Abstract
Background:
Breast pain is one of the most common reasons for referral to breast imaging.Objectives:
This study aimed to determine the diagnostic yield of mammography and sonomammography in women complaining of breast pain in a teaching hospital in Southeast Nigeria.Methods:
This descriptive study analyzed the mammographic/sonomammographic images and records of 241 consecutive adult women aged 18 - 81 years with breast pain who presented to the radiology department over three years. A non-random sampling method was employed to select the participants. The extracted variables were patient’s age, positive clinical history of breast pain, laterality of breast pain, type of imaging, presence or absence of lesion, type, and laterality of lesions if present, and Breast Imaging Reporting and Data System (BI-RADS) assignment of imaging findings on mammography and sonomammography. The descriptive analysis of continuous variables and inferential statistics of ordinal data were performed with Microsoft Excel and chi-squared test, respectively. In this study, P < 0.05 was set as the significance level.Results:
Most women (20%) with a complaint of breast pain were in the 40 - 44-year age group. Moreover, 32.3%, 33.2%, and 34.4% of the participants had left-sided, right-sided, and bilateral breast pain, respectively. Among the participants, 118 and 123 women had mammography and sonomammography, respectively. Furthermore, 76.3% had normal findings on mammography or sonomammography, and only 23.7% had positive imaging findings on breast imaging. These lesions were mostly observed among the women in the age group of 45 - 49 years. Of those with lesions detected on imaging, 79.2% and 20.8% demonstrated benign and malignant attributes, respectively. Masses with definite benign attributes assigned BI-RADS II were mostly fibroadenomata and cysts. Inferential statistics indicated that unilateral mastalgia was more likely to be associated with a breast lesion, while bilateral mastalgia usually resulted in normal breast imaging findings.Conclusions:
Women referring to the Radiology Department with a complaint of breast pain alone are unlikely to have any significant breast imaging finding; hence, imaging serves as a tool for assuaging the anxiety of these patients and reassuring the referring physician. Unilateral but not bilateral mastalgia is likely to yield positive imaging findings, which are largely benign.Keywords
Breast Pain Mastalgia Sonomammography Breast Ultrasound Cancer Mammography.
1. Background
Breast pain, also known as mastalgia, mastodynia, or mammalgia, can be cyclical or non-cyclical, bilateral or unilateral, intermittent or continuous, and diffuse or focal. Mammalgia is one of the most typical breast complaints among women requiring medical attention (1) at breast clinics and imaging departments (2-4). According to some statistics, about 45 - 70% of breast-related symptoms in the primary care setting are associated with breast pain (5), and this type of pain is more common than breast cancer (6). Some reports have indicated that 50 - 80% of women experience mastalgia in their lifetime (7, 8).
Three types of breast pain are introduced: cyclical, non-cyclical, and extramammary (9). Cyclical mastalgia is associated with the menstrual cycle and usually occurs in both breasts diffusely. It is felt as soreness or heaviness at the breast and radiates to the axilla and arms (10, 11). It is more frequent in younger females and is resolved spontaneously. Non-cyclical mastalgia is not associated with the menstrual cycle. This type of pain can be persistent or intermittent. Extramammary pain arises from the chest wall but is felt within the breast (musculoskeletal chest pain). Some examples of extramammary pain are costochondritis, Tietze syndrome, and others (7, 9, 12). This type may be unilateral and localized in the breast, being observed more frequently in females aged 40 - 50 years. Extramammary pain is felt as a burning, sharp pain (10, 13).
Although breast pain, as the only symptom, is a low risk factor of breast cancer (9, 14), it leads to remarkable morbidity, anxiety and generally influences of the quality of life worldwide (15, 16). These women often seek medical attention due to concerns about possible breast cancer as the most typical female cancer worldwide (17-19). Studies have recommended imaging in patients who need reassurance (20).
In addition to clinical breast examination (CBE), imaging techniques such as sonomammography and mammography play a pivotal role in evaluating the painful breast, especially when there is a palpable mass. Sonomammography uses high-frequency sound waves above the human audible range (20 Hz - 20,000 Hz) to produce the images of the concerned area (3). This technique is highly acceptable for evaluating a dense breast, differentiating cystic from solid masses, and assessing highly painful breast in a patient who cannot withstand the compression involved with mammography examination. Mammography utilizes low-dose X-rays with breast compression to produce high-quality breast images revealing microcalcifications (21). In the absence of a palpable mass, the same tools are deployed to exclude an occult lesion in younger and older women, respectively, or to be used in combination (16).
Countries such as America, Europe, and Asia have had clinical trials and developed guidelines to help clinicians manage women with breast pain (15, 22). However, management schedules in African society are still in their infantile stage. On the other hand, imaging findings in women who present with breast pain in Southeast Nigeria have not been evaluated.
2. Objectives
This study aimed to determine the diagnostic yield of mammography and sonomammography in women complaining of breast pain in a teaching hospital in Southeast Nigeria from January 2015 to December 2017.
3. Methods
This study was approved by the ethics committee of a Teaching Hospital affiliated with the University of Nigeria, Ituku/Ozalla, Enugu, Nigeria.
We used a questionnaire to obtain biodata and past medical history of the subjects. Then, each subject signed the consent page in the questionnaire. Clinical breast examination was done, followed by breast imaging. The mammographic examination was performed using GE Alpha RT mammography machine, with a molybdenum cathode/target combination. Exposure factors were generally a low tube voltage ranging from 25 - 35 kVp and an mAs of 200. The mammographic images were acquired using film/screen combinations and stored physically with hardcopy reports in an archival room. Sonomammography was performed with a Toshiba ultrasound machine, with a linear transducer at frequencies ranging from 7.5 to 10 MHz, depending on the breast size. The images and reports were stored on a digital archive on a computer's hard drive, and the hard copies were stored in secure cardboard paper files.
A retrospective analysis was performed on breast imaging questionnaires and the mammographic and sonomammographic reports of 241 women with breast pain referring to the radiology department of our hospital during a three-years period from January 2015 to December 2017. A non-random sampling method was employed to select the participants. The following variables were extracted from the records, questionnaires, and radiologic reports: Patients’ age, positive clinical history of breast pain, laterality of breast pain, type of imaging, presence or absence of lesions, type and laterality of lesions if present, and Breast Imaging Reporting and Data System (BI-RADS) assignment of imaging findings on mammography and sonomammography.
Microsoft Excel 2013 (Microsoft Inc, Redmond, Washington, USA) was used for the descriptive analysis and display of the following variables: Frequency of breast pain amongst different age groups of the women, the laterality of symptoms, and the BI-RADS assignment of the lesions identified on either mammography or sonomammography amongst different age groups. Inferential statistics, including chi-squared test (GraphPad Prism, Version 5.03 (Graphpad Software Inc. USA, 1992-2010)), was used to compare the incidence of positive and negative imaging findings among the participants with unilateral and bilateral mastalgia. The significance level was set at P < 0.05.
4. Results
Two hundred and forty-one women referred to the radiology department with a complaint of breast pain, most (20%) of whom were in 40 - 44 years old range (Table 1). Moreover, 65.6% and 34.4% of the women had unilateral and bilateral breast pain, respectively (Table 1). According to the BI-RADS lexicon, 76.4% of the women with mastalgia, either unilateral or bilateral, ended up with BI-RADS 1, i.e., no mammographic/sonomammographic abnormality, and 21.9% had positive imaging findings (Table 2). These were predominantly benign breast masses such as fibroadenomata and cysts, mainly observed in the participants in the age group of 45 - 49 years. When lesions emerged, they were mostly benign-BI-RADS 2. Moreover, the higher grade BI-RADS (4 or 5) lesions occurred more in patients with unilateral mastalgia (Table 2). The lesions diagnosed in positive cases were simple fibroadenoma, breast cysts, fibrocystic breast disease, lactational and non-lactational breast abscesses, breast cancer, fat necrosis, mastitis, and Mondor’s disease. In this regard, 88% of women with bilateral mastalgia had negative/normal imaging findings (BI-RADS I). Chi-Square analysis revealed a P-value of 0.0089 (P < 0.05), thereby confirming that imaging the breasts of women with bilateral mastalgia will likely not yield any pathology (Table 3).
Frequency and Laterality of Breast Pain in Different Age Groups Presenting for Mammography and Sonomammography
| Age Range (y) | Types of Examination | Breast Pain | ||||
|---|---|---|---|---|---|---|
| Mammography | Sonomammography | Total | Unilateral | Bilateral | Total | |
| < 20 | 0 | 10 | 10 | 7 | 4 | 10 |
| 20 - 24 | 0 | 10 | 10 | 7 | 3 | 10 |
| 25 - 29 | 1 | 30 | 31 | 18 | 13 | 31 |
| 30 - 34 | 0 | 16 | 16 | 10 | 6 | 16 |
| 35 - 39 | 16 | 16 | 32 | 27 | 5 | 32 |
| 40 - 44 | 33 | 16 | 49 | 32 | 17 | 49 |
| 45 - 49 | 23 | 11 | 34 | 19 | 15 | 34 |
| 50 - 54 | 23 | 6 | 29 | 19 | 10 | 29 |
| 55 - 59 | 9 | 5 | 14 | 10 | 4 | 14 |
| 60 - 64 | 11 | 2 | 13 | 6 | 7 | 13 |
| > 64 | 2 | 1 | 3 | 3 | 0 | 3 |
| Total | 118 | 123 | 241 | 158 (65.6%) | 83 (34.4%) | 241 |
| Breast Imaging Reporting and Data System (BI-RADS) Assignment | Unilateral Mastalgia | Bilateral Mastalgia | Sub-total | Interpretation | Total |
|---|---|---|---|---|---|
| BI-RADS 0 | 4 (2.5) | 0 | 4 (1.7) | Inconclusive | 4 (1.7) |
| BI-RADS I | 111 (70.3) | 73 (88) | 184 (76.4) | Normal | 184(76.4) |
| BI-RADS II | 19 (12) | 10 (12) | 29 (12) | Benign | 42 (17.4) |
| BI-RADS III | 13 (8.2) | 0 | 13 (5.4) | ||
| BI-RADS IV | 2 (1.3) | 0 | 2 (0.8) | Malignant | 11 (4.5) |
| BI-RADS V | 9 (5.7) | 0 | 9 (3.7) | ||
| Total | 158 (100) | 83 (100) | 241 | 241(100) |
Comparison of Positive and Negative Imaging Findings in Patients with Unilateral and Bilateral Mastalgia
| Imaging Findings | Laterality of Mastalgia | ||
|---|---|---|---|
| Unilateral Mastalgia | Bilateral Mastalgia | Total | |
| Positive imaging findings | 47 (29.8) | 10 (12) | 57 |
| Negative imaging findings | 111 (70.2) | 73 (88) | 184 |
| Total | 158 (100) | 83 (100) | 241 |
5. Discussion
Breast pain seems to be more prevalent in the 5th decade of life among the research participants. The women complaining of breast pain mainly belonged to the age group of 40 - 49 years (n = 83, 34.4%). This finding agrees with those of some other studies in Ghana, the USA, and Australia, reporting mastalgia to be predominant among women passing their 5th decade of life (2, 3, 16, 23). In our study, painful breast masses were most reported in women aged 40 - 49 years (35% of all cases). Furthermore, 65.6% and 34.4% of the women had unilateral and bilateral mastalgia, respectively. This finding is similar to previous works suggesting relatively fewer women experiencing bilateral mastalgia (1, 3).
The preponderance of negative/normal findings on imaging in the present study agrees with some previous studies, especially those in the setting of a normal CBE (9, 17, 20). In this study, 76% of the patients revealed no abnormality on imaging, which is similar to two reports in the USA (77.3% and 75%) (16, 17). On the contrary, in some studies in Nigeria, smaller frequencies (4.7%) were reported (1, 2).
The etiology of mastalgia is not fully understood; however, some reports have demonstrated its association with anxiety, depression, psychosomatic disorders, and high-stress levels (24-26). Moreover, high levels of prolactin and high plasma fatty acids have been introduced as the possible causes of mastalgia, especially in the absence of clinical or radiological findings (27). Other factors associated with breast pain are caffeine and nicotine consumption, lactation frequency, alteration in estrogen/progesterone ratio, oral contraceptives, hormonal therapy, psychotropic drugs, and others (10, 14, 16, 28). Large breasts also cause some degree of ligamentous pain (9). In the aforementioned cases, negative/normal imaging findings are usually observed.
Our study shows that, a majority of the women with positive imaging findings (n = 42, 79.2%) had lesions with BI-RADS II and III assignment, suggesting that most of the patients with painful breast lesions had benign imaging attributes. This finding is some reports in local studies (71.4% (25 out of 35), 98.9% (841 out of 850) and 85% (57 out of 67)), clinically and histologically proving benign diseases in a majority of women presenting with mastalgia (1, 29, 30).
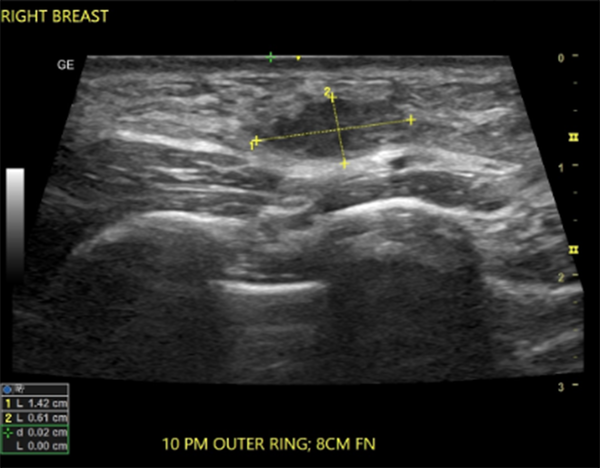
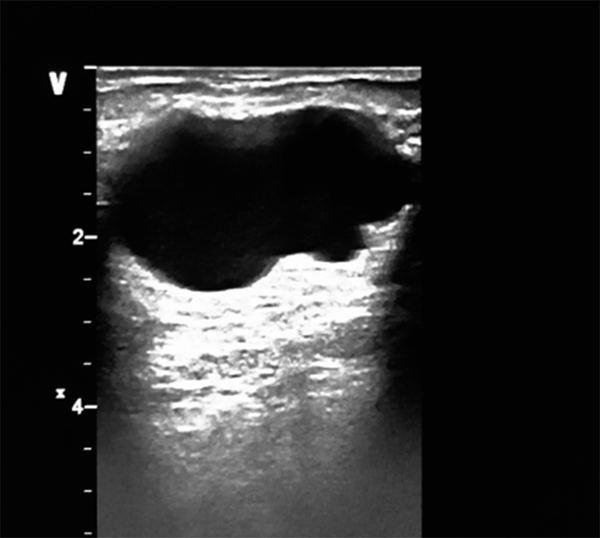
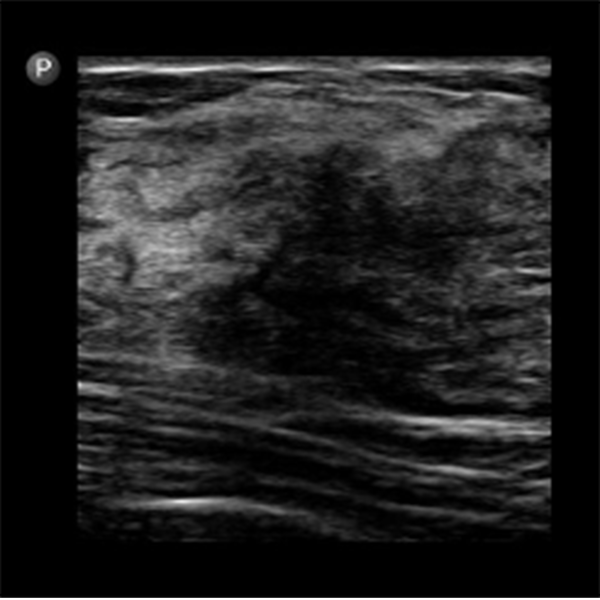
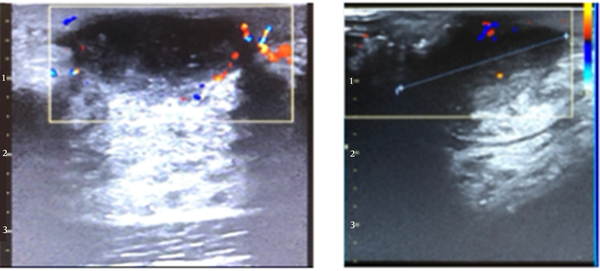
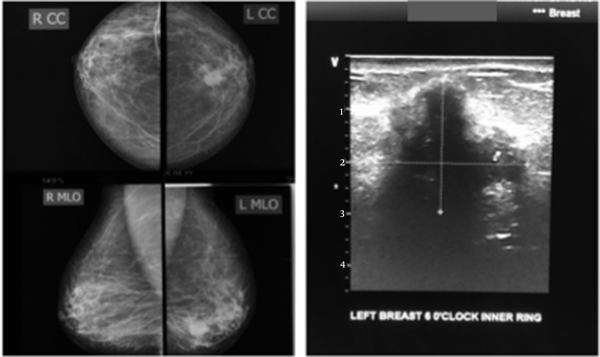
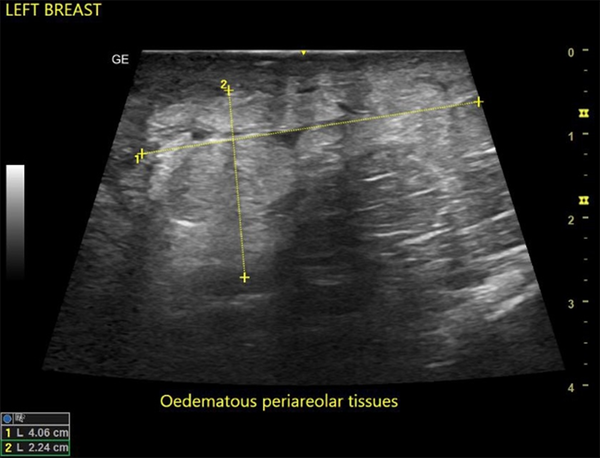
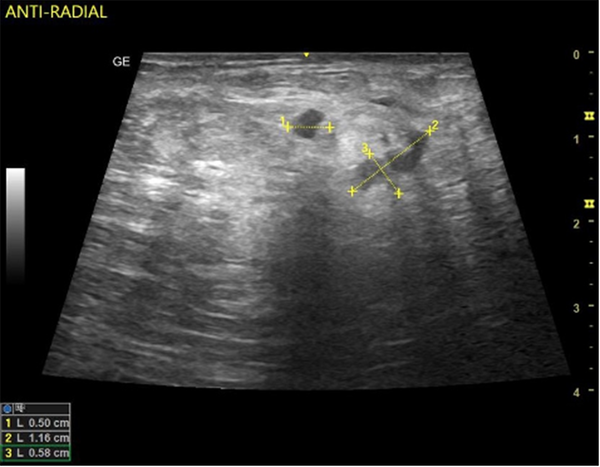
In this study, the predominant imaging diagnosis was fibroadenoma in those with lesions (Figure 1), followed by solitary or multiple simple breast cyst(s) (Figure 2), fibrocystic disease (Figure 3), lactating/nonlactating breast abscesses (Figures 4A and B), and cancer (Figure 5). This finding is in a similar vein with some studies (12, 16) and in contrast with some other studies claiming a fibrocystic change as the most common breast pathology in women with breast pain (1, 2, 29, 31, 32). Interestingly, we observed just one case with a sonological diagnosis of diffuse mastitis, which we assumed was tuberculous, but ended up with a histological diagnosis of breast myxoedema (Figure 6). One patient had a history and sonologic findings suggestive of fat necrosis, which was confirmed at histology after ultrasound-guided core biopsy (Figure 7).
Hypoechoic, wider-than-tall, ellipsoid mass with regular margins; a finding consistent with a fibroadenoma
Simple breast cyst: Anechoic, thin-walled mass demonstrating posterior acoustic enhancement
Ultrasound showing an ill-defined hypoechoic area within the fibroglandular tissue; this case was histologically confirmed as a fibrocystic change.
Breast abscess in a lactating breast (left) and a nonlactating breast (right); ultrasound shows a hypoechoic collection with irregular margins, demonstrating peripheral vascularity on Colour Doppler.
The LCC and LMLO views of the mammogram (left) show an oval dense, bilobed mass with spiculated margins extending into the surrounding tissues; complimentary ultrasound (right) shows a deeply hypoechoic, taller-than-wide mass with irregular margins. Findings are consistent with malignancy. Histology confirmed invasive ductal carcinoma.
Ultrasound shows an ill-defined area of hyperechogenicity (marked by calipers) with intersecting hypoechoic areas. Histology confirmed the myxedema of the breast.
A case of fat necrosis; the patient presented with a painful right breast after sleeping on the bare floor the previous night. Ultrasound showed multifocal irregular hypoechoic foci on a background of echogenic (oedematous) breast tissue. The histology of the core needle biopsy revealed fat necrosis. The symptoms and ultrasound findings were resolved after three weeks.
Reports have also demonstrated a lower risk of breast cancer in women with breast pain, citing frequencies ranging from 0.4 to 0.6% (19, 29, 33). Nine women (3.7%) in our study had BI-RADS V assignments. In previous work on 110 subjects with the breast pain symptoms, no cancer was detected. This, however, may be due to the small sample size of the participants in this study (16). Nevertheless, researchers have demonstrated that cancer prevalence in breast pain ranges from as low as 0.6% and 1.5% (17, 20, 29) to as high as 28.6% (1). The higher frequency is most likely to be attributed to the absence of histopathological confirmation. The cited studies included histopathology outcomes and reported that women with other complaints other than breast pain are more likely to be diagnosed with breast cancer than women with isolated breast pain (30).
No male with breast pain was observed in the present study. This is similar to the findings in Australia (3) and contrary to other studies reporting that 0.6% of the patients were male. It has to be noted, however, that the latter study included other breast complaints besides breast pain (2).
We believe that, despite the negative yields, imaging the painful breast is beneficial. Researchers have noted that the high negative predictive value (NPV) of mammography and sonomammography are quite reassuring not only for the patient but for the managing clinician, even in a setting of a normal CBE (20).
5.1. Conclusions
Imaging, including mammography, and sonomammography, helps confirm or rule out a cause for breast pain. More often than not, there are adverse findings on imaging. Of those that turn out positive, a large majority are benign lesions. Considering the low diagnostic (imaging) yield in patients with mastalgia, there is a need to properly examine and select patients who would likely benefit from imaging, especially those with other symptoms along with breast pain. However, in our environment, where there is still a poor culture of breast screening, this could serve as an opportunity to screen for cancer.
5.2. Limitations of Study
There was no distinction between different forms of breast pain-focal/diffuse and cyclical/non-cyclical as these specific types of pain tend to indicate certain pathologies. Furthermore, the histological diagnosis of the BI-RADS-assigned lesions was not performed for all cases. Moreover, the number of women with breast pain with or without a concomitant breast mass palpated on CBE was not determined.
5.3. Recommendations for Future Studies
Further studies on imaging findings should be followed up with histological diagnosis to reach more comprehensive findings.
References
-
1.
Egwuonwu OA, Anyanwu SN, Chianakwana GU, Ihekwoaba EC. Breast Pain: Clinical Pattern and Aetiology in a Breast Clinic in Eastern Nigeria. Niger J Surg. 2016;22(1):9-11. [PubMed ID: 27013851]. [PubMed Central ID: PMC4785698]. https://doi.org/10.4103/1117-6806.169822.
-
2.
Ohene-Yeboah M, Amaning E. Spectrum of complaints presented at a specialist breast clinic in kumasi, ghana. Ghana Med J. 2008;42(3):110-3. [PubMed ID: 19274109]. [PubMed Central ID: PMC2643436]. https://doi.org/10.4314/gmj.v42i3.43612.
-
3.
Brakohiapa EK, Armah GE, Clegg-Lamptey JN, Brakohiapa WO. Pattern of breast diseases in Accra: review of mammography reports. Ghana Med J. 2013;47(3):101-6. [PubMed ID: 24391224]. [PubMed Central ID: PMC3875282].
-
4.
Okere P, Aderibigbe A, Iloanusi N, Olusina DB, Itanyi D, Okoye I. An audit of the first three years of mammography and sono-mammography at the University of Nigeria Teaching Hospital, Enugu, Nigeria. Journal of College of Medicine. 2013;17(2). https://doi.org/10.4314/jcm.v17i2.5.
-
5.
Barton MB, Elmore JG, Fletcher SW. Breast symptoms among women enrolled in a health maintenance organization: frequency, evaluation, and outcome. Ann Intern Med. 1999;130(8):651-7. [PubMed ID: 10215561]. https://doi.org/10.7326/0003-4819-130-8-199904200-00005.
-
6.
Onukak EE, Cederquist RA. Benign breast disorders in nonwestern populations: Part III--Benign breast disorders in northern Nigeria. World J Surg. 1989;13(6):750-2. [PubMed ID: 2623885]. https://doi.org/10.1007/BF01658427.
-
7.
Tejwani PL, Srivastava A, Nerkar H, Dhar A, Hari S, Thulkar S, et al. Centchroman regresses mastalgia: a randomized comparison with danazol. Indian J Surg. 2011;73(3):199-205. [PubMed ID: 22654331]. [PubMed Central ID: PMC3087062]. https://doi.org/10.1007/s12262-010-0216-z.
-
8.
Carmichael AR. Can Vitex Agnus Castus be Used for the Treatment of Mastalgia? What is the Current Evidence? Evid Based Complement Alternat Med. 2008;5(3):247-50. [PubMed ID: 18830450]. [PubMed Central ID: PMC2529385]. https://doi.org/10.1093/ecam/nem074.
-
9.
Karimian F, Akhavan S, Marzoughi A, Keramati MR, Ashouri M. Correlation between correction of Menstrual Irregularity and Diminution of Cyclic Mastalgia. Journal of Obstetrics, Gynecology and Cancer Research. 2019;4(4):135-40. https://doi.org/10.30699/jogcr.4.4.135.
-
10.
Tahir MT, Shamsudeen S. Mastalgia. StatPearls. Treasure Island (FL); 2022. eng.
-
11.
Schorge J. Breast disease. In: Schorge J, Schaffer J, Harvorson L, et al, editors. Williams Gynecology. 1st ed. New York, USA: Mc Graw Hill Medical; 2008. p. 269-90.
-
12.
Eren T, Aslan A, Ozemir IA, Baysal H, Sagiroglu J, Ekinci O, et al. Factors Effecting Mastalgia. Breast Care (Basel). 2016;11(3):188-93. [PubMed ID: 27493619]. [PubMed Central ID: PMC4960349]. https://doi.org/10.1159/000444359.
-
13.
Salzman B, Fleegle S, Tully AS. Common breast problems. Am Fam Physician. 2012;86(4):343-9. [PubMed ID: 22963023].
-
14.
Iddon J. Mastalgia. In: Dixon JM, editor. ABC of breast disease. 3rd ed. New Jersey, USA: Blackwell Publishing; 2006.
-
15.
Prance SE, Pass HA. Etiology and management of breast pain. In: Singletary SE, Robb GL, Hortobagy GN, editors. Advance Therapy of breast disease. London, England: BC Becker; 2004.
-
16.
Kanat BH, Atmaca M, Girgin M, Ilhan YS, Bozdag A, Ozkan Z, et al. Effects of Mastalgia in Young Women on Quality of Life, Depression, and Anxiety Levels. Indian J Surg. 2016;78(2):96-9. [PubMed ID: 27303116]. [PubMed Central ID: PMC4875894]. https://doi.org/10.1007/s12262-015-1325-5.
-
17.
Tizdast N, Ghazalian F, Gholami M. The Effect of Exercise Type on Inflammatory Markers in Obese Survivors With Breast Cancer: Randomized Control Trial. Health Scope. 2016;5(4). https://doi.org/10.17795/jhealthscope-33421.
-
18.
Howard MB, Battaglia T, Prout M, Freund K. The effect of imaging on the clinical management of breast pain. J Gen Intern Med. 2012;27(7):817-24. [PubMed ID: 22331398]. [PubMed Central ID: PMC3378742]. https://doi.org/10.1007/s11606-011-1982-4.
-
19.
Isfahani P, Arefy M, Shamsaii M. Prevalence of Severe Depression in Iranian Women with Breast Cancer: A Meta-Analysis. Depress Res Treat. 2020;2020:5871402. [PubMed ID: 32455010]. [PubMed Central ID: PMC7240657]. https://doi.org/10.1155/2020/5871402.
-
20.
Tumyan L, Hoyt AC, Bassett LW. Negative predictive value of sonography and mammography in patients with focal breast pain. Breast J. 2005;11(5):333-7. [PubMed ID: 16174154]. https://doi.org/10.1111/j.1075-122X.2005.00018.x.
-
21.
Rosen EL, Sickles E, Keating D. Ability of mammography to reveal nonpalpable breast cancer in women with palpable breast masses. AJR Am J Roentgenol. 1999;172(2):309-12. [PubMed ID: 9930773]. https://doi.org/10.2214/ajr.172.2.9930773.
-
22.
Blue J, Harman J. Mastalgia review: St Marks Breast Centre. N Z Med J. 1998;111(1059):33-4. [PubMed ID: 9506670].
-
23.
Wetzig NR. Mastalgia: a 3 year Australian study. Aust N Z J Surg. 1994;64(5):329-31. [PubMed ID: 8179529]. https://doi.org/10.1111/j.1445-2197.1994.tb02221.x.
-
24.
Johnson KM, Bradley KA, Bush K, Gardella C, Dobie DJ, Laya MB. Frequency of mastalgia among women veterans. Association with psychiatric conditions and unexplained pain syndromes. J Gen Intern Med. 2006;21 Suppl 3:S70-5. [PubMed ID: 16637950]. [PubMed Central ID: PMC1513174]. https://doi.org/10.1111/j.1525-1497.2006.00378.x.
-
25.
Katar MK, Baser M. Relationship Between Mastalgia And Anxiety-Depression: An Observational Study. Cureus. 2021;13(1). e12734. [PubMed ID: 33614336]. [PubMed Central ID: PMC7883554]. https://doi.org/10.7759/cureus.12734.
-
26.
Jaiswal G, Thakur GS. An alternative yogic approach for cyclical mastalgia-A narrative review. J Family Med Prim Care. 2021;10(2):601-8. [PubMed ID: 34041048]. [PubMed Central ID: PMC8138339]. https://doi.org/10.4103/jfmpc.jfmpc_1688_20.
-
27.
Çakir T, Cİngİ A, Nurhan F, Bez Y, Topçuoğlu V, Güllüoğlu BM. [The place of suggestion in patients with mastalgia without an organic cause A prospective cross-sectional study]. J Breast Health. 2006;2(2):96-9. Turkish.
-
28.
Ader DN, South-Paul J, Adera T, Deuster PA. Cyclical mastalgia: prevalence and associated health and behavioral factors. J Psychosom Obstet Gynaecol. 2001;22(2):71-6. [PubMed ID: 11446156]. https://doi.org/10.3109/01674820109049956.
-
29.
Ohene-Yeboah M. Breast pain in Ghanaian women: clinical, ultrasonographic, mammographic and histological findings in 1612 consecutive patients. West Afr J Med. 2008;27(1):20-3. [PubMed ID: 18689298].
-
30.
Chiedozie LC, Guirguis MN. Mastalgia and breast tumour in Nigerian women. West Afr J Med. 1990;9(1):54-8. [PubMed ID: 2271423].
-
31.
Brkic M, Vujovic S, Ivovic M, Tancic Gajic M, Marina L, Franic Ivanisevic M, et al. The Role of E2/P Ratio in the Etiology of Fibrocystic Breast Disease, Mastalgia and Mastodynia. Acta Clin Croat. 2018;57(4):756-61. [PubMed ID: 31168213]. [PubMed Central ID: PMC6544108]. https://doi.org/10.20471/acc.2018.57.04.18.
-
32.
Stachs A, Stubert J, Reimer T, Hartmann S. Benign Breast Disease in Women. Dtsch Arztebl Int. 2019;116:565-74. https://doi.org/10.3238/arztebl.2019.0565.
-
33.
Khan SA, Apkarian AV. Mastalgia and breast cancer: a protective association? Cancer Detect Prev. 2002;26(3):192-6. [PubMed ID: 12269765]. https://doi.org/10.1016/s0361-090x(02)00065-x.