Abstract
Background:
Malnutrition and failure to thrive (FTT) is a delay or a halt in children’s growth, which leads to serious compilations if it is left untreated. Malnutrition due to its prevalence is the most important nutritional disease in developing countries and has the most prevalence among infants and preschool children. This study aimed at rating and determining the effective factors of malnutrition incidence and growth delay among 0 to 24 months children.Methods:
To identify children under 2 years of age, we referred to health centers and health stations in the city of Shahroud (Northeast of Iran) in 2015. Using cluster sampling, 706 children were surveyed. Anthropometric indices with international reference standards were compared. The values obtained for less than 2 standard deviations as stunting, underweight, wasting, and FTT were defined. All statistical analyses were performed using SPSS software with significance level set at 0.05.Results:
The results indicated the existence of malnutrition in the region. Based on the findings, the percentage of underweight, wasting, stunting and ratio of head circumference with age was determined to be 1.7%, 5.4%, 9.5%, and 8.6%, respectively; and considering the category of growth disorder, Type 1, 2, and 3 were, respectively, 1.7%, 5.2% and 3.1%. Factors affecting malnutrition included age, birth weight, birth spacing, and the mother’s BMI at child birth.Conclusions:
Tracking the status of children with growth disorder and malnutrition, offering appropriate interventions, considering the nutrition status of mothers during pregnancy, and providing appropriate nutritional counseling are of prime importance to attend to this problem.Keywords
Failure to Thrive Malnutrition Children Under the Age of Two Iran
1. Background
Malnutrition is considered to be the most important nutritional disease in developing countries mainly due to its high prevalence and relationship with high levels of mortality among children (1). This disease can be considered as an indicator of a society’s social and economic status. About 70% of the children suffering from malnutrition live in Asia, among which the highest prevalence rate of malnutrition is related to infants and preschoolers (2). During the first 2 years of life, which is accompanied with quick physical and social development, many changes occur in an infant’s nutrition and nutrient intake. Healthy and well-fed infants have enough energy to respond to and learn from the environmental stimuli; in fact, they are able to make better contact with their parents (3). The evaluation of nutritional status is one of the most important fundamental principles of global strategy to prevent malnutrition and raise the infant’s level of health; this is, in fact, an important way to find people in societies or groups whose growth does not conform to the considered pattern (4, 5). Failure to thrive, particularly due to malnutrition, can be generally seen in children under the age of 5; in this regard, the most common age in which this issue interferes with the growth of children is between 6 and 12 months (6). Over the last decades, researchers have worked on finding the causes and appropriate interventional guidelines for malnutrition. So far, it has been shown that the issue of malnutrition is multidimensional and its causes are complicated and interrelated (6, 7).
Although a decrease in the percentage of children suffering from malnutrition has been mentioned in previous studies around the globe, this issue is still an important interventional priority; in other words, the factors affecting children’s nutritional status in 1 region apparently differ from those of another region. Malnutrition has multiple causes, and identifying the causative factors or increasing factors is the first step to solving this problem (8, 9).
The studies conducted previously in this field showed that specific factors including insufficient nutrient intake, inappropriate diet of children, and infectious diseases (e.g., fever and diarrhea, parents’ education, parents’ occupation, and family size) are the most important factors in the incidence of FTT. So far, researchers have been mostly concerned with the health of children under the age of 6. Because the first 2 years of life are of considerable importance for children’s development and growth, focusing on this period of life to find the causative factors of malnutrition can be a big step forward in preventing failure to thrive.
2. Objectives
The present study aimed at investigating the causative factors of malnutrition and failure to thrive in children under the age of 2 in Shahroud, Iran, in 2015.
3. Methods
This was a descriptive-analytical and cross-sectional study. In this study, 706 out of a total population of 4300 children younger than 2 years of age were selected using proportional cluster method from 13 health centers and 4 health stations in Shahroud, Iran. The selected children had active health files in the health centers.
To collect the required data for this work, a self-administered questionnaire was applied. The questionnaires were administered by the principal investigator in a face to face interview with the children’s mothers. Using SPSS software, the data were analyzed through statistical Chi-square test and independent t-test. The nutritional status of children was measured based on the anthropometric method. Weight was measured by a digitally scaled device (Seca, Germany) specified for children with minimal clothing, and with an accuracy of 0.01. In addition, height was measured horizontally using a special height measuring box; the child’s head was held at the end of the box, while her knees were held horizontally flat with the pressure of hands. Then, the moving plate was moved in a way to make a tangent line with the child’s heels. Furthermore, a non-elastic tape was used to measure the head circumference. In this study, the standard deviation means of weight for age, height for age, weight for height, and head circumference for age were calculated and compared according to the international reference values of national center for health statistics (NCHS) (10, 11). The values less than 2 standard deviations were defined as underweight, wasting, stunting, and failure to thrive. FTT types were also determined and categorized into the following categories:
- Type 1 FTT: Underweight, but with normal head circumference
- Type 2 FTT: Normal head circumference, but with proportionally reduced weight and height
- Type 3 FTT: Below normal head circumference, with proportionally reduced weight and height
In failure to thrive, weight reduces at first, followed by a reduction in height and head circumference. Failure to thrive, known also as developmental delay, means gradual reduction of development rate in an established pattern. This is of high importance because of its disruptive effects on the child’s health and growth, and also because it may cause other complications. The data were analyzed using descriptive statistics, Chi-square test. Furthermore, Epi-Info Software V 2006 was applied to determine anthropometric indices.
The parents or child legal guardian were informed about the study goals, and verbal consent was obtained to take their child’s anthropometric measurements. Inclusion criteria were healthy children aged > 2 years; and those children who had infection, metabolic, congenital, and chronic diseases were excluded from the study.
The questionnaire included the following information: the child’s age; gender; child birth weight; birth interval; family size; parental education and occupation; factors related to the mother; acute respiratory infection (ARI); diarrhea in the last 2 weeks; breastfeeding; the kind of complementary feeding; birth weight; parasite; visiting health centers for care; and order of live birth.
4. Results
In the present study, 706 children were studied for malnutrition and failure to thrive. Table 1 demonstrates the nutritional status of these children. As displayed in the table, the prevalence of underweight, stunting, wasting, and head circumference was 5.9%, 7.1%, 4.5%, and 6.8%, respectively.
Prevalence of Underweight, Stunting, Wasting, and Head Circumference According to Age (Shahroud, Iran, 2015)a,b
| Nutritional Statues for Age | Wt./Age | H t/Age | Wt./H t | Head circ./Age | ||||
|---|---|---|---|---|---|---|---|---|
| Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | |
| < 6 | 158 (99.4) | 1 (0.6) | 156 (98.1) | 3 (1.9) | 158 (99.4) | 1 (6) | 147 (92.5) | 12 (7.5) |
| 6 - 12 | 196 (94.2) | 12 (5.8) | 194 (93.3) | 14 (6.6) | 198 (95.2) | 10 (4.8) | 192 (92.3) | 16 (7.5) |
| ≥ 12 | 302 (89.1) | 37 (10.9) | 314 (92.6) | 25 (7.4) | 318 (93.8) | 21 (6.2) | 314 (94) | 20 (6) |
| Total | 656) 92.9) | 50 (7.1) | 664 (94.1) | 42 (5.9) | 674 (95.5) | 32 (4.5) | 653 (93.2) | 48 (6.8) |
| P value | 0.000c | 0.046c | 0.020c | 0.690 | ||||
A significant relationship was found between (underweight) weight for age (P < 0.001), (stunting) height for age (P < 0.046), and (wasting) weight for height (P < 0.020) and age. Figure 1 displays the types of developmental delay in the participants under FTT study. Considering the abovementioned categories for FTT, 1.7%, 2.5%, and 1.3% of the children studied in this work fell into the Types 1, 2, and 3 FTT, respectively (Figure 1).
Types of Developmental Delay in the Participants Under FTT Study
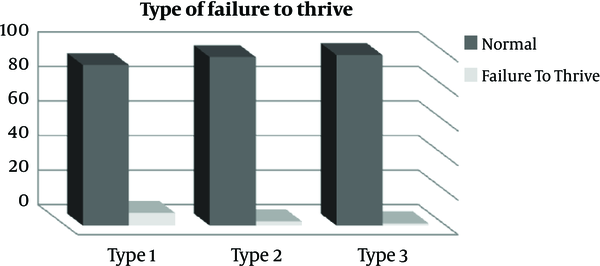
Table 2 presents the classification of nutritional status indexes of present and past, past, present, and head circumference of children younger than 2 years according to their gender.
The Prevalence of Underweight, Stunting, Wasting, and Head Circumference According to Gender (Shahroud, Iran)a
| Variable | No. (%) | WA/Underweight | HA/A Stunting | W/H Wasting | Head Circumference | ||||
|---|---|---|---|---|---|---|---|---|---|
| Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | ||
| Child’s gender | |||||||||
| Female | 326 (46.2) | 302 (92.6) | 24 (7.4) | 311 (95.4) | 15 (4.6) | 311 (95.4) | 15 (4.6) | 305 (94.7) | 17 (5.3) |
| Male | 380)53.8) | 354 (93.2) | 26 (6.8) | 535 (92.9) | 27 (7.1) | 363 (95.5) | 17 (4.5) | 348 (91.8) | 31 (8.2) |
| Total | 706 (100) | 656 (92.9) | 50 (7.1) | 664 (94.1) | 42 (5.9) | 674 (96.5) | 32 (4.5) | 653 (93.2) | 48 (6.8) |
| P value | 0.788 | 0.161 | 0.935 | 0.130 | |||||
From the statistical point of view, no significant relationship was obtained between all nutritional status indices with parents’ education and occupation, and family size (Table 3). However, a significant relationship was observed between mothers’ BMI and malnutrition at the present time and those of the past time. No significant relationship was found between mothers’ age and height and the children’s nutritional status and all the anthropometric indices. Moreover, no significant statistical difference was obtained between mothers’ BMI index, malnutrition in the past and present, and children’s head circumference. The results revealed that 6.8% of the mothers had anemia because of low levels of hemoglobin, but no significant relationship was found between mothers’ nutritional status and anemia (Table 4).
The Nutritional Status of Children According to Some of Social and Economic Factors (Shahroud, Iran, 2015)
| Variable | No. (%) | WA/Underweight | HA/A Stunting | W/H Wasting | Head Circumference | ||||
|---|---|---|---|---|---|---|---|---|---|
| Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | ||
| Mother’s education | |||||||||
| Illiterate | 4 (0.65) | 4 (100.0) | 0 (0) | 4 (100.0) | 0 (0.0) | 4 (100.0) | 0 (0) | 3 (75.0) | 1 (25.0) |
| Primary | 59 (6.8) | 57 (96.6) | 1 (1.7) | 55 (93.2) | 4 (6.8) | 58 (98.3) | 1 (1.7) | 56 (94.9) | 3 (5.1) |
| Guidance | 12 (17.4) | 85 (91.4) | 5 (5.4) | 87 (93.5) | 6 (6.5) | 88 (94.6) | 5 (5.4) | 89 (95.7) | 4 (4.3) |
| High schooland higher | 520 (52.45) | 506 (92.7) | 26 (4.7) | 517 (94.0) | 32 (5.8) | 523 (95.5) | 26 (4.7) | 504 (92.6) | 40 (7.4) |
| Total | 706 (100) | 655 (92.9) | 32 (4.5) | 663 (94.0) | 42 (6.0) | 673 (95.5) | 32 (4.5) | 652 (93.1) | 48 (6.9) |
| P value | 0.596 | 0.944 | 0.684 | 0.319 | |||||
| Father’s education | |||||||||
| Illiterate | 8 (1.1) | 7 (87.5) | 1 (12.5) | 8 (100.0) | 0 (0) | 8 (100.1) | 0 (0.0) | 8 (100.0) | 0 (0.0) |
| Primary | 48 (8.6) | 46 (95.8) | 2 (4.2) | 45 (93.8) | 3 (6.3) | 48 (100.0) | 0 (0.0) | 44 (91.7) | 4 (8.3) |
| Guidance | 123 (17.4) | 109 (88.6) | 14 (11.4) | 110 (89.4) | 13 (10.6) | 118 (95.9) | 5 (4.1) | 115 (93.5) | 8 (6.5) |
| Hgh schooland higher | 527 (74.7) | 493 (93.7) | 33 (6.3) | 500 (95.1) | 26 (4.9) | 499 (94.9) | 27 (5.1) | 485 (93.1) | 36 (6.9) |
| Total | 706 (100) | 655 (92.9) | 50 (7.1) | 663 (94.0) | 42 (6.0) | 673 (95.5) | 32 (4.5) | 652 (93.1) | 48 (6.9) |
| P value | 0.176 | 0.105 | 0.368 | 0.854 | |||||
| Father’s job | |||||||||
| Un employed | 6 (0.8) | 6 (100.0) | 0 (0.0) | 6 (100.0) | 0 (0.0) | 6 (100.0) | 0 (0.0) | 5 (83.3) | 1 (16.7) |
| Have a job | 700 (94) | 647 (92.8) | 50 (7.2) | 655 (94.0) | 42 (6.0) | 665 (95.4) | 32 (4.6) | 645 (93.2) | 47 (6.8) |
| Total | 706 (100) | 653 (92.9) | 50 (7.1) | 661 (94.0) | 42 (6.0) | 671 (95.4) | 32 (4.6) | 650 (93.1) | 48 (6.9) |
| P value | 0.591 | 0.535 | 0.591 | 0.341 | |||||
| Mother’s job | |||||||||
| Housewife | 658 (93.2) | 564 (92.9) | 43 (7.1) | 570 (93.9) | 37 (6.1) | 580 (95.6) | 27 (4.4) | 560 (92.9) | 43 (7.1) |
| Have a job | 48 (6.8) | 88 (92.6) | 7 (7.4) | 90 (94.7) | 5 (5.3) | 90 (94.7) | 5 (5.3) | 89 (94.7) | 5 (5.3) |
| Total | 706 (100) | 652 (92.9) | 50 (7.1) | 660 (94.0) | 42 (6.0) | 670 (95.4) | 32 (4.6) | 649 (93.1) | 48 (6.9) |
| P value | 0.920 | 0.750 | 0.723 | 0.519 | |||||
| Family size | |||||||||
| = 3 | 377 (53.4) | 349 (92.6) | 28 (7.4) | 358 (95.0) | 19 (5.0) | 356 (94.4) | 21 (5.6) | 350 (93.6) | 24 (6.4) |
| 4 | 274 (35) | 231 (93.5) | 16 (6.5) | 228 (92.3) | 19 (7.7) | 240 (97.2) | 7 (2.8) | 228 (92.7) | 18 (7.3) |
| ≥ 5 | 55 (11.6) | 70 (94.6) | 4 (5.4) | 71 (95.9) | 9 (4.1) | 71 (95.9) | 3 (4.1) | 68 (93.2) | 5 (6.8) |
| Total | 706 (100) | 650 (93.1) | 48 (6.9) | 657 (94.1) | 41 (5.9) | 667 (95.6) | 31 (4.4) | 646 (93.2) | 47 (6.8) |
| P value | 0.783 | 0.302 | 0.264 | 0.909 | |||||
The Nutritional Status of Children With Respect to Factors Related to Mothers (Shahroud, Iran, 2015)
| Variable | No. (%) | WA/Underweight | HA/A Stunting | W/H Wasting | Head Circumference | ||||
|---|---|---|---|---|---|---|---|---|---|
| Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | ||
| Height’ mother | |||||||||
| < 150 | 42 (5.9) | 44 (91.7) | 4 (8.3) | 46 (95.8) | 2 (4.2) | 45 (93.8) | 3 (6.3) | 46 (95.8) | 2 (4.2) |
| 150 - 160 | 258 (36.5) | 168 (93.9) | 11 (6.1) | 169 (94.4) | 10 (5.6) | 168 (93.9) | 11 (6.1) | 168 (93.9) | 11 (6.1) |
| > 160 | 405 (57.4) | (92.3) | 33 (7.7) | 403 (93.5) | 28 (6.5) | 418 (97.0) | 13 (3.0) | 394 (92.5) | 32 (7.5) |
| Total | 705 (99.9) | 610 (92.7) | 48 (7.3) | 618 (93.9) | 40 (6.1) | 631 (95.9) | 27 (4.1) | 608 (93.1) | 45 (6.9) |
| P value | 0.773 | 0.775 | 0.153 | 0.617 | |||||
| BMI’ mother | |||||||||
| -> 19 | 23 (3.3) | 18 (78.3) | 5 (21.7) | 20 (87.0) | 3 (13.0) | 20 (87.0) | 3 (13.0) | 20 (87.0) | 3 (13.0) |
| 19 - 24.99 | 309 (43.7) | 285 (93.1) | 21 (6.9) | 286 (93.5) | 20 (6.5) | 291 (95.1) | 15 (4.9) | 282 (92.8) | 22 (7.2) |
| 25 - 29.99 | 261 (37) | 241 (92.3) | 20 (7.7) | 248 (95.0) | 13 (5.0) | 250 (95.8) | 11 (4.2) | 242 (93.4) | 17 (6.6) |
| ≥30 | 113 (16) | 109 (96.5) | 4 (3.5) | 107 (94.0) | 6 (5.3) | 110 (97.3) | 3 (2.7) | 106 (94.6) | 6 (5.4) |
| Total | 706 (100) | 653 (92.9) | 50 (7.1) | 661 (94.0) | 42 (6.0) | 671 (95.4) | 32 (4.6) | 650 (93.1) | 48 (6.9) |
| P value | 0.021 | 0.429 | 0.179 | 0.600 | |||||
| HB mother | |||||||||
| < 11 | 48 (7.3) | 44 (91.7) | 4 (8.3) | 46 (95.8) | 2 (4.2) | 45 (93.8) | 3 (6.3) | 46 (95.8) | 2 (4.2) |
| 11 - 12 | 179 (27.2) | 168 (93.9) | 11 (6.1) | 169 (94.4) | 10 (5.6) | 168 (93.9) | 11 (6.1) | 168 (93.9) | 11 (6.1) |
| > 12 | 431 (65.5) | 398 (92.3) | 33 (7.7) | 403 (93.5) | 28 (6.5) | 418 (97.0) | 13 (3.0) | 394 (92.5) | 32 (7.5) |
| Total | 658 (100) | 610 (92.7) | 48 (7.3) | 618 (93.9) | 40 (6.1) | 631 (95.9) | 27 (4.1) | 608 (93.1) | 45 (6.9) |
| P value | 0.775 | 0.773 | 0.153 | 0.617 | |||||
Considering children’s nutritional factors, no significant statistical relationship was observed between height for age, weight for height, weight for age, head circumference for age and breastfeeding, the first supplementary food, and the type of staple food up to the age of 1. Considering the children’s non-nutritional factors, including birth rank, respiratory infections, diarrhea in the past 2 weeks, and the existence of parasites, no relationship was found between these factors. However, a significant relationship was obtained between weight for age (P < 0.038), weight for height (P = 0.049), and birth interval. Table 5 demonstrates some nutritional and non-nutritional factors in children (SD classification). The results also revealed a significant relationship between weight for age, head circumference for weight, and birth weight (P < 0.001).
The Nutritional Status of Children With Respect to Some Variables (Shahroud, Iran, 2015)
| Variable | No. (%) | WA/Underweight | HA/A Stunting | W/H Wasting | Head Circumference | ||||
|---|---|---|---|---|---|---|---|---|---|
| Norma | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | Normal | Malnutrition | ||
| Order birth | |||||||||
| 1 | 377 (53.4) | 394 (92.6) | 28 (7.4) | 358 (95.0) | 19 (5.0) | 356 (94.4) | 21 (5.6) | 349 (93.3) | 25 (6.7) |
| 2 | 245 (36) | 236 (92.9) | 18 (7.4) | 235 (92.5) | 19 (7.5) | 246 (96.9) | 8 (3.1) | 235 (92.9) | 18 (7.1) |
| ≥ 3 | 70 (9.9) | 66 (94.3) | 4 (5.7) | 67 (95.7) | 3 (4.3) | 67 (95.7) | 3 (4.3) | 65 (94.2) | 4 (5.8) |
| Total | 651 (92.9) | 50 (7.1) | 660 (94.2) | 41 (5.8) | 669 (95.4) | 32 (4.6) | 649 (93.2) | 47 (6.8) | |
| P value | 0.877 | 0.37 | 0.358 | 0.925 | |||||
| Acute respiratory infection in last two weeks (ARI) | |||||||||
| Yes | 1 (0.1) | 648 (93.0) | 49 (7.0) | 1 (100.0) | 42 (6.0) | 666 (95.6) | 31 (4.4) | 645 (93.2) | 47 (6.8) |
| No | 705 (99.9) | 1 (100.0) | 0 (0.0) | 655 (94.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) |
| Total | 706 (100) | 649 (93.0) | 49 (7.0) | 656 (94.0) | 42 (6.0) | 667 (95.6) | 31 (4.4) | 646 (93.2) | 47 (6.8) |
| P value | 0.783 | 0.800 | 0.829 | 0.787 | |||||
| Diarrhea in the last two weeks | |||||||||
| Yes | 169 (32.9) | 499 (93.6) | 34 (6.4) | 505 (94.7) | 28 (5.3) | 508 (95.3) | 25 (4.7) | 491 (92.8) | 38 (7.2) |
| No | 533 (75.5) | 153 (90.5) | 16 (9.5) | 155 (91.7) | 14 (8.3) | 162 (95.9) | 7 (4.1) | 159 (94.6) | 9 (5.4) |
| Total | 702 (100) | 652 (92.9) | 50 (7.1) | 660 (94.0) | 42 (6.0) | 670 (95.4) | 32 (4.6) | 650 (93.3) | 47 (6.7) |
| P value | 0.174 | 0.148 | 0.766 | 0.411 | |||||
| Breastfeeding, mo | |||||||||
| Yes | 700 (99) | 572 (92.4) | 47 (7.6) | 579 (93.5) | 40 (6.5) | 590 (95.3) | 29 (4.7) | 575 (92.9) | 44 (7.1) |
| No | 6 (1) | 8 (100.0) | 0 (0.0) | 8 (100.0) | 0 (0.0) | 8 (100.0) | 0 (0.0) | 7 (87.5) | 1 (12.5) |
| Total | 706 (100) | 580 (92.5) | 47 (7.5) | 587 (93.6) | 40 (6.4) | 598 (95.4) | 29 (4.6) | 582 (92.8) | 45 (7.2) |
| P value | 0.418 | 0.457 | 0.531 | 0.557 | |||||
| Brith interval, mo | |||||||||
| Frist | 425 (60.2) | 393 (55.6) | 32 (4.53) | 402 (56.94) | 23 (3.25) | 401 (56.7) | 24 (3.4) | 393 (55.6) | 29 (4.1) |
| < 36 | 37 (5.2) | 232 (32.9) | 12 (1.7) | 227 (39.23) | 17 (2.4) | 239 (33.8) | 5 (0.7) | 228 (32.3) | 14 (1.98) |
| ≥ 36 | 244 (34.6) | 31 (4.4) | 6 (0.85) | 35 (4.95) | 2 (0.3) | 34 (4.81) | 3 (0.42) | 32 (4.53) | 5 (0.7) |
| Total | 706 (100) | 656 (92.9) | 50 (7.08) | 664 (94.05) | 42 (5.6) | 674 (95.4) | 32 (4.53) | 653 (92.4) | 48 (6.84) |
| P value | 0.038a | 0.708 | 0.049a | 0.222 | |||||
5. Discussion
The results of the present study showed malnutrition and failure to thrive among the studied children. In a study conducted by Emamian et al., on children under the age of 5 in the same region as this study, the percentage of underweight, wasting, and stunting was reported to be 7.7%, 4.5%, and 10.3%, respectively (12). Comparing the FTT recorded at the present with that of the past, it was found that FTT has not changed. Considering this, it can be implied that appropriate intervention should have at least reduced wasting. One of the reasons for this could be a failure to provide primary health care services in the urban areas. Because weight for height represents a failure to thrive in the present, these results could be justified based on differences of age groups and the importance of family nutrition after weaning. Therefore, it can be implied that cooking and food preparation, family food security and attention to local foods are of particular importance. In a study conducted by Al-Zuheiry et al., in Kanaan, Diyale Province, Iraq, most of the cases of failure to thrive in relation to body weight were found to be mild (80.8%), whereas its moderate cases were 19.2%. Their study concluded that FTT is common in Iraq (8). Compared with the results of the mentioned study, the children studied here had a better status. Namakin et al. studied children under the age of 2 in the Southeast of Iran; based on their reports, the 3 types of FTT, as mentioned above were6.5%, 37.3%, and 1%, respectively. Based on the results of the present study, the children in Shahroud region were of better health in stunting compared with the group of children from the study conducted by Namakin et al. This can be considered as the representative of the nutritional status during pregnancy and mothers’ BMI; in fact, this is one of the efficient factors affecting children’s nutritional status. In this regard, the result of the present study is consistent with that reported by Namakin et al. (13). In 1998, a national study was conducted on children under the age of 5 with the aim of evaluating malnutrition and failure to thrive among these children. According to the reports of that study, stunting, underweight, and wasting for the children of Semnan, Iran, were 3.7%, 6.5%, and 1%, respectively. In comparison with the results of the present study, children’s status has worsened from 1998 to 2015. However, this is still of better status compared with the status of the children from Cameroon, Peru, and Haiti (5, 14-16). In addition, the malnutrition status of children in Shahroud in the present time was found to be in a more unfavorable position than those from poor regions of China (17). Furthermore, in a meta-analysis study on Indian children, all anthropometric indices indicated an unfavorable position for children in this region (18). The results of most studies conducted in this field represent high levels of chronic malnutrition among children, which is of high concern and should be taken into account.
Stunting is still one of the main problems found in almost all societies (4, 19). Based on the results, stunting was found to be reduced over time in children. Anthropometric indices are among the common indices used to evaluate nutritional status. To appropriately assess the anthropometric status of the society, 3 indices should be simultaneously taken into account. Underweight is sometimes accompanied with wasting and sometimes with stunting or with both. In a short child, weight may be suitable for height, but it is inappropriate for age. However, it is possible for the child to have misleading fitness and malnutrition, or other past diseases could have caused his or her height to be shorter than expected. On the other hand, a child with favorable height for age may have a lower than expected weight because of malnutrition or past diseases. In fact, none of these children have a suitable weight for age. Currently, treatment is started after malnutrition is found among children through monitoring. There is also another way to further advance the current regulations by replacing the intervention of malnutrition treatment with preventing treatment. In other words, this replacement can be done by emphasizing to weight the child in the interval between the two due weighing times instead of measuring suitable weight for age at a specified time.
It was found that the status of the males is better than the females in malnutrition, but it was not found to be statistically significant. This result is in line with that of Emamian et al., and inconsistent with the report of Wamani et al. (12, 20). The results of better anthropometric indices could be attributed to the higher literacy of parents compared with the past and the existence of health facilities. There was a significant relationship between mothers’ BMI and weight for age in this study. However, what is notable about mothers’ BMI was their nutrition quality and quantity because fatness and overweight cases were found in the study and this could affect the birth weight; this finding is consistent with that of other studies (21). In the present study, 4.4% of children weighed less than 2500 grams at birth, and a significant relationship was seen between birth weight and height for age, weight for age, and head circumference for age. However, no significant relationship was found between parents’ literacy, parents’ occupation, and even suffering from an acute respiratory infection in the past weeks and the nutritional status of children in this study, which can represent a growing trend in developing societies and more appropriate access to primary health services.
Birth interval can be a contributing factor affecting malnutrition in the present and past. In this study, 5.2% of children had a birth interval less than 36 months and this had a significant relationship with weight for age and weight for height, with P = 0.038 and P = 0.049, respectively. A study in the rural areas of Saudi Arabia is among the studies referring to the significant effects of child birth order on malnutrition (22). Providing postdelivery consultations to observe pregnancy spacing is one of the most important duties of health and media staff.
In the present study, a significant relationship was observed between the child’s age and malnutrition. This finding is in agreement with that of some of the world and Iran’s studies. The maximum age of malnutrition in this study was between 1 and 2 years. It seems that the risk and level of malnutrition in children increase as they age. Among the studies conducted on the effects of growing up on the child’s malnutrition, we can refer to Martorell et al. study that found the maximum malnutrition at the age of 1 to 2 years and the minimum malnutrition at the age of 0 to 5 months (23). These results reveal the importance of breastfeeding, supplementary feeding, and suitability of family food for children.
5.1. Conclusion
The results of the present study revealed the existence of malnutrition and failure to thrive among children under the age of 2 in Shahroud, Iran. Age, birth interval, and mothers’ body mass index were some of the factors affecting nutritional status. Thus, conducting studies on this subject still seems necessary. Following the status of children suffering from failure to thrive and malnutrition, making appropriate interventions, paying attention to the nutritional status of mothers during pregnancy, and providing suitable nutritional consultants are obligatory. Taking quick action on interventional educational programs, paying attention to appropriate nutritional educational programs suitable for pregnancy, proper birth spacing, following malnourished people and supporting them while planning the programs are the ways by which malnutrition can be controlled.
Acknowledgements
References
-
1.
Pawenrusi EP. Factors related to the nutritional status of children in area served by the pattingalloang health center, makassar. Pakistan J Nutr. 2016;15(4):333-6. https://doi.org/10.3923/pjn.2016.333.336.
-
2.
Khor GL. Update on the prevalence of malnutrition among children in Asia. Nepal Med Coll J. 2003;5(2):113-22. [PubMed ID: 15024783].
-
3.
Trahms CM,, McKean KN. Mahan LK, Escott-Stump S, editors. Nutrition during infancy. 13th ed. USA: WB Saunders Company: Krause's Food Nutrition Therapy; 2008. 375 p.
-
4.
de Onis M, Blossner M, Borghi E, Morris R, Frongillo EA. Methodology for estimating regional and global trends of child malnutrition. Int J Epidemiol. 2004;33(6):1260-70. [PubMed ID: 15542535]. https://doi.org/10.1093/ije/dyh202.
-
5.
Johnson W. Analytical strategies in human growth research. Am J Hum Biol. 2015;27(1):69-83. [PubMed ID: 25070272]. https://doi.org/10.1002/ajhb.22589.
-
6.
Wilcox WD, Nieburg P, Miller DS. Failure to thrive. A continuing problem of definition. Clin Pediatr (Phila). 1989;28(9):391-4. [PubMed ID: 2670392]. https://doi.org/10.1177/000992288902800901.
-
7.
Wright CM. Identification and management of failure to thrive: a community perspective. Arch Dis Child. 2000;82(1):5-9. [PubMed ID: 10630901]. https://doi.org/10.1136/adc.82.1.5.
-
8.
Al-Zuheiry MSH. The rate of failure to thrive among children aged 2 months - 5 years in Kanaan sub-district / Diyala province. Diyala J Appl Res. 2009;5(1):16-21.
-
9.
Ministry of Health and Medical Education and UNICEF. The nutritional status of children. Tehran: Ministry of Health and Medical Education and UNICEF; 2000.
-
10.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1-190. [PubMed ID: 12043359].
-
11.
Measuring changes in nutritional status. Geneva: WHO; 1983. p. 19-28.
-
12.
Emamian MH, Gorgani N, Fateh M. Malnutrition status in children of Shahroud, Iran [In Persian]. J Knowledge Health. 2011;6(1):7-14.
-
13.
Namakin K, Sharifzadeh GR, Zardast M, Khoshmohabbat Z, Saboori M. Comparison of the WHO Child Growth Standards with the NCHS for Estimation of Malnutrition in Birjand-Iran. Int J Prev Med. 2014;5(5):653-7. [PubMed ID: 24932399].
-
14.
Kavosi E, Hassanzadeh Rostami Z, Kavosi Z, Nasihatkon A, Moghadami M, Heidari M. Prevalence and determinants of under-nutrition among children under six: a cross-sectional survey in Fars province, Iran. Int J Health Policy Manag. 2014;3(2):71-6. [PubMed ID: 25114945]. https://doi.org/10.15171/ijhpm.2014.63.
-
15.
Nagahori C, Tchuani JP, Yamauchi T. Factors associated with nutritional status in children aged 5-24 months in the Republic of Cameroon. Nurs Health Sci. 2015;17(2):229-35. [PubMed ID: 25818304]. https://doi.org/10.1111/nhs.12176.
-
16.
Rollet SR, Gray ES, Previl H, Forrester JE. Prevalence of malnutrition in children under five and school-age children in Milot Valley, Haiti. Public Health. 2014;128(12):1094-8. [PubMed ID: 25454253]. https://doi.org/10.1016/j.puhe.2014.10.002.
-
17.
Wang X, Hojer B, Guo S, Luo S, Zhou W, Wang Y. Stunting and 'overweight' in the WHO Child Growth Standards - malnutrition among children in a poor area of China. Public Health Nutr. 2009;12(11):1991-8. [PubMed ID: 19656437]. https://doi.org/10.1017/S1368980009990796.
-
18.
Sahu SK, Kumar SG, Bhat BV, Premarajan KC, Sarkar S, Roy G, et al. Malnutrition among under-five children in India and strategies for control. J Nat Sci Biol Med. 2015;6(1):18-23. [PubMed ID: 25810629]. https://doi.org/10.4103/0976-9668.149072.
-
19.
Keino S, Plasqui G, Ettyang G, van den Borne B. Determinants of stunting and overweight among young children and adolescents in sub-Saharan Africa. Food Nutr Bull. 2014;35(2):167-78. [PubMed ID: 25076764]. https://doi.org/10.1177/156482651403500203.
-
20.
Wamani H, Astrom AN, Peterson S, Tumwine JK, Tylleskar T. Boys are more stunted than girls in sub-Saharan Africa: a meta-analysis of 16 demographic and health surveys. BMC Pediatr. 2007;7:17. [PubMed ID: 17425787]. https://doi.org/10.1186/1471-2431-7-17.
-
21.
Delvarianzadeh M, Ebrahimi H, Bolbol HN. Surveying pregnant women's nutritional status and some factors affecting it; in cases referring to Shahrood health-care centers. J Birjand Univ Med Sci. 2007;4(13):42-8.
-
22.
Bamgboye EA, Al-Nahedh N. Factors associated with growth faltering in children from rural Saudi Arabia. Afr J Med Med Sci. 2003;32(4):343-7. [PubMed ID: 15259914].
-
23.
Martorell R, Young MF. Patterns of stunting and wasting: potential explanatory factors. Adv Nutr. 2012;3(2):227-33. [PubMed ID: 22516733]. https://doi.org/10.3945/an.111.001107.