) plus VAS score (range 0 - 10). This maximum total score of 25 is then multiplied by 4. The range of total scores is from 0 (least amount of difficulty) to 100 (the most amount of difficulty) (8).
There is a need for clinical outcome assessment tools available in the Persian language to be used for the assessment of young athletes with back pain. The MFS has not been translated and culturally adapted into Persian language.
2. Objectives
Therefore, the purposes of this study were to translate and culturally adapt the MFS into Persian language, and to assess the discriminative validity, construct validity, concurrent criterion-related validity, internal consistency reliability, and test-retest reliability of the Persian MFS (PMFS) in young athletes with LBP.
3. Materials and Methods
3.1. Design
A cross-sectional study was conducted to assess the psychometric properties of the PMFS in young athletes with LBP. The Research Council, School of Rehabilitation, and Ethical Committee of Tehran University of Medical Sciences (TUMS) approved the study protocol.
3.2. Participants
The patients were included in the study from May to December 2013 in Tehran, Iran. Inclusion criteria were: 1) young athlete aged between 10 - 22 years old involved in sport activities for at least 3 times per week; 2) having LBP; and 3) able to read and write in Persian language. Exclusion criteria were: 1) history of spinal pathologies or surgery; 2) presence of lower limb injuries; 3) non consent.
According to the literature (9), at least 100 patients are needed for internal consistency and 50 patients for validity analyses. The written informed consent was obtained from subjects before participation.
3.3. Translation and Cross-Cultural Adaptation
The procedure suggested for translation and cross-cultural adaptation of self-report questionnaires was followed (10, 11). This consists of: 1) forward translation; 2) backward translation; and 3) expert’s committee review. The original English version of the MFS was forward translated by two independent translators. The two translations and the original English version of MFS were reviewed by 3 expert physiotherapists, a methodologist, and 2 translators until a Persian version of the MFS was produced. The back translation of the consensus version was carried out by two new translators that were teachers of English language from the English language unit of TUMS, and were blinded to the study. At this stage, the experts committee together with translators reviewed the original English MFS and the all translations and finalized the prefinal version of the PMFS. The prefinal version of the PMFS was then pilot tested for face and content validity with 30 normal young athletes with LBP who agreed to participate at this stage of the study to test whether the patients had difficulties in the understanding of questionnaire items. The participants reported that they could understand the prefinal version of the Persian MFS correctly, and consequently, the final PMFS was developed for further psychometric characterization testing.
3.4. Face and Content Validity
Face and content validity of the PMFS were assessed by adopting the standard procedure for cross-cultural validation of health status questionnaires enhanced by expert committee discussions, and field testing of the prefinal version which was shown to be acceptable (9-11). The content validity of the PMFS was examined by the presence of floor or ceiling effects as well (9).
3.5. Discriminative Validity
It was tested by comparing total PMFS scores between young athletes with and without LBP.
3.6. Construct Validity
The construct validity was examined by relating PMFS with Persian FRI. A priori hypothesis was a high correlation between the PMFS and the PFRI.
The FRI is a self-report questionnaire for assessing pain and function in patients with LBP from 0% (no disability) to 100% (severe disability) (12). It was used because it needs shorter duration to administer (78 seconds) and is reliable, valid, and responsive (13). The FRI has been validated in Persian language for spinal conditions of LBP (14) and neck pain (15). The relation between the PMFS and the Persian FRI (PFRI) was evaluated with Pearson’s correlation test. Moreover, the factor analysis was performed for evaluation of construct validity.
3.7. Concurrent Validity
For concurrent criterion-related validity, the relation between PMFS and visual analogue scale (VAS) was examined by Pearson’s correlation test.
3.8. Internal Consistency
It is a measure of the extent to which items in a questionnaire are correlated (inter-item correlation), and measuring the same concept. If internal consistency is relevant, a factor analysis should be applied to determine whether the items form one or more than one subscale (9).
3.9. Test-Retest Reliability
The PMFS questionnaire was completed 2 times for the test-retest reliability to test whether repeated measurements provide similar responses. The time interval between 2 measurements was 7 days.
3.10. Data Collection Procedure
The young athletes were recruited from sports clubs in Tehran, Iran. The young athletes with LBP completed the PMFS, the visual analogue scale (VAS), and the Persian questionnaire of functional rating scale (FRI). For test-retest reliability, the second PMFS was completed by 50 young athletes after 7 days. The normal individuals only completed the PMFS.
3.11. Statistical Analysis
The independent samples t-test or Chi-Square test was used to compare LBP and healthy groups for age, education, and gender. The measurement properties of PMFS were interpreted according to the quality criteria proposed by Terwee et al. (9). The floor and ceiling effects were calculated as percentage frequency of lowest or highest possible score achieved by individuals. The presence of floor and ceiling effects was set as > 15%. For discriminative validity, the differences between the young athletes with and without LBP were examined by the independent samples t-test. The construct validity of the PMFS was examined in relation to the Persian FRI using Pearson correlation coefficient test. The concurrent criterion validity of the PMFS was investigated by associating the PMFS to the VAS using Pearson correlation coefficient test where a minimum value of 0.70 is recommended acceptable. The internal consistency reliability was tested by Cronbach’s alpha. Values between 0.70 to 0.95 are proposed for good internal consistency when factor analysis is analyzed. The test-retest reliability of the PMFS was assessed by the intraclass correlation coefficient (agreement) (ICCagreement) (two-way random effects model, average measure). At least 0.70 is recommended for giving a positive rating for reliability. The principle component analysis (PCA) with varimax rotation was applied to examine the factor structure of the PMFS. Analyses were performed by using the SPSS for Windows, version 18, Chicago, Illinois, USA.
4. Results
4.1. Demographic and Clinical Characteristics
The PMFS was administered to 100 young athletes with LBP (male/female: 44/56; mean age = 16.5 ± 2.5 years, range = 11 - 22). The mean duration of LBP was 12.78 ± 12.04 months (range 1 - 60). Table 1 shows the descriptive data of the PMFS, the PFRI, and the VAS. There were no differences between young athletes with (n = 100) and without LBP (n = 50) for age (P = 0.45), education (P = 0.79), or gender (P = 0.87).
Demographic and Descriptive Data for the Persian Mitcheli Functional Scale (PMFS), Persian Functional Rating Index (PFRI), and the Visual Analogue Scale (VAS) (N = 100)
| Variables | Mean ± SD | Range (Min - Max) |
|---|---|---|
| Age, y | 16.5 ± 2.5 | 11 - 22 |
| Education, y | 10.11 ± 2.32 | 5 - 15 |
| PMFS | 38.97 ± 18.40 | 8.00 - 96.80 |
| PFRI | 32.90 ± 16.64 | 10.00 - 82.50 |
| VAS | 4.16 ± 2.42 | 0.50 - 10.00 |
The athletes in this sample (n = 150) were involved in the sports activities of physical fitness (n = 43, 28.7%), soccer (n = 37, 24.7%), volleyball (n = 20, 13.3%), judo (n = 14, 9.3%), basketball (n = 12, 8%), and others (n = 24, 16 %).
4.2. Acceptability
Translation of the questionnaire was presented without problems and the back translation was concurred with the original English MFS. The PMFS was well accepted by patients with no difficulties in understanding of the PMFS items. The patients responded to all items of the questionnaire without missing data, and commented the items of PMFS easy and relevant to their LBP.
4.3. Floor and Ceiling Effects
There were no missing values for each of PMFS item. The patient had not achieved a maximum or minimum score for the total PMFS [median, IQR (interquartile range)] = 40.00 (25.90 - 51.50). The floor and ceiling effects were not observed for the PMFS.
4.4. Discriminative Validity
The data from the 50 of 100 young athletes with LBP (mean age = 16.7 ± 2.4 years, range 12.00 - 22.00) who participated in the retest were analyzed for discriminative validity. There were no differences between 2 groups for age (P = 0.31), education (P = 0.62), or gender (P = 0.07). The PMFS scores were statistically higher for young athletes with LBP (40.85 ± 18.25, range 8.00 - 78.80) than those who had no LBP (2.64 ± 4.90, range 0.00 - 18.00) with a mean age = 16.2 ± 2.7 years (range 11.00 - 22.00) and a mean education = 10.00 ± 2.54 (range 5.00 - 16.00) (Levene’s test for equality of variances, F = 54.72, P < 0.001; t = −13.99; df = 56.03; P < 0.001).
4.5. Construct Validity
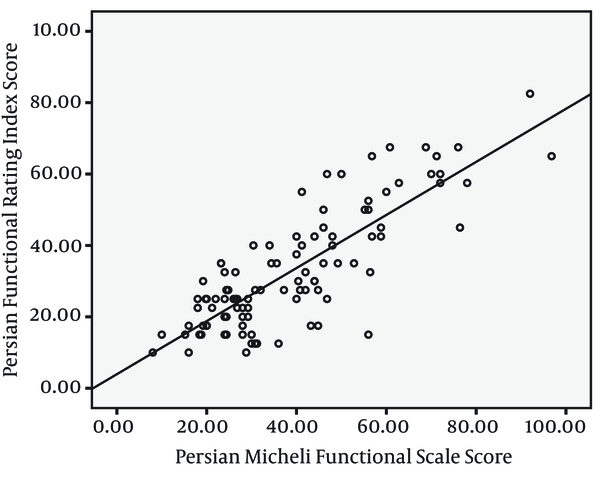
The Pearson correlation test revealed a significant correlation between the PMFS and PFRI for test (r = 0.82; P < 0.001) and retest (r = 0.86; P < 0.001). Figure 1 demonstrates the scatterplot of the PMFS and the PFRI.
Scatterplot Showing Significant Correlation Between the Persian Micheli Functional Scale (PMFS) and the Persian Functional Rating Index (PFRI), Pearson r = 0.82
4.6. Concurrent Criterion-Related Validity
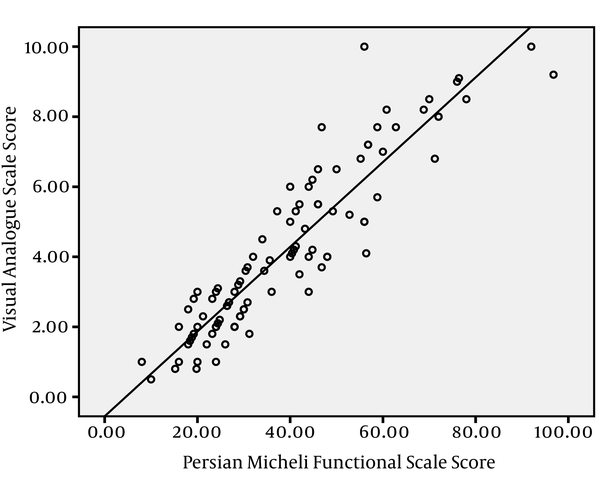
There were significant correlations between the PMFS and the VAS (r = 0.92 and 0.95 for test and retest, respectively, P < 0.001). Figure 2 shows the scatterplot of the PMFS and the VAS.
Scatterplot Showing Significant Correlation Between the Persian Micheli Functional Scale (PMFS) and the Visual Analogue Scale (VAS), Pearson r = 0.92
4.7. Internal Consistency
The internal consistency was good (Cronbach α = 0.73 for test and 0.75 for retest).
4.8. Test-Retest Reliability
The test-retest reliability was calculated using data from 50 young adolescents with LBP who participated at test and retest phase of the study. Excellent test-retest reliability for the total PMFS score was found (ICCagreement) = 0.99, P < 0.001.
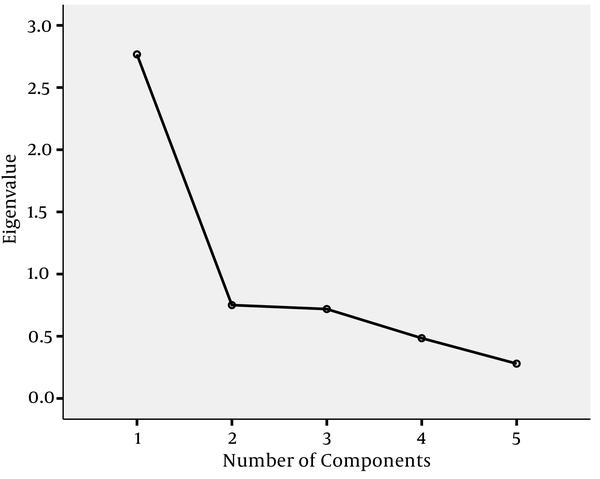
4.9. Factor Analysis
The factor analysis of PMFS extracted 1 factor with eigenvalue > 1, accounting for 55.34% of the total variance (the Kaiser-Meyer-Olkin (KMO) coefficient 0.77; Bartlett’s test 154.33, P < 0.001). Figure 3 shows only 1 eigenvalue before the scree plot levels out, indicative of 1-factor structure for PMFS.
Scree Plot of Persian Micheli Functional Scale
5. Discussion
This is the first study to translate and culturally adapt the MFS from English into Persian language, and evaluate the validity and reliability of the PMFS for Persian speaking young athletes. This study showed that the PMFS is a valid and reliable instrument for evaluating the pain and functional levels in the young athletes with LBP, with sound psychometric properties which corresponds to the original English MFS.
Many children and adolescents participate in sport and exercise activities. Training and high level of physical activities in different sports may cause various musculoskeletal conditions such as LBP in young athletes. There is a great need for valid and reliable tools to be used in the clinic and research to assess young athletes with LBP to provide the best and most accurate treatments. The MFS is a new, function specific instrument that evaluates the perspective of young athletes with LBP with regard to their pain, function, and disability related to sport activities (8). The PMFS validated in this study provides the Persian speaking clinicians and researchers with an instrument to assess the pain and functional status of young athletes with LBP in the context of their sport activities.
The PMFS did not show floor or ceiling effects for the total score as found for the original English MFS. However, the authors of the original MFS did not focus on the floor and ceiling effects, and the main aim was evaluating the MFS validity. In this study, compared to the original study, a larger sample of patients was enrolled (100 vs. 44). This indicates that the PMFS did not exhibit the floor or ceiling effects though there was more opportunity for occurrence. No floor and ceiling effects observed for the PMFS indicates the sensitivity of the PMFS to detect changes after treatment and the ability to distinguish different levels of LBP severity in young athletes with LBP. The PMFS acceptability together with no floor or ceiling effects point out to the content validity of the PMFS.
The PMFS total scores for young athletes with LBP were significantly higher than those of the young athletes without LBP. The values of PMFS indicated a greater pain intensity and higher disability in young athletes with LBP compared to those without LBP. Therefore, the PMFS differentiated young athletes with and without LBP supporting the excellent discriminative validity. This suggests that the PMFS is effective in identifying young athletes with LBP and sport dysfunctions. The discriminative validity of the PMFS provides evidence for this new tool in distinguishing young athletes with and without LBP confirming the previous work on the original MFS where good discriminative validity was concluded (8).
In the current study, construct validity was examined in terms of the correlation between the PMFS and the PFRI. A significant inter-correlation between the PMFS and the PFRI was revealed as hypothesized, which indicates that the PMFS has an excellent convergent validity. The construct validity demonstrated for PMFS is consistent with the original English MFS (8). A robust statistically significant correlation between the two self-report questionnaires indicates a full convergence between two measures of PMFS and PFRI, confirming that both instruments are related to a common construct.
Concurrent criterion-related validity assessed by correlation analysis between the PMFS and the VAS showed an excellent positive association between the two. There is no established gold standard for health status questionnaires available for comparison (16). In this study, the concurrent criterion-related validity of the PMFS was examined in relation to the VAS, which is a reliable and valid tool for pain assessment (17). In the study of English MFS, the concurrent criterion validity has not been investigated.
The internal consistency reliability estimates expressed as Cronbach’s Alpha coefficient for the PMFS was well above the acceptable level of 0.70, which indicates acceptable interitem reliability among PMFS items in agreement with the findings reported for the original English MFS (8). However, it appears that the Cronbach alpha value to be lower compared to the English MFS (α = 0.904). A possible explanation could be that the number of patients in the study for validation of the English MFS was small compared to the sample included in the present study. We adopted and followed the guideline presented for translating and validating health questionnaires. At least 100 individuals are needed for internal consistency reliability analysis (9). The internal consistency coefficient indicates that the PMFS is a homogenous instrument consisting of items that are related to a single domain when factor analysis confirms that the items appear only on one overall scale.
Test-retest reliability is an important measurement property for health status instruments indicating how scores using a tool are stable over time. The PMFS demonstrated excellent test-retest reliability. This indicates that when the PMFS is readministered some time later to the same young athletes with LBP while being in a clinically steady state, similar scores will be achieved. The test-retest reliability was not investigated for the English MFS (8). The excellent test-retest reliability of the PMFS is a measure for reproducibility of the PMFS, and signifies that the PMFS is stable for assessing young athletes with LBP.
The factor analysis of the PMFS yielded a 1 factor solution in agreement with the hypothesized construct related to sport activities. The factor analysis extracted 1 factor confirming the PMFS as a functional instrument with 1 dimension. The finding of 1 dimension also confirms the construct validity of the PMFS. The factor analysis was not performed in the case of original English MFS. The high internal consistency together with 1 factor solution found in the present study clearly demonstrates that the PMFS measures the same dimension.
In this study, we used the VAS as a gold standard for the evaluation of PMFS criterion validity. The VAS was also an item of PMFS. Further study is needed to clarify the criterion-related validity of the PMFS. Responsiveness of the PMFS to detect clinically important changes after intervention was not examined.
In conclusion, this is the first study to translate and adapt the MFS from English into another language. Therefore, the results of this investigation will be used as a reference for comparison in the future studies. The present study provides evidence regarding the validity and reliability of the PMFS, a newly developed measurement instrument for young athletes with LBP. The PMFS can be a useful tool for use in clinical and research settings in Persian speaking populations.
Acknowledgements
References
-
1.
Jones MA, Stratton G, Reilly T, Unnithan VB. A school-based survey of recurrent non-specific low-back pain prevalence and consequences in children. Health Educ Res. 2004;19(3):284-9. [PubMed ID: 15140848]. https://doi.org/10.1093/her/cyg025.
-
2.
Jones GT, Macfarlane GJ. Epidemiology of low back pain in children and adolescents. Arch Dis Child. 2005;90(3):312-6. [PubMed ID: 15723927]. https://doi.org/10.1136/adc.2004.056812.
-
3.
Trainor TJ, Trainor MA. Etiology of low back pain in athletes. Curr Sports Med Rep. 2004;3(1):41-6. [PubMed ID: 14728913].
-
4.
Purcell L, Micheli L. Low back pain in young athletes. Sports Health. 2009;1(3):212-22. [PubMed ID: 23015874]. https://doi.org/10.1177/1941738109334212.
-
5.
Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Mutanen PO, Karppinen JI. Musculoskeletal pains in relation to different sport and exercise activities in youth. Med Sci Sports Exerc. 2008;40(11):1890-900. [PubMed ID: 18845965]. https://doi.org/10.1249/MSS.0b013e31818047a2.
-
6.
Grotle M, Brox JI, Vollestad NK. Functional status and disability questionnaires: what do they assess? A systematic review of back-specific outcome questionnaires. Spine (Phila Pa 1976). 2005;30(1):130-40. [PubMed ID: 15626993].
-
7.
Zamani E, Kordi R, Nourian R, Noorian N, Memari AH, Shariati M. Low back pain functional disability in athletes; conceptualization and initial development of a questionnaire. Asian J Sports Med. 2014;5(4). eee24281. [PubMed ID: 25741417]. https://doi.org/10.5812/asjsm.24281.
-
8.
d'Hemecourt PA, Zurakowski D, d'Hemecourt CA, Curtis C, Ugrinow V, Deriu L, et al. Validation of a new instrument for evaluating low back pain in the young athlete. Clin J Sport Med. 2012;22(3):244-8. [PubMed ID: 22382433]. https://doi.org/10.1097/JSM.0b013e318249a3ce.
-
9.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34-42. [PubMed ID: 17161752]. https://doi.org/10.1016/j.jclinepi.2006.03.012.
-
10.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186-91. [PubMed ID: 11124735].
-
11.
Kristjansson EA, Desrochers A, Zumbo B. Translating and adapting measurement instruments for cross-linguistic and cross-cultural research: a guide for practitioners. Can J Nurs Res. 2003;35(2):127-42. [PubMed ID: 12908201].
-
12.
Feise RJ, Michael Menke J. Functional rating index: a new valid and reliable instrument to measure the magnitude of clinical change in spinal conditions. Spine (Phila Pa 1976). 2001;26(1):78-86. [PubMed ID: 11148650].
-
13.
Feise RJ, Menke JM. Functional Rating Index: literature review. Med Sci Monit. 2010;16(2):RA25-36. [PubMed ID: 20110929].
-
14.
Ansari NN, Feise RJ, Naghdi S, Ebadi S, Yoosefinejad AK. The functional rating index: reliability and validity of the Persian language version in patients with low back pain. Spine (Phila Pa 1976). 2011;36(24):E1573-7. [PubMed ID: 21270679]. https://doi.org/10.1097/BRS.0b013e3182103282.
-
15.
Ansari NN, Feise RJ, Naghdi S, Mohseni A, Rezazadeh M. The functional rating index: reliability and validity of the Persian language version in patients with neck pain. Spine (Phila Pa 1976). 2012;37(14):E844-8. [PubMed ID: 22310090]. https://doi.org/10.1097/BRS.0b013e31824b5bde.
-
16.
Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol. 2010;10:22. [PubMed ID: 20298572]. https://doi.org/10.1186/1471-2288-10-22.
-
17.
Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17-24. [PubMed ID: 18487245]. https://doi.org/10.1093/bja/aen103.