Abstract
Context:
In the last few years, humanity has faced one of the most twisted pandemics in history. The COVID-19 pandemic has had a significant impact on people’s lives during its outbreak, especially on people with underlying diseases such as diabetes. This study reviewed diabetes care during the COVID-19 outbreak to facilitate diabetes management during the coronavirus outbreak and promote the survival of these patients in this global pandemic.Methods:
This work was done as a study on diabetes and coronavirus. Scopus, PubMed, and Web of Science databases were searched on January 20, 2021.Results:
Studies demonstrated that diabetes is not the leading cause of comorbidity or ultimate cause of mortality or morbidity of COVID-19 disease, as mentioned above.Conclusions:
This review study concluded that with the peak of the coronavirus, diabetes management is critical. Besides, providing conditions to maintain the health of diabetic patients by informing them and communicating effectively with healthcare personnel is of great importance.Keywords
1. Context
In late 2019, a new virus causing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a coronavirus, was reported in Wuhan, a Chinese city (1). Coronavirus disease 2019 (COVID-19) spread rapidly in various countries and was recognized by the World Health Organization on 11 March 2020 as a global epidemic (2). Severe acute respiratory syndrome coronavirus 2, known as COVID-19, is a mild acute respiratory illness that may become complicated with severe pneumonia, leading to respiratory failure and septic shock. Severe coronary heart disease affects mainly adults with underlying comorbidities such as hypertension, diabetes, cardiovascular disease, chronic lung disease, cancer, and chronic kidney diseases (3, 4). In patients with coronary heart disease, several studies have demonstrated that comorbidities are present in approximately half of the hospitalized patients with COVID-19, with hypertension being the most common comorbidity, followed by diabetes and coronary heart disease (CHD) (5-7).
According to the present evidence, the outbreak of COVID-19 is complicated. The epidemiological criteria for a global epidemic with an infection rate of over 100,000 people per 100 countries have been established (8). The COVID-19 epidemic mainly kills the elderly and high-risk individuals. People with severe diseases caused by underlying risk factors, such as diabetes, are at higher risk. For severe cases of COVID-19 and its complications, high mortality of up to 50% is predicted (9).
Diabetes mellitus (DM) is a disease with high blood sugar levels and is a severe risk to human health. According to statistical reports, in the last twenty years, the number of diabetic patients has been increasing (10). In 1985, the number of diabetics around the world was about 30 million; in 2010, that number rose to approximately 285 million. According to the statistics from the International Diabetes Federation, the number of people with diabetes in 2019 will reach 463 million. It is estimated that by 2045, about 700 million people will be affected (11, 12). In 2011, the prevalence of diabetes in Iran in individuals between 25 and 70 years was 11.9%. The reported results demonstrated a 35% increase compared to 2005. With this increasing trend, it is estimated that, in 2030, about 2.9 Iranians will have diabetes (13).
Uncontrolled DM can lead to irreversible complications such as blindness, kidney failure, cardiovascular problems, diabetic foot ulcers, amputation, infection, and genital disorders such as infertility and erectile dysfunction in men. These complications can cause disability in these patients (14, 15).
People with diabetes mellitus have a potentially high risk of contracting COVID-19 and its complications for various reasons. The mortality rate in people with diabetes is reported to be up to 50% higher than in non-diabetic controls. Measures such as “quarantine” impose different risks on people with diabetes regarding diet, exercise, medication availability, and stress, which can impede glycemic control with the consequence of uncontrolled hyperglycemia and worsening the condition in these people (9, 16).
Since the beginning of the pandemic, several countries have taken measures to curb the corona spread. Actions such as screening, health education, quarantine, and widespread vaccination worldwide have been prioritized in the essential programs of various countries.
In this study, we reviewed the therapeutic measures and strategies studied in self-care and diabetes management against the COVID-19 pandemic. Since the outbreak of COVID-19, many communities have attempted to care for high-risk individuals, such as diabetics. In this regard, particular recommendations and care measures for diabetics have been provided for self-management to cope with the coronavirus. Maintaining the community’s health is very important, and we have tried to summarize these interventions in this study.
The purpose of this study was to promote the health of people with diabetes by investigating the relationship between blood sugar levels in diabetic patients and its consequences regarding different strains of coronavirus. To realize this, related situations in this field have been investigated, and useful review articles were analyzed and reported.
2. Methods
This work was done as a study in diabetes and coronavirus. Scopus, PubMed, and Web of Science databases were searched on January 20, 2021. All kinds of eligible articles on diabetes and coronavirus published in recent years were evaluated. A total of 32 articles (80%) were published in Q1 journals, and nine (20%) were related to other international studies. There were few review articles on primary care in diabetes during the coronavirus outbreak.
3. Discussion
3.1. Association Between Diabetes Mellitus and the Coronavirus
Patients with underlying diseases such as uncontrolled diabetes, hypertension, and cardiovascular disease, as well as the elderly, are more prone to severe clinical consequences, as well as a higher rate of COVID-19-related complications (17, 18). According to evidence, diabetes, especially in men, the elderly, senescence obesity, high blood pressure, and heart disease, predisposes people to the development of COVID-19 with severe and lethal consequences such as accumulation of cytokines, thrombose, and eventually death. Many patients in India had diabetic ketoacidosis as the first presentation of the disease. COVID-19 in diabetic patients causes severe hyperglycemia. Infection with the coronavirus can also cause high blood sugar symptoms in people with an unmasked diabetes condition. Ten percent of patients with COVID-19 with no history of diabetes develop high blood sugar after COVID-19 infection, which can be due to the detrimental effects of the virus on the pancreas. Approximately one-third of coronavirus deaths occur in people with diabetes (19). A study in Hong Kong showed that in 115 patients with SARS-CoV, the diabetes mortality rate increased (20). Also, in 2009, the results of a study demonstrated severe complications during the influenza A (H1N1) epidemic in people with diabetes (21). In another study on MERS-CoV, the results showed that approximately 50% of 637 patients infected with the virus had diabetes (3). The presence of diabetes in patients with COVID-19 depends on the study population. Statistical studies in China demonstrated that in a study of 1,099 patients with COVID-19, 7.4% had diabetes (22).
In a meta-analysis study in 2019, the results of 7 studies involving 1,576 patients from China demonstrated that after hypertension, diabetes was the second most common comorbidity in patients with COVID-19, and about 9.7% of patients had diabetes (23). In a study in Italy, an analysis of COVID-19 consequences in 1591 patients admitted to the intensive care unit demonstrated that the rates of underlying diseases in hospitalized patients were: blood pressure (49%), cardiovascular disorders (21%), high cholesterol (18%) and diabetes (17%) (24). The results of observational studies demonstrated that the leading cause of death in patients with COVID-19 was diabetes, and the complications of COVID-19 in people with diabetes were very severe, which could be responsible for various complications in these patients (25). Since diabetes is associated with immune system disorders, diabetics are more likely to contract infections than non-diabetics. Uncontrolled hyperglycemia in diabetics can lead to degenerative changes, decreased phagocytosis, endovascular adhesion to the endothelium, and decreased intracellular bactericidal activity (26). Also, uncontrolled diabetes can lead to complications such as vascular injuries and subsequent neuropathic injuries, which can cause infection in diabetics (27). Diabetes and obesity are associated with chronic inflammation caused by increased secretion of adipose tissue leptin and cytokines hormones such as tumor necrosis factor α (TNFα) and interleukin 6 (IL-6), which play an essential role in insulin resistance (28). The results of several studies indicate that diabetes has adverse effects on patients’ clinical outcomes. However, these results are not conclusive and need further investigation. Several studies have demonstrated that diabetes is a significant determinant of adverse clinical outcomes in patients with COVID-19 (6). According to the results of some studies, acute hyperglycemia is associated with the risk of COVID-19. This new hypothesis has been the focus of much research during the current epidemic, and similar studies will continue in this field. Yang et al. and Mirzaei et al. reported that during the previous SARS epidemic, diabetes and hyperglycemia were associated with poor prognoses (29, 30). In a 2015 study on ICU patients, Liao et al. found that stress-induced hyperglycemia was an independent and related factor in increasing the risk of death in nondiabetic patients (31). In a study on diabetic patients admitted to the ICU between 2011 and 2014, it was observed that levels of glycated hemoglobin A or hemoglobin A1c (HbA1c) in people with a glucose gap greater than 80 mg/dL were significantly higher in deceased patients than in diabetics with a glucose gap less than 80 mg/dL. Among the identified causes of death in the mentioned study, 38.8% were related to respiratory failures, and 59.5% were related to underlying infections (31). Researchers have suggested that HIV AIDS is important in predicting mortality in critically ill patients. In these studies, the severity of HIV AIDS has been linked to the severity of the disease. In humans, stress-induced hyperglycemia (SIH) can transform severe adaptive responses to a serious illness that can cause the body to over-release cytokines and anti-regulatory hormones, resulting in insulin resistance (32). Controlled diabetes with regular quarterly monitoring of HbA1c levels can play an important role in managing the disease in people with diabetes and keeping the body free from inflammation. In a 2020 study by Raufi et al., they examined the effects of good and poor diabetes control in 117 COVID-19 patients with diabetes and reported that 79.5% of patients had poor management, and 20.5% had good glycemic control (33). Nonetheless, CT scan images in the two groups were not significantly different. The observed mortality and recovery rates were also the same in both groups. This indicates that the outcomes of the study could be more reliable according to the results of HbA1c. Since this study was observational, the results cannot be compared with the results of another study, and they may seem contradictory (33, 34).
3.2. Management of Diabetes During the COVID-19
The outbreak of coronavirus is a high-risk period for diabetics. Therefore, to avoid physical and face-to-face contact and to prevent unwanted gatherings of diabetic patients, especially patients with diabetes complications, diabetic patients are advised to use telemedicine as much as possible (35). Examination of molecular events in the body of diabetic patients exposed to the coronavirus demonstrated a link between this virus and diabetes. COVID-19 activates the enzyme dipeptidyl peptidase-4 (DPP-4) in these patients. The enzyme dipeptidyl peptidase is a practical replicator of the COVID-19 virus. Dipeptidyl peptidase-4 is a membrane-specific glycoprotein that plays a crucial role in glucose and insulin metabolism and, under certain conditions, increases inflammation. Although the mechanism of DPP-4 suppressant drugs is not yet known, they may be effective in treating COVID-19 patients with diabetes (35, 36). In managing their disease, diabetic patients should consider their blood sugar control as a primary prevention against COVID-19, and this control should be comprehensive. Besides controlling blood sugar, other parameters, such as blood pressure and blood lipids, should also be controlled. Additionally, remote medical counseling should be taken more seriously by these patients than before. Diabetics should take the WHO and CDC guidelines for regular hand washing and social distancing seriously (37, 38). People with diabetes, especially groups that have diabetes with side effects, need more consideration and care. Elevated HbA1c levels in people with diabetes, especially type 1 diabetes, can lead to the malfunction of the immune system, which in turn, predisposes them to infectious diseases such as COVID-19 (39). Today, the increase in the number of patients with type 2 diabetes, accompanied by fatty liver disease in many due to the increase in cytokines in the blood, makes them very susceptible to inflammatory reactions. These people are considered the high-risk groups with COVID-19 disease and need special care (40). It is important to determine the diabetes subtypes and study how they are related to the COVID-19 consequences, particularly whether some different management approaches will be effective in managing COVID-19 diabetes (16).
3.3. Conclusions
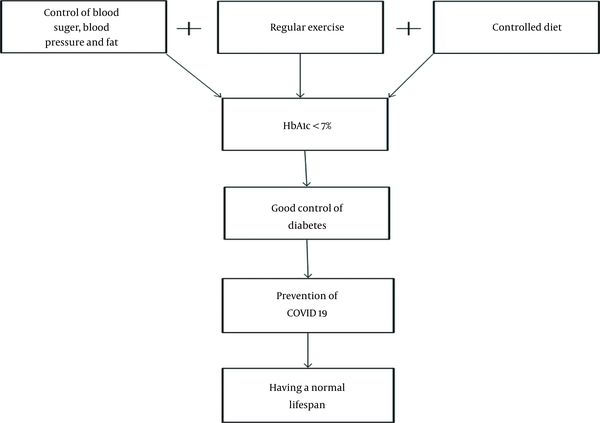
Although vaccinations have worked well these days, nothing is yet certain, and diabetics should improve their blood sugar control by following health guidelines, avoiding crowds, and performing aerobic exercises such as walking and cycling. Diabetic patients, especially in this epidemic, should ensure that their blood sugar is controlled by regular HbA1c monitoring every three months to manage their condition well. Following a regular diet prescribed by nutritionists is recommended to control diabetes and ensure that they have normal blood sugar levels during the outbreak of the coronavirus and its new strains. The results of this review study are illustrated in Figure 1.
The three basic principles of diabetes control and the benefits of control
References
-
1.
Qu YM, Kang EM, Cong HY. Positive result of Sars-Cov-2 in sputum from a cured patient with COVID-19. Travel Med Infect Dis. 2020;34:101619. [PubMed ID: 32160971]. [PubMed Central ID: PMC7129439]. https://doi.org/10.1016/j.tmaid.2020.101619.
-
2.
Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157-60. [PubMed ID: 32191675]. [PubMed Central ID: PMC7569573]. https://doi.org/10.23750/abm.v91i1.9397.
-
3.
Shi J, Wen Z, Zhong G, Yang H, Wang C, Huang B, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020;368(6494):1016-20. [PubMed ID: 32269068]. [PubMed Central ID: PMC7164390]. https://doi.org/10.1126/science.abb7015.
-
4.
Peng QY, Wang XT, Zhang LN, Chinese Critical Care Ultrasound Study G. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020;46(5):849-50. [PubMed ID: 32166346]. [PubMed Central ID: PMC7080149]. https://doi.org/10.1007/s00134-020-05996-6.
-
5.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. [PubMed ID: 31986264]. [PubMed Central ID: PMC7159299]. https://doi.org/10.1016/S0140-6736(20)30183-5.
-
6.
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531-8. [PubMed ID: 32161990]. [PubMed Central ID: PMC7087935]. https://doi.org/10.1007/s00392-020-01626-9.
-
7.
Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020;12(7):6049-57. [PubMed ID: 32267833]. [PubMed Central ID: PMC7185114]. https://doi.org/10.18632/aging.103000.
-
8.
Callaway E. Time to use the p-word? Coronavirus enters dangerous new phase. Nature. 2020. [PubMed ID: 33623145]. https://doi.org/10.1038/d41586-020-00551-1.
-
9.
Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225-8. [PubMed ID: 32178769]. [PubMed Central ID: PMC7102589]. https://doi.org/10.1016/S0140-6736(20)30627-9.
-
10.
Ramachandran A, Snehalatha C, Shetty AS, Nanditha A. Trends in prevalence of diabetes in Asian countries. World J Diabetes. 2012;3(6):110-7. [PubMed ID: 22737281]. [PubMed Central ID: PMC3382707]. https://doi.org/10.4239/wjd.v3.i6.110.
-
11.
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4-14. [PubMed ID: 19896746]. https://doi.org/10.1016/j.diabres.2009.10.007.
-
12.
International Diabetes Federation Executive Office. IDF diabetes atlas. 5th ed. Brussels, Belgium: International Diabetes Federation; 2011.
-
13.
Mirzaei M, Rahmaninan M, Mirzaei M, Nadjarzadeh A, Dehghani Tafti AA. Epidemiology of diabetes mellitus, pre-diabetes, undiagnosed and uncontrolled diabetes in Central Iran: results from Yazd health study. BMC Public Health. 2020;20(1):166. [PubMed ID: 32013917]. [PubMed Central ID: PMC6998152]. https://doi.org/10.1186/s12889-020-8267-y.
-
14.
Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311-21. [PubMed ID: 22079683]. https://doi.org/10.1016/j.diabres.2011.10.029.
-
15.
Hamano K, Nakadaira I, Suzuki J, Gonai M. N-terminal fragment of probrain natriuretic peptide is associated with diabetes microvascular complications in type 2 diabetes. Vasc Health Risk Manag. 2014;10:585-9. [PubMed ID: 25328404]. [PubMed Central ID: PMC4199566]. https://doi.org/10.2147/VHRM.S67753.
-
16.
Wondafrash DZ, Desalegn TZ, Yimer EM, Tsige AG, Adamu BA, Zewdie KA. Potential Effect of Hydroxychloroquine in Diabetes Mellitus: A Systematic Review on Preclinical and Clinical Trial Studies. J Diabetes Res. 2020;2020:5214751. [PubMed ID: 32190699]. [PubMed Central ID: PMC7064866]. https://doi.org/10.1155/2020/5214751.
-
17.
Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475-81. [PubMed ID: 32105632]. [PubMed Central ID: PMC7102538]. https://doi.org/10.1016/S2213-2600(20)30079-5.
-
18.
Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75(7):1730-41. [PubMed ID: 32077115]. https://doi.org/10.1111/all.14238.
-
19.
Joshi SR, Tiwaskar MH, Shah SN. COVID 19: Diabetes and Obesity API-ICP Recommendations. J Assoc Physicians India. 2020;68(5):42-4. [PubMed ID: 32610865].
-
20.
Chan JW, Ng CK, Chan YH, Mok TY, Lee S, Chu SY, et al. Short term outcome and risk factors for adverse clinical outcomes in adults with severe acute respiratory syndrome (SARS). Thorax. 2003;58(8):686-9. [PubMed ID: 12885985]. [PubMed Central ID: PMC1746764]. https://doi.org/10.1136/thorax.58.8.686.
-
21.
Allard R, Leclerc P, Tremblay C, Tannenbaum TN. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care. 2010;33(7):1491-3. [PubMed ID: 20587722]. [PubMed Central ID: PMC2890346]. https://doi.org/10.2337/dc09-2215.
-
22.
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. [PubMed ID: 32109013]. [PubMed Central ID: PMC7092819]. https://doi.org/10.1056/NEJMoa2002032.
-
23.
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-5. [PubMed ID: 32173574]. [PubMed Central ID: PMC7194638]. https://doi.org/10.1016/j.ijid.2020.03.017.
-
24.
Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574-81. [PubMed ID: 32250385]. [PubMed Central ID: PMC7136855]. https://doi.org/10.1001/jama.2020.5394.
-
25.
World Health Organization. WHO delivers advice and support for older people during COVID-19. Geneva, Switzerland: World Health Organization; 2020. Available from: https://www.who.int/news-room/feature-stories/detail/who-delivers-advice-and-support-for-older-people-during-covid-19.
-
26.
Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol. 1999;26(3-4):259-65. [PubMed ID: 10575137]. https://doi.org/10.1111/j.1574-695X.1999.tb01397.x.
-
27.
Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J Endocrinol Metab. 2012;16 Suppl 1(Suppl1):S27-36. [PubMed ID: 22701840]. [PubMed Central ID: PMC3354930]. https://doi.org/10.4103/2230-8210.94253.
-
28.
Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: an endocrine organ. Arch Med Sci. 2013;9(2):191-200. [PubMed ID: 23671428]. [PubMed Central ID: PMC3648822]. https://doi.org/10.5114/aoms.2013.33181.
-
29.
Yang JK, Feng Y, Yuan MY, Yuan SY, Fu HJ, Wu BY, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med. 2006;23(6):623-8. [PubMed ID: 16759303]. https://doi.org/10.1111/j.1464-5491.2006.01861.x.
-
30.
Mirzaei F, Khodadadi I, Vafaei SA, Abbasi-Oshaghi E, Tayebinia H, Farahani F. Importance of hyperglycemia in COVID-19 intensive-care patients: Mechanism and treatment strategy. Prim Care Diabetes. 2021;15(3):409-16. [PubMed ID: 33436320]. [PubMed Central ID: PMC7834268]. https://doi.org/10.1016/j.pcd.2021.01.002.
-
31.
Liao WI, Wang JC, Chang WC, Hsu CW, Chu CM, Tsai SH. Usefulness of Glycemic Gap to Predict ICU Mortality in Critically Ill Patients With Diabetes. Medicine (Baltimore). 2015;94(36). e1525. [PubMed ID: 26356728]. [PubMed Central ID: PMC4616648]. https://doi.org/10.1097/MD.0000000000001525.
-
32.
Marik PE, Bellomo R. Stress hyperglycemia: an essential survival response!. Crit Care. 2013;17(2):305. [PubMed ID: 23470218]. [PubMed Central ID: PMC3672537]. https://doi.org/10.1186/cc12514.
-
33.
Raoufi M, Khalili S, Mansouri M, Mahdavi A, Khalili N. Well-controlled vs poorly-controlled diabetes in patients with COVID-19: Are there any differences in outcomes and imaging findings? Diabetes Res Clin Pract. 2020;166:108286. [PubMed ID: 32592836]. [PubMed Central ID: PMC7314673]. https://doi.org/10.1016/j.diabres.2020.108286.
-
34.
Su YW, Hsu CY, Guo YW, Chen HS. Usefulness of the plasma glucose concentration-to-HbA(1c) ratio in predicting clinical outcomes during acute illness with extreme hyperglycaemia. Diabetes Metab. 2017;43(1):40-7. [PubMed ID: 27663631]. https://doi.org/10.1016/j.diabet.2016.07.036.
-
35.
Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8(6):546-50. [PubMed ID: 32334646]. [PubMed Central ID: PMC7180013]. https://doi.org/10.1016/S2213-8587(20)30152-2.
-
36.
Kokic Males V. Letter to the editor in response to the article "COVID-19 and diabetes: Can DPP4 inhibition play a role?". Diabetes Res Clin Pract. 2020;163:108163. [PubMed ID: 32333972]. [PubMed Central ID: PMC7177108]. https://doi.org/10.1016/j.diabres.2020.108163.
-
37.
Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4). e21. [PubMed ID: 32171062]. [PubMed Central ID: PMC7118626]. https://doi.org/10.1016/S2213-2600(20)30116-8.
-
38.
Roncon L, Zuin M, Rigatelli G, Zuliani G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol. 2020;127:104354. [PubMed ID: 32305882]. [PubMed Central ID: PMC7195018]. https://doi.org/10.1016/j.jcv.2020.104354.
-
39.
Andersen CJ, Murphy KE, Fernandez ML. Impact of Obesity and Metabolic Syndrome on Immunity. Adv Nutr. 2016;7(1):66-75. [PubMed ID: 26773015]. [PubMed Central ID: PMC4717890]. https://doi.org/10.3945/an.115.010207.
-
40.
Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017;127(1):1-4. [PubMed ID: 28045402]. [PubMed Central ID: PMC5199709]. https://doi.org/10.1172/JCI92035.