Abstract
Background:
Carotid Intima Media Thickness (IMT) is currently used to assess the relationship between progression of coronary and systemic atherosclerosis. To date, however, the possible impact of regular physical activity (PA) on this parameter has not been well estimated.Objectives:
Our study aims to examine this aspect especially in the absence of cardiovascular (CV) risk factors.Patients and Methods:
100 master athletes (MA) and 51 sedentary controls (SC) were enrolled. They were evaluated by echo test with dedicated software (QIMT-Esaote) for IMT, and Bruce protocol and 2D echocardiography for cardiac hemodynamic parameters.Results:
All values were within normal range. Left IMT mean values were significantly higher than right IMT values in both MA and SC groups (MA: IMT left 635 ± 104 µ, IMT right 614 ± 104 µ and mean IMT 624 ± 91.9 µ; SC: IMT left 633 ± 78 µ, IMT right 622 ± 90 µ and mean IMT 627 ± 78.1 µ). A positive relationship was found in both groups between IMT mean values and age (P < 0.01) and between IMT mean values and peak systolic blood pressure (MA: 0.28 R, P < 0.01; SC: 0.32 R, P < 0.05). At rest, only in MA was a significant relationship evident, between mean arterial pressure value and IMT (P < 0.01).Conclusions:
In the absence of CV risk factors, only age is associated with a slight increase of wall carotid thickening. The data are indicative of a physiological increase in IMT, as a consequence of increased peak effort systolic pressure after regular PA in athletes.Keywords
1. Background
Carotid intima media thickness (IMT) is the ultrasound measurement of the two innermost layers of the arterial wall, where atherosclerotic damage begins before plaque occurrence. It has been proved that carotid IMT is an early marker of systemic subclinical atherosclerotic burden: in fact it is strictly related to atherosclerotic coronary involvement (1, 2). Literature highlights the role of carotid IMT as an early marker of systemic atherosclerotic burden, independently of the occurrence of traditional CV risk factors (3-5). In chronic metabolic diseases such as diabetes, high IMT values have been associated with postprandial metabolic derangements (5, 6). Despite this, however, has not uniformly supported a direct relationship between IMT and risk of atherosclerotic progression, as in the case of other chronic diseases with a low grade of inflammation, such as immunological diseases (7). An increase in IMT is generally associated with a decrease in vascular compliance (8) which is one of the main determinants of arterial blood pressure (BP). It is to be noted that vascular compliance is in any case the major cause of increase in blood pressure during physical exercise. The effects of regular physical activity and sports on cardiac remodeling have in fact been clearly demonstrated (9, 10). On the contrary the impact of regular physical activity on the arterial walls of peripheral vascular areas is still under debate.
2. Objectives
This study was aimed at evaluating the relationship between the hemodynamic and cardiac modifications induced by physical activity and IMT changes in a group of master athletes (MA) compared to sedentary subjects, enrolled as a SC. They were matched for age, sex and body surface. An inclusion criteria was the absence of traditional cardiovascular (CV) risk factors.
3. Patients and Methods
3.1. Study Population
The study population was composed of 151 subjects aged between 40-60 years, 109 males (82 MA and 27 SC) and 42 females (18 MA and 24 SC). All subjects examined were consecutively enrolled and the relative prevalence of males was due to the fact that the male population is more involved in regular physical activity than the female population. The low number of subjects in the control group was due to poor and irregular attendance of non-athletes at the sports medicine center. All subjects underwent scrupulous general clinical examination and medical history was taken in order to rule out the presence of cardiovascular or metabolic diseases as well as of main traditional cardiovascular risk factors. Exclusion criteria included: smoking habits during the previous 10 years, hypertension, dyslipidemia, diabetes, insulin resistance or glucose intolerance, familiarity for CV diseases and BMI > 25 kg/m2. Subjects affected by thyroid dysfunction were also excluded. According to the 2007 updated recommendations of the American College of Sports Medicine and the American Heart Association, we classified as athletes those subjects who performed regular training i.e. 2-3 hours of training per session at least three times a week. Physical training consisted of jogging or cycling at moderate intensity. On the contrary, we classified as sedentary all those subjects who only occasionally took part actively in sports (< 4 h/week) and low level of physical activity.
3.2. Study Protocol
The weekly level of physical activity was investigated by a dedicated questionnaire. The mean value of 4.4 ± 2.6 hours of weekly physical activity was considered the cut-off value to differentiate athletes from sedentary subjects. Both underwent a standard 2D echocardiographic Doppler examination and an ergometric treadmill test up to maximal tolerated effort according to a modified Bruce protocol that provides a gradual increase in workload every 2 minutes.
3.3. Carotid IMT Measurement
All testing was carried out in a blinded manner by two certified operators. In case of controversy, another sonographer was normally involved. Dedicated QIMT-Esaote software was used to measure the left and right IMT levels of the posterior wall of the common carotid, 1 centimeter from the beginning of bulb bifurcation, by ultrasound 2D exam. The IMT measurements were obtained according to the recommendations of the Italian Society of Vascular Diagnostics (11) and the standardized criteria described by Mannheim Carotid Intima Media Thickness Consensus to ensure full reliability (12). The manual image acquisition of carotid vessels was obtained before the automatic measurement of the intima-media using QIMT (Quality Intima Media Thickness) software, integrated into the instrument provided (Esaote MyLab 30 CV); QIMT software, using the RF (Radio Frequency Data Processing) signal in real-time, ensures high accuracy of a few µM, making it the method of choice for early detection of atherosclerosis.
3.4. Treadmill Exercise Test
The treadmill exercise test was conducted up to 85% of the estimated theoretical maximum heart rate for each subject, monitored by continuous ECG associated with systolic (SBP) and diastolic (DBP) blood pressure measurements, according to a modified Bruce protocol that provides for 7 or more stages. The first stage consisted of running with an initial gradient of 0.5% and with an initial scrolling speed of approximately 3 km/h. The incline was progressively increased up to the third stage by 10% and by 2% from the fourth stage on, and was associated with an increase in speed of 1.5 km/h at every stage.
3.5. Echocardiographic Study
Echocardiography was conducted by two experienced certified cardiologists who measured systolic and diastolic left ventricle (LV) parameters using an ESAOTE My Lab 50 echocardiograph equipped with a 2.5 MHz probe. Each subject was examined with mono-bidimensional echocardiographic and Doppler tests and according to the guidelines of the American Society of Echocardiography (13). The following parameters were measured: end-systolic and end-diastolic left ventricle diameters (LVEDd, LVESd), interventricular septum (IVS) and posterior wall (PW) thickness, left atrium (LA), and, aorta (Ao) root, starting from the parasternal long-axis view. The LV Mass Index (LVMI) was calculated following Devereux’s formula (14). Considering the regularity of the geometry of the left ventricular chamber of the subjects, the ejection fraction (EF %) was calculated according to the formula (LVEDd - LVESd/LVEDd), for which volumes are substituted by diameters. Analysis of the diastolic variables was performed in the presence of a stable RR interval and in three different but sequential measurements from the 4-chamber view consisting of the measurements, by Doppler analysis, of transmitral flow of E-wave and A-wave peak velocities, isovolumetric relaxation, and deceleration times and E/A ratio from 4-chamber view (13).
3.6. Statistical Analysis
All data are expressed as mean and standard deviation. The comparison of the mean values of the two groups was possible by ANOVA-two way method. The linear correlations among the parameters obtained were calculated with the Pearson index for each group. A p value < 0.05 was considered significant.
4. Results
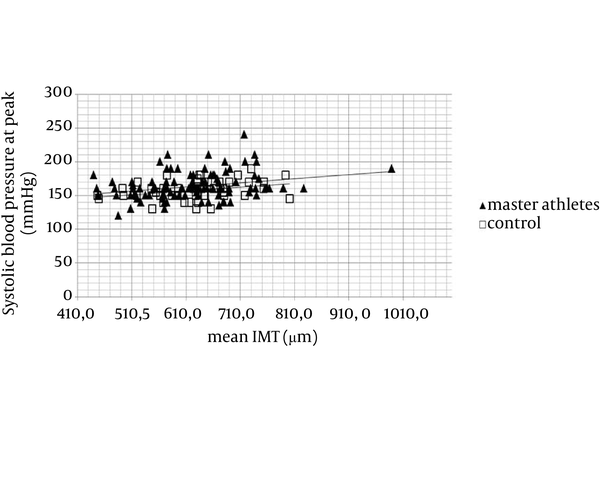
The two groups had similar demographic characteristics (Table 1). At rest, MA showed significantly (P < 0.01) lower mean HR values than SC but HR increase during exercise testing was similar in both athletes and sedentaries. Blood pressure at rest did not differ between the two groups, but systolic and diastolic blood pressure at peak of exercise was significantly higher in athletes than in controls. Among the echocardiographic parameters, LVM was significantly higher in MA than in SC, owing to larger systolic and diastolic diameters (Table 2). At the same time also aortic and atrium diameters were significantly larger in MA than in SC (Table 2). On the contrary the EF value did not differ between the two groups. The mean IMT value was within normal range in both groups with an average value of 624 ± 91.9 mm for MA and 627 ± 78.1 mm for SC (Table 3). If distinguished by gender, the IMT values of left and right carotid artery were within the normal range, despite a greater value in males than in females. IMT mean values in the MA group were 630 ± 93 for males and 601 ± 87.9 for females, while in SC the mean value was 645 ± 79.9 for males and 607 ± 72.5 for females. However, there was no significant difference between any of the values. IMT was significantly related to age (Table 4). No correlations were found between IMT and both echo parameters and the amount of physical activity, expressed as hours of physical activity per week (Table 4). Peak systolic blood pressure during exercise was significantly positively related to IMT in both groups, with a major significance in athletes (Figure 1). At rest, in MA but not in SC, mean blood pressure values were related to IMT average values.
General and Hemodynamic Data of the Exercise Test of Master Athletes and Sedentary Control a,b
| Variables | MA | SC | P Value |
|---|---|---|---|
| Gender | |||
| Female | 18 | 24 | |
| Male | 82 | 27 | |
| Age, y | 50.0 ± 6.7 | 51.1 ± 5.7 | NS |
| Body mass index, kg/m2 | 23.8 ± 2.5 | 24.0 ± 2.8 | NS |
| Weekly hours of sports activity | 7.0 ± 2.6 | < 4.0 ± 0.0 | 0.001 |
| IMT right, mm | 614 ± 104.2 | 622 ± 89.8 | NS |
| IMT left, mm | 635 ± 104.1 | 633 ± 98.4 | NS |
| Mean IMT, mm | 624 ± 91.9 | 627 ± 78.1 | NS |
| HR at rest | 72.4 ± 12.0 | 78.3 ± 10.4 | 0.003 |
| HR at peak | 152.7 ± 11.5 | 151.7 ± 8.7 | NS |
| HR at recovery | 87.7 ± 16.0 | 103.4 ± 67.5 | 0.03 |
| SBP, mmHg at rest | 118.2 ± 10.6 | 116.7 ± 10.5 | NS |
| DBP at rest, mmHg | 78.1 ± 8.1 | 76.9 ± 8.2 | NS |
| SBP peak, mmHg | 163.8 ± 19.7 | 157.7 ± 14.0 | 0.05 |
| DBP peak, mmHg | 71.0 ± 9.7 | 67.3 ± 8.7 | 0.02 |
| SBP recovery, mmHg | 123.5 ± 11.0 | 120.6 ± 12.8 | NS |
| DB recovery, mmHg | 75.3 ± 8.2 | 73.3 ± 8.6 | NS |
| SC | MA | P Value | |
|---|---|---|---|
| IVS, mm | 9.3 ± 0.8 | 9.4 ± 1.4 | NS |
| PW, mm | 9.1 ± 0.9 | 9.4± 1.4 | NS |
| LVEDd, mm | 47.7 ± 3.8 | 50.5 ± 3.5 | < 0.01 |
| LVESd, mm | 30.3 ± 2.9 | 32.0 ± 2.8 | < 0.01 |
| Aorta | 30.5 ± 3.2 | 32.3 ± 2.6 | < 0.01 |
| Atrium | 34.5 ± 3.8 | 36.5 ± 3.2 | < 0.01 |
| LVM, g | 168.6 ± 48.5 | 203.4 ± 42.2 | < 0.01 |
| LVMi, g/m2 | 92.4 ± 20.5 | 109.6 ± 20.2 | < 0.01 |
| RV, mm | 23.2 ± 2.1 | 23.2 ± 2.7 | NS |
| EF, % | 64.3 ± 3.4 | 64.7 ± 3.7 | NS |
Average IMT Values of Left and Right Carotid Vessel in Master Athletes and Sedentary Control a,b
| Variables | IMT Left Carotid | IMT Right Carotid | Mean IMT |
|---|---|---|---|
| Male SC | 658 ± 97.2 | 634 ± 94.9 | 645 ± 79.9 |
| Male MA | 641 ± 105.2 | 618 ± 104.6 | 629 ± 92.5 |
| Female SC | 602 ± 92.4 | 612 ± 83.2 | 608 ± 7 |
| Female MA | 601 ± 96.7 | 595 ± 1 | 601 ± 87.9 |
| Correlation | Pearson Index | P Value |
|---|---|---|
| Mean IMT Value-Systolic BP at Peak | ||
| MA | 0.280 | 0.004 |
| SC | 0.320 | 0.02 |
| Mean IMT Value-Systolic BP at Rest | ||
| MA | 0.17 | 0.08 NS |
| SC | 0.13 | 0.38 NS |
| Mean IMT Value-SBP Variation Rest-peak | ||
| MA | 0.23 | 0.02 |
| SC | 0.26 | 0.06 NS |
| Mean IMT Value-Age | ||
| MA | 0.300 | 0.002 |
| SC | 0.300 | 0.03 |
| Mean IMT Value-Weekly Hours of Sport | ||
| MA | 0.02 | 0.81 NS |
| Mean IMT Value-BMI | ||
| MA | 0.20 | 0.04 |
| SC | 0.12 | 0.40 NS |
| Mean IMT Value-Mean BP at Rest | ||
| MA | 0.25 | 0.01 |
| SC | 0.6 | NS |
| Mean IMT Value-Mean BP at Peak | ||
| MA | 0.23 | 0.2 |
| SC | 0.27 | NS |
| Mean IMT Value-Mean BP Variation Rest-peak | ||
| MA | 0.7 | NS |
| SC | 0.26 | NS |
Graph of Dispersion Mean Intima Media Thickness and Systolic Blood Pressure at the Peak of Exercise
5. Discussion
Carotid IMT is increasingly used as a surrogate marker for atherosclerosis (3). A number of longitudinal studies have examined the relationship between IMT and future events, most frequently the incidence of cardiac events such as myocardial infarction (MI), angina pectoris, coronary intervention but also cerebrovascular events such as stroke or transient ischemic attack (2). The measurement of carotid IMT can quantify the systemic burden of atherosclerosis (15); the role of CV risk factors in modulating IMT levels has been proven (10). There is also some evidence of the importance of IMT as a predictive parameter in the absence of cardiovascular risk factors (3). Previous studies have demonstrated that blood pressure is the main determinant of m-IMT, while the eventual interaction of this parameter with other risk factors like age and plasma lipids, is more relevant for advanced intima-media thickening such as mean-maximum (M-MAX) IMT (11, 12, 16). The present investigation considered the m-IMT parameter in a population with a very low cardiovascular risk profile. The results obtained show that IMT thickness is significantly related to aging, while regular physical activity does not appear to have an impact on this parameter, particularly in the absence of cardiovascular risk factors. However, some slight differences are evident between MA and SC males, where IMT values are lower in the first group with respect to the second, while on the contrary no differences were found among the female groups. This could suggest a distinctive and independent impact of physical activity within a particular group where there are no changes in pattern, as the result of progressive aging. Nevertheless, in consequence of the positive correlation found between mean SBP and IMT values, the possible role of SBP value in inducing evident increased thickness of the peripheral vessel wall needs to be considered as an unexpected component, particularly in the athletic population where physical activity is practiced regularly. In the absence of cardiovascular risks factors, in a population of similar age, blood pressure appears to maintain the principal role in inducing endothelium thickness and in reducing vascular compliance. In any case, bearing in mind the normal range of m-IMT and the positive correlation between m-IMT and mean SBP values at rest condition, the results found could be indicative of a physiological adaptation of the peripheral arteries to regular training, more evident in MA than in SC. This aspect confirms the universal importance of the role of regular physical activity. In addition, considering the BMI parameter as the principal indicator for metabolic risk factor, there is not sufficient evidence for its relevant role in inducing IMT modification, especially if compared with other life style parameters and particularly in the absence of other risk factors. In conclusion, despite the positive role of regular physical activity in preventing global cardiovascular risk and reducing any other possible metabolic risk factors, there is no evidence in the present investigation of a direct correlation between IMT and hours per week of physical activity, at least in MA, without evidence of cardiovascular risks factors. These findings suggest that physical activity has no direct impact on the IMT parameter in the absence of hypertension, diabetes, hypercholesterolemia etc., but it appears that it could more directly modify the heart but not the arteries. However, it is not possible to exclude the eventual indirect mediation of other aspects or mechanisms related to an incorrect life style not assessed in this study. This study was conducted on a wide population of subjects, however, the athletic population investigated was restricted to an MA class and no data are now available regarding the younger subjects. Another important limit of this study lies in the non-homogeneous composition by gender of the population investigated: both the groups were composed of a prevalence of male subjects. This in fact constitutes the principal limit and is mainly due to the specific composition of the population related to our center. This aspect might partially condition the interpretation of the data, despite the fact that the present analysis by gender shows no substantial positive correlation with the results. Further information is necessary in order to investigate the eventual role or relationship of IMT with relevant anthropometric parameters such as visceral fat and waist circumference, both strongly related to the metabolic syndrome and not investigated in the present study.
Acknowledgements
References
-
1.
Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997;96(5):1432-7. [PubMed ID: 9315528].
-
2.
Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115(4):459-67. [PubMed ID: 17242284]. https://doi.org/10.1161/CIRCULATIONAHA.106.628875.
-
3.
Pourafkari M, Bahtyari ET, Jalali AH. Ultrasonic Measurement of Carotid Intima–Media Thickness in a Group of Iranian with No Cardiovascular Risk Factors. Iran J Radiol. 2006;3(3).
-
4.
Alipour M, Masri D, Mofazzali A, Chitsazan M. Carotid Artery Intima-Media Thickness in Patients Undergoing Coronary Artery Bypass Graft Surgery. Arch Cardiovasc Imaging. 2013;1(1):26-30.
-
5.
Khamseh ME, Soltani K, Rafiee J, Mokhber A, Baradaran H. The Association of Carotid Intima-Media Thickness and Postprandial Dyslipidemia in Patients with Type 2 Diabetesv. Int J Endocrinol Metab. 2007;1:5-8.
-
6.
Alizadeh A, Roudbari A, Heidarzadeh A, Babaei Jandaghi A, Bani Jamali M. Ultrasonic measurement of common carotid intima-media thickness in type 2 diabetic and non-diabetic patients. Iran J Radiol. 2012;9(2):79-82. [PubMed ID: 23329968]. https://doi.org/10.5812/iranjradiol.7564.
-
7.
Zakeri Z, Saneie Sistani S, Bari Z, Ansari-Moghaddam A, Imani M, Reza Miradi M, et al. The Relationship Between Atherosclerosis and the Intima Media Thickness of Carotid Arteries With Serum C-Reactive Protein Levels in Patients With Systemic Lupus Erythematosus. Health Scope. 2012;1(2):57-60. https://doi.org/10.5812/jhs.6820.
-
8.
Lorenz MW, Polak JF, Kavousi M, Mathiesen EB, Volzke H, Tuomainen TP, et al. Carotid intima-media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): a meta-analysis of individual participant data. Lancet. 2012;379(9831):2053-62. [PubMed ID: 22541275]. https://doi.org/10.1016/S0140-6736(12)60441-3.
-
9.
Fox CS, Polak JF, Chazaro I, Cupples A, Wolf PA, D'Agostino RA, et al. Genetic and environmental contributions to atherosclerosis phenotypes in men and women: heritability of carotid intima-media thickness in the Framingham Heart Study. Stroke. 2003;34(2):397-401. [PubMed ID: 12574549].
-
10.
Kozakova M, Palombo C, Mhamdi L, Konrad T, Nilsson P, Staehr PB, et al. Habitual physical activity and vascular aging in a young to middle-age population at low cardiovascular risk. Stroke. 2007;38(9):2549-55. [PubMed ID: 17656659]. https://doi.org/10.1161/STROKEAHA.107.484949.
-
11.
Societa Italiana di Diagnostica Vascolare G. [Operative procedures for vascular diagnostic investigations. Guidelines of the Italian Society of Vascular Diagnosis (GUIV)]. Minerva Cardioangiol. 2000;48(9):303-55. [PubMed ID: 11130563].
-
12.
Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Desvarieux M, et al. Mannheim intima-media thickness consensus. Cerebrovasc Dis. 2004;18(4):346-9. [PubMed ID: 15523176]. https://doi.org/10.1159/000081812.
-
13.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440-63. [PubMed ID: 16376782]. https://doi.org/10.1016/j.echo.2005.10.005.
-
14.
Devereux RB. Detection of left ventricular hypertrophy by M-mode echocardiography. Anatomic validation, standardization, and comparison to other methods. Hypertension. 1987;9(2 Pt 2):II19-26. [PubMed ID: 2948914].
-
15.
Bauer M, Delaney JA, Mohlenkamp S, Jockel KH, Kronmal RA, Lehmann N, et al. Comparison of factors associated with carotid intima-media thickness in the Multi-ethnic Study of Atherosclerosis (MESA) and the Heinz Nixdorf Recall Study (HNR). J Am Soc Echocardiogr. 2013;26(6):667-73. [PubMed ID: 23611058]. https://doi.org/10.1016/j.echo.2013.03.011.
-
16.
Pauletto P, Palatini P, Da Ros S, Pagliara V, Santipolo N, Baccillieri S, et al. Factors underlying the increase in carotid intima-media thickness in borderline hypertensives. Arterioscler Thromb Vasc Biol. 1999;19(5):1231-7. [PubMed ID: 10323774].