Abstract
Background:
Associations between ambient air pollution and emergency department (ED) visits for headache and migraine were examined in a multi-city study during the period of April 2004 to December 2011 in nine cities across Ontario, Canada.Objectives:
Evaluate potential positive associations between air pollution and ED visits for headache.Materials and Methods:
Data on ED visits for headache were retrieved from the national ambulatory care reporting system in Canada. Case-crossover design was used for this study for three diagnosis categories: migraine, headache-OS (other specified, OS) and headache-NOS (not otherwise specified, NOS). A time-stratified case-crossover technique was applied to investgate the associations of ED visits for headache with ambient air pollution. Odds ratios (ORs) and their corresponding 95% confidence intervals for ED visits associated with increased levels of air pollutants were calculated by applying conditional logistic regression.Results:
Among females, statistically significant positive results were observed for one unit increase in inter-quartile range (IQR) of NO2 (IQR = 9 ppb) for lag 0 days: OR = 1.015 (1.000, 1.030) for migraine and for NOS: for NO2 for lags 0 to 2, where the highest result was for lag 0: OR = 1.015 (1.005, 1.026), for SO2 (IQR = 2.5 ppb) for lag 2: OR = 1.012 (1.002, 1.021) and for PM2.5 for lags 1 and 2, OR = 1.011 (1.002, 1.021) and OR = 1.010 (1.000, 1.020) respectively among females. No significant statistically significant results were observed among males.Conclusions:
Our findings support a number of statistically significant positive associations between air pollutants and the number of ED visits for headache and migraine.Keywords
1. Background
Air pollution is associated with hospital admissions for respiratory diseases all over the world (1-7). Headaches, especially migraines, are important causes of morbidity in many modern societies. A longitudinal study in Canada estimated that more than seven million working days are lost annually due to migraine (8). Likewise, in the United States, migraine causes the loss of approximately 150 million work days per year at an estimated lost labor cost of $13 billion (9). In Canada, it has been estimated that 2.6 million adult females and nearly one million adult males experience migraines, but only about one half of these individuals are diagnosed by a physician (10).
There are many self-reported triggers for migraine, including noise, weather, fatigue, stress, diet, menstruation and infections (4, 11-13). Although the link between environmental factors, such as air pollution, temperature and humidity, and migraines or other headaches has not been accepted widely by clinicians, there are a number of studies that suggest that air pollution may be linked to headache (14-28). A multi-city study of emergency department (ED) visits for migraine and headache across five cities in Canada (Edmonton, Halifax, Ottawa, Toronto and Vancouver) supports the association between air pollution and the number of ED visits for headache and migraine (29).
2. Objectives
The aim of the current study was to expand on the previous studies by investigating correlations between ambient air pollution exposures and ED visits for headache and migraine during the period of April 2004 to December 2011 in nine cities across Ontario, Canada: Algoma, Halton, Hamilton, London, Ottawa, Peel, Toronto, Windsor and York. Multi-city studies, versus small studies in individual centers, are known to generate results that are more reliable and less susceptible to biases (30).
For this study, health data were retrieved from the National Ambulatory Care Reporting System (NACRS). The NACRS contains data for all hospital and community-based ambulatory care centers, including day and night surgery, outpatient clinics and ED visits. These data are collected at time of service in participating hospitals. (For more information on NACRS, see the Canadian website).
A case-crossover (CC) design was used in this study (31). ED visits were used to represent health outcomes and were analyzed as separate individual events. Ambient air pollutant concentrations, temperature and relative humidity were obtained from Environment Canada and expressed as daily mean values.
3. Materials and Methods
3.1. Study Population
ED visits for headache and migraine were retrieved from the NACRS using the international classification of diseases, tenth revision (ICD-10) during the period of April 2004 to December 2011. For this study, three categories have been considered: i) ICD-10 code G43 (migraine), ii) ICD-10 code G44 (headache, other specified headache, OS) and iii) ICD-10 code R51 (headache, not otherwise specified headache, NOS). Diagnosed ED visits with primary cause as headache were analyzed.
3.2. Environmental Data
The environmental data were obtained from Environment Canada’s national air pollution surveillance program (NAPS). The daily average values of ozone (O3), nitrogen dioxide (NO2), particulate matter (PM) with an aerodynamic diameter less than 2.5 µm (PM2.5) and sulfur dioxide (SO2) were calculated by averaging over all the NAPS stations within 35 km of each patient’s postal code centroid. Hourly data for temperature and relative humidity for these nine cities were also retrieved from Environment Canada databases. Daily levels for temperature and relative humidity were calculated by averaging hourly data over 24 hour periods. Only meteorological stations within 100 km of each patient’s residential postal code centroid were considered and, if more than one station was available for a patient, the daily values of all stations were averaged.
Carbon monoxide (CO) data were only available for Toronto and Windsor, so these data were analyzed separately.
3.3. Statistical Analysis
For the multi-city study, statistical analysis was performed in two stages. First, a time stratified CC design was applied (32). With this methodology, cases served as their own controls on a set of predefined control days proximate to the time they became cases. Because cases are the perfect match for themselves in personal characteristics (i.e., age, race), the CC method is commonly used in air pollution epidemiology studies (33).
A P value less than 0.05 was considered statistically significant in all analyses. The generated results were reported as odds ratios (ORs) and their 95% confidence intervals (CI).
For the first stage of analysis, ORs for O3, NO2, PM2.5 and SO2 were calculated separately for each city using the PROC PHREG procedure in SAS EG v.4.2. In this model, air pollutant levels were lagged by the same number of days, from 0 to 8 days. Ambient temperature and relative humidity factors were used in the form of quadratic spline of apparent temperature and humidity on the day and one day before (lag 0 and 1) ED visits. Controls are matched to cases by day of week (i.e., day of week is adjusted by design), the control periods are determined as other days in the same month and year.
For the second stage of analysis, individual estimates were combined to calculate an overall effect for all cities; therefore, this stage of study included a meta-analysis of the estimates and their standard errors to achieve a pooled effect estimate. Pooled estimates and their standard errors were calculated using a fixed-effects model, which assumes that individual effect size estimates represent the same underlying parameter and the effect estimates are weighted by the inverse of the variance. A random-effects model was also run, which assumes individual effect size estimates reflect potentially different underlying parameters, coming from a larger parent distribution model, and that effect estimates are weighted by the inverse of the sum of within (34). Meta-analysis and meta-regression were performed using the R language (v. 2.7.2, 2008).
4. Results
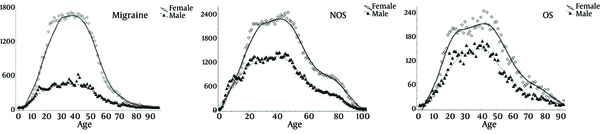
Table 1 summarizes the frequency of visits by type (N = 296,653: 65% NOS, 6% OS and 29% migraine), sex, age group, season (cold (October-March) and warm (April - September) and by city. The majority of visits were for non-specific headaches and the numbers of visits by females were twice as high as males. Figure 1 shows the frequency (counts) of ED visits for three categories by both sex and age (migraine, NOS, and OS). Table 2 summarizes the characteristics of relative humidity and temperature of all cities in this study. Table 3 summarizes the descriptive air pollution statistics by cities. In Table 4, the statistically significant results found for individual cities among lag 0 to 8. ORs and their 95% CIs have been calculated for one ppb increase for NO2, O3 and SO2 and 1 μg/m3 for PM2.5. There were no statistically significant results for the city of Ottawa. Ambient temperature and relative humidity factors were used in form of quadratic spline.
Shows the Frequency (Counts) of ED Visits for Three Categories by Both Sex and Age (Migraine, NOS, and OS)
Frequency of Visits by Type (Migraine, NOS and OS), Sex, Age Group, Season and by City During the Period of April 2004 to December 2011 in Nine Cities
| Description | No. (%) |
|---|---|
| Type | |
| Migraine | 86,318 (29) |
| NOS | 193,254 (65) |
| OS | 17,081 (6) |
| Sex | |
| Female | 198,312 (67) |
| Male | 98,341 (33) |
| Age, y | |
| 0 - 24 | 63,760 (21) |
| 25 - 55 | 170,656 (58) |
| < 55 | 62,237 (21) |
| Seasona | |
| Cold | 140,208 (47) |
| Warm | 156,445 (53) |
| City/Region | |
| Algoma | 13,804 (5) |
| Halton | 16,998 (6) |
| Hamilton | 26,617 (9) |
| London | 20,686 (7) |
| Ottawa | 35,180 (12) |
| Peel | 42,569 (14) |
| Toronto | 92,829 (31) |
| Windsor | 19,495 (7) |
| York | 28,475 (10) |
| Total | 296,653 |
Characteristics of Relative Humidity and Temperature During the Period of April 2004 to December 2011 in 9 Cities
| Variable | Mean | Minimum | Maximum | Q1 | Q3 |
|---|---|---|---|---|---|
| Algoma | |||||
| RH | 75.1 | 29.0 | 100.0 | 68.2 | 82.9 |
| T | 6.2 | -26.2 | 26.4 | -1.1 | 15.3 |
| Halton | |||||
| RH | 70.5 | 35.7 | 95.5 | 62.6 | 78.5 |
| T | 9.7 | -17.9 | 31.0 | 2.2 | 18.3 |
| Hamilton | |||||
| RH | 76.2 | 36.2 | 100.0 | 69.0 | 84.7 |
| T | 9.0 | -19.8 | 30.0 | 1.0 | 17.8 |
| London | |||||
| RH | 73.5 | 33.2 | 98.9 | 66.9 | 81.4 |
| T | 9.1 | -19.7 | 30.6 | 1.0 | 17.9 |
| Ottawa | |||||
| RH | 72.2 | 26.7 | 100.0 | 63.8 | 82.2 |
| T | 7.9 | -26.6 | 29.6 | -0.1 | 17.6 |
| Peel | |||||
| RH | 70.2 | 27.6 | 99.8 | 62.6 | 78.7 |
| T | 9.7 | -20.3 | 31.7 | 1.8 | 18.7 |
| Toronto | |||||
| RH | 72.5 | 24.6 | 99.7 | 64.8 | 81.6 |
| T | 10.1 | -19.3 | 31.5 | 2.5 | 18.7 |
| Windsor | |||||
| RH | 69.5 | 32.4 | 97.4 | 61.4 | 77.7 |
| T | 11.0 | -19.5 | 30.4 | 2.7 | 20.0 |
| York | |||||
| RH | 70.1 | 30.1 | 100.0 | 62.2 | 78.7 |
| T | 9.0 | -20.0 | 32.0 | 1.1 | 18.0 |
Descriptive Air Pollution Statistics by Cities During the Period of April 2004 to December 2011 in 9 Citiesa
| Pollutant | Mean | Minimum | Maximum | Q1 | Q3 |
|---|---|---|---|---|---|
| Algoma | |||||
| NO2 | 5.1 | 0.0 | 24.0 | 3.0 | 7.0 |
| O3 | 28.5 | 2.0 | 80.0 | 21.0 | 35.0 |
| PM2.5 | 5.3 | 0.0 | 29.0 | 2.2 | 6.5 |
| SO2 | 1.1 | 0.0 | 17.0 | 0.0 | 2.0 |
| Halton | |||||
| NO2 | 12.9 | 1.0 | 51.2 | 8.5 | 16.2 |
| O3 | 25.8 | 2.0 | 67.7 | 18.4 | 32.4 |
| PM2.5 | 7.7 | 0.5 | 34.2 | 4.0 | 9.8 |
| SO2 | 2.3 | 0.0 | 14.0 | 1.0 | 3.0 |
| Hamilton | |||||
| NO2 | 13.9 | 1.7 | 63.0 | 8.5 | 18.0 |
| O3 | 26.3 | 1.5 | 70.0 | 19.0 | 32.5 |
| PM2.5 | 9.8 | 0.0 | 64.2 | 5.1 | 12.7 |
| SO2 | 4.1 | 0.0 | 35.5 | 1.4 | 5.5 |
| London | |||||
| NO2 | 10.9 | 0.0 | 51.0 | 7.0 | 14.0 |
| O3 | 26.3 | 1.0 | 66.0 | 19.0 | 33.0 |
| PM2.5 | 9.5 | 0.0 | 66.3 | 5.0 | 12.2 |
| SO2 | 1.7 | 0.0 | 15.0 | 1.0 | 2.0 |
| Ottawa | |||||
| NO2 | 8.7 | 1.0 | 47.0 | 4.5 | 11.5 |
| O3 | 24.1 | 1.0 | 66.5 | 17.5 | 30.5 |
| PM2.5 | 7.0 | 0.0 | 67.7 | 3.0 | 9.3 |
| SO2 | 0.8 | 0.0 | 13.0 | 0.0 | 1.0 |
| Peel | |||||
| NO | 13.2 | 2.0 | 54.0 | 7.5 | 17.0 |
| O3 | 25.0 | 1.0 | 69.5 | 18.0 | 31.5 |
| PM2.5 | 8.5 | 0.0 | 64.9 | 4.0 | 10.8 |
| SO2 | 1.4 | 0.0 | 12.0 | 0.5 | 2.0 |
| Toronto | |||||
| NO2 | 18.5 | 4.5 | 62.1 | 13.2 | 22.6 |
| O3 | 22.5 | 1.5 | 60.7 | 15.4 | 28.8 |
| PM2.5 | 9.3 | 0.0 | 66.8 | 4.6 | 12.0 |
| SO2 | 1.8 | 0.0 | 13.7 | 0.5 | 2.3 |
| Windsor | |||||
| NO2 | 15.6 | 2.4 | 55.5 | 10.9 | 19.0 |
| O3 | 25.7 | 1.0 | 68.5 | 17.4 | 33.5 |
| PM2.5 | 9.5 | 0.8 | 33.6 | 5.1 | 12.5 |
| SO2 | 4.3 | 0.0 | 24.3 | 1.5 | 6.0 |
| York | |||||
| NO2 | 8.2 | 0.0 | 47.0 | 4.0 | 11.0 |
| O3 | 29.2 | 3.0 | 71.0 | 22.0 | 36.0 |
| PM2.5 | 6.7 | 0.0 | 27.0 | 3.0 | 9.0 |
| SO2 | 1.2 | 0.0 | 8.0 | 0.0 | 2.0 |
Summary of Statistically Significant Association With Pollutants for Individual Cities Among Lag 0 to 8 Days in Nine Cities for the Period of April 2004 to December 2011
| Type | Sex | Lag | Pollutant | OR | 95%CI |
|---|---|---|---|---|---|
| Algoma | |||||
| NOSa | Female | 7 | O3 | 1.004 | (1.000, 1.009) |
| NOS | Male | 6 | SO2 | 1.046 | (1.000, 1.093) |
| Hamilton | |||||
| Migraine | Female | 7 | SO2 | 1.013 | (1.005, 1.020) |
| NOS | Female | 2 | NO2 | 1.005 | (1.000, 1.010) |
| London | |||||
| NOS | Male | 2 | O3 | 1.007 | (1.002, 1.013) |
| NOS | Male | 1 | O3 | 1.007 | (1.000, 1.013) |
| NOS | Male | 3 | O3 | 1.006 | (1.000, 1.011) |
| Peel | |||||
| Migraine | Female | 3 | PM2.5 | 1.005 | (1.000, 1.010) |
| NOS | Female | 4 | O3 | 1.004 | (1.001, 1.010) |
| NOS | Male | 0 | SO2 | 1.023 | (1.003, 1.040) |
| NOS | Male | 1 | SO2 | 1.021 | (1.002, 1.040) |
| NOS | Male | 2 | SO2 | 1.020 | (1.000, 1.040) |
| Toronto | |||||
| NOS | Female | 0 | NO2 | 1.003 | (1.001, 1.005) |
| NOS | Female | 1 | NO2 | 1.003 | (1.001, 1.050) |
| NOS | Female | 2 | NO2 | 1.003 | (1.001, 1.005) |
| NOS | Female | 3 | NO2 | 1.003 | (1.005, 1.004) |
| NOS | Female | 4 | NO2 | 1.002 | (1.000, 1.004) |
| NOS | Female | 5 | NO2 | 1.002 | (1.000, 1.004) |
| NOS | Female | 0 | PM2.5 | 1.002 | (1.000, 1.004) |
| NOS | Female | 1 | PM2.5 | 1.002 | (1.000, 1.004) |
| Windsor | |||||
| Migraine | Female | 4 | PM2.5 | 1.018 | (1.003, 1.033) |
| Migraine | Female | 5 | NO2 | 1.008 | (1.002, 1.015) |
| Migraine | Female | 5 | PM2.5 | 1.019 | (1.005, 1.033) |
| Migraine | Female | 7 | NO2 | 1.008 | (1.001, 1.014) |
| NOS | Female | 2 | SO2 | 1.010 | (1.002, 1.018) |
| NOS | Female | 2 | PM2.5 | 1.011 | (1.005, 1.022) |
| York | |||||
| NOS | Female | 0 | SO2 | 1.054 | (1.004, 1.106) |
| NOS | Female | 1 | SO2 | 1.054 | (1.004, 1.107) |
| NOS | Female | 2 | SO2 | 1.056 | (1.004, 1.110) |
| NOS | Female | 4 | PM2.5 | 1.012 | (1.002, 1.022) |
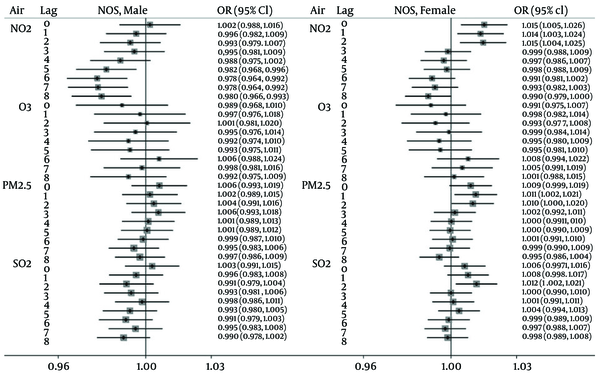
ORs and their 95% CIs have been calculated for one unit increase in their interquartile range (IQR) of air pollutants, which is equivalent to the difference between the values of the 75th - 25th percentiles. The IQR values were calculated among all 9 cities and are 9, 14.5 and 2.5 ppb respectively, for daily means of NO2, O3, SO2 and 7.12 μg/m3 for PM2.5 for category of migraine, for females, statistically significant positive results were observed for NO2 for lag 0 days: OR = 1.015 (1.000, 1.030). For males, positive results for NO2 were obtained for lags 4 to 6 positive results were also observed for O3, among lags 0 to 3 and for PM 2.5 for lags 3 and 4 days.
The results for NOS for males (left panel) and females (right panel) are presented in Figure 2. Statistically significant positive results were observed for females for NO2 for lags 0 to 2 days, where the highest result is for lag 0 days: OR = 1.015 (1.005, 1.026). For SO2 for lag 2 days: OR = 1.012 (1.002, 1.021). Statistically significant positive results were also observed for PM2.5 for lags 1 and 2 days: OR = 1.011 (1.002, 1.021) and OR = 1.010 (1.000, 1.020), respectively. No significant positive results were observed for males; instead, statistically significant negative results were observed. To study these negative results in more detail, the possible comorbidity between NOS and circulatory system diseases and mental behavioural disorders were analyzed. For all patients in this category, patients who also suffered from either circulatory system diseases (ICD 10 prefix “I”) or mental behavioural disorders (ICD 10 prefix “F”) as a secondary disease were identified. Because of the small sample size of this sub-analysis, the nine cities and both females and males (N = 4,850 patients) were considered as a single group. Under these conditions, positive results were observed for NO2 among lags 2 to 4 and 7 to 8 for females and among lags 2, 4 and 5 for males. No statistically significant negative results were observed for any of the pollutants.
The Results for NOS for Males (Left Panel) and Females (Right Panel)
In the analysis for the two major cities where the daily values of CO were available (Toronto and Windsor), a statistical significant association was found between one unit increase in IQR value of CO (IQR = 0.1 ppm, calculated for two cities) and ED visits for headache and migraine for females. For the city of Toronto, statistically significant positive results were observed for lag 0 OR = 1.069 (1.003, 1.031) and lag 1 for migraine, and lags 0 to 4 and lag 7 days for NOS. For the city of Windsor, among lag 6 and 7, OR = 1.040 (1.004, 1.079) and OR = 1.053 (1.017, 1.091), respectively, for migraine; and lag 2 days, OR = 1.038 (1.008, 1.068) for NOS. There have been no statistically significant results for the category OS.
The random effect model was used to allow for the possibility that the estimates from different cities may be estimates of different parameters, rather than just a single underlying parameter. By using the random effects meta-analysis, a heterogeneity variance component was obtained. Approximately 8% of the estimates passed the Q-statistic test and in two cases statistically significant results were observed: OR = 1.001 (1.000, 1.003), OR = 1.002 (1.000, 1.003) for PM2.5 lags 0 and 1 respectively for category NOS among females.
5. Discussion
In this study, data 296,653 patients from nine major cities in Ontario, Canada were analyzed. Air pollution data were linked to ED visits for headache and migraine during the period of April 2004 to December 2011. This is one of the largest multi-city studies in Canada investigating the effects of air pollution on ED visits for headache and migraine. The results were presented for all three headache categories and for both genders. The largest statistically significant association was obtained for same day NO2 among females, for both migraine and NOS. Also, positive results were also obtained for O3 for NOS for females among lags 4 to 8. SO2 showed positive association for lags 1 and 7 for migraine and statistically significant association for lag 3 for NOS among females.
These results agree with previous studies in this area. In another multi-city study (29), a time-series study of 13,000 ED visits for headache and migraine among five major cities in Canada showed an increase in daily visits for headache and migraine associated with NO2, SO2 and PM2.5. A study from Finland also detected significant effects of SO2 and PM 2.5 on ED visits for migraine and headache (35). In similar time series studies in Ottawa (19), Montreal (18) and Edmonton (25), the two common pollutants, NO2 and SO2, were positively associated with ED visits for non-migraine headaches. Another study in Chile (27) also reported the associations of CO, NO2, O3, SO2 and PM2.5 with headaches. This study also reported that there was no significant effect modification by age, sex or season. Another study reported in (28) found a strong association of headache with ambient temperature. These findings support an association between NO2 exposures for headaches not diagnosed as migraine. Mukamal et al. (28) reported weather fluctuations as a major migraine trigger and show a higher mean ambient temperature in the 24 hours preceding ED visit (lag 1) increases the acute risk of headache. For this reason, daily temperature and relative humidity were included in our models on the day and one day before of ED visit as a confounder. In the case of NO2, negative significant results were seen for males; however, in the subgroup of patients restricted to comorbidity, no negative significant results were observed and results were positive among most of lags. It may indicate that some ED visits for headache (NOS) are also related to other health conditions and the patients’ response to environmental triggers.
In this study, slightly stronger results were found for the age group 25 to 55 years during the warm season. In addition, the results show a stronger association between air pollution and ED visits for both headache and migraine among females. Because PM2.5 appears to induce sympathetic nervous system activation (36-40), PM2.5 could be anticipated to have the strongest association with headache as compared with other air pollutants; however, no association was found between PM2.5 and ED visits for headache or migraine. In support of these findings, a large-scale study in Montreal (18) found that PM2.5 showed a much weaker risk of headaches than the other pollutants analyzed.
There are several limitations of the present study. The CO data were unavailable for most of the days in our study period, so analysis could only be performed using the data from two cities (Toronto and Windsor). Also, there were some missing PM2.5 and humidity data for some periods in our study. This might partially explain the small effect of PM2.5 on headache and migraine visits to the ED. Despite these limitations, our findings support the associations between air pollutants and the number of ED visits for headache and migraine.
Acknowledgements
References
-
1.
Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360(9341):1233-42. [PubMed ID: 12401268]. https://doi.org/10.1016/S0140-6736(02)11274-8.
-
2.
Burnett RT, Brook JR, Yung WT, Dales RE, Krewski D. Association between ozone and hospitalization for respiratory diseases in 16 Canadian cities. Environ Res. 1997;72(1):24-31. [PubMed ID: 9012369]. https://doi.org/10.1006/enrs.1996.3685.
-
3.
Pope CA, Dockery DW, Schwartz J. Review of epidemiological evidence of health effects of particulate air pollution. Inhal Toxicol. 1995;7(1):1-18. https://doi.org/10.3109/08958379509014267.
-
4.
Roth HD, Hwang PM, Li Y. Assessment of recent ozone short-term epidemiologic studies. Inhal Toxicol. 2001;13(1):1-24. [PubMed ID: 11153057]. https://doi.org/10.1080/089583701753333267.
-
5.
Health effects of outdoor air pollution. Committee of the Environmental and Occupational Health Assembly of the American Thoracic Society. Am J Respir Crit Care Med. 1996;153(1):3-50. [PubMed ID: 8542133]. https://doi.org/10.1164/ajrccm.153.1.8542133.
-
6.
Spix C, Anderson HR, Schwartz J, Vigotti MA, LeTertre A, Vonk JM, et al. Short-term effects of air pollution on hospital admissions of respiratory diseases in Europe: a quantitative summary of APHEA study results. Air Pollution and Health: a European Approach. Arch Environ Health. 1998;53(1):54-64. [PubMed ID: 9570309]. https://doi.org/10.1080/00039899809605689.
-
7.
Zanobetti A, Schwartz J, Dockery DW. Airborne particles are a risk factor for hospital admissions for heart and lung disease. Environ Health Perspect. 2000;108(11):1071-7. [PubMed ID: 11102299].
-
8.
Pryse-Phillips W, Findlay H, Tugwell P, Edmeads J, Murray TJ, Nelson RF. A Canadian population survey on the clinical, epidemiologic and societal impact of migraine and tension-type headache. Can J Neurol Sci. 1992;19(3):333-9. [PubMed ID: 1393842].
-
9.
Gary L, Baxter K. Migraine: Health effect of air pollution. 2005. Available from: http://www.ecopolitics.ca/migraine-health-effect-of-air-pollution/.
-
10.
O'Brien B, Goeree R, Streiner D. Prevalence of migraine headache in Canada: a population-based survey. Int J Epidemiol. 1994;23(5):1020-6. [PubMed ID: 7860153].
-
11.
Kelman L. The triggers or precipitants of the acute migraine attack. Cephalalgia. 2007;27(5):394-402. [PubMed ID: 17403039]. https://doi.org/10.1111/j.1468-2982.2007.01303.x.
-
12.
Osterman PO, Lovstrand KG, Lundberg PO, Lundquist S, Muhr C. Weekly headache periodicity and the effect of weather changes on headache. Int J Biometeorol. 1981;25(1):39-45. [PubMed ID: 7228440].
-
13.
Steiner T, MacGregor E, Davies P. Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type, cluster and medication-overuse headache. British association for the study of headache; 2007. Available from: ttp://wwwbashorguk/guidelines.
-
14.
Chabriat H, Danchot J, Michel P, Joire JE, Henry P. Precipitating factors of headache. A prospective study in a national control-matched survey in migraineurs and nonmigraineurs. Headache. 1999;39(5):335-8. [PubMed ID: 11279913].
-
15.
Chang CC, Chiu HF, Yang CY. Fine particulate air pollution and outpatient department visits for headache in Taipei, Taiwan. J Toxicol Environ Health A. 2015;78(8):506-15. [PubMed ID: 25849767]. https://doi.org/10.1080/15287394.2015.1010465.
-
16.
Chiu HF, Weng YH, Chiu YW, Yang CY. Air pollution and daily clinic visits for headache in a subtropical city: Taipei, Taiwan. Int J Environ Res Public Health. 2015;12(2):2277-88. [PubMed ID: 25690001]. https://doi.org/10.3390/ijerph120202277.
-
17.
Diaz E, Smith-Sivertsen T, Pope D, Lie RT, Diaz A, McCracken J, et al. Eye discomfort, headache and back pain among Mayan Guatemalan women taking part in a randomised stove intervention trial. J Epidemiol Community Health. 2007;61(1):74-9. [PubMed ID: 17183019]. https://doi.org/10.1136/jech.2006.043133.
-
18.
Szyszkowicz M. Air pollution and daily emergency department visits for headache in Montreal, Canada. Headache. 2008;48(3):417-23. [PubMed ID: 18302702]. https://doi.org/10.1111/j.1526-4610.2007.00808.x.
-
19.
Szyszkowicz M. Ambient air pollution and daily emergency department visits for headache in Ottawa, Canada. Headache. 2008;48(7):1076-81. [PubMed ID: 18218009]. https://doi.org/10.1111/j.1526-4610.2007.01039.x.
-
20.
Medina S, Le Tertre A, Quenel P, Le Moullec Y, Lameloise P, Guzzo JC, et al. Air pollution and doctors' house calls: results from the ERPURS system for monitoring the effects of air pollution on public health in Greater Paris, France, 1991-1995. Evaluation des Risques de la Pollution Urbaine pour la Sante. Environ Res. 1997;75(1):73-84. [PubMed ID: 9356196].
-
21.
Nattero G, Enrico A. Outdoor pollution and headache. Headache. 1996;36(4):243-5. [PubMed ID: 8675430].
-
22.
Prince PB, Rapoport AM, Sheftell FD, Tepper SJ, Bigal ME. The effect of weather on headache. Headache. 2004;44(6):596-602. [PubMed ID: 15186304]. https://doi.org/10.1111/j.1526-4610.2004.446008.x.
-
23.
Segala C, Poizeau D, Neukirch F, Aubier M, Samson J, Gehanno P. Air pollution, passive smoking, and respiratory symptoms in adults. Arch Environ Health. 2004;59(12):669-76. [PubMed ID: 16789476]. https://doi.org/10.1080/00039890409602952.
-
24.
Szyszkowicz M, Porada E. Ambient Sulphur Dioxide and Female ED Visits for Migraine. ISRN Neurol. 2012;2012:279051. [PubMed ID: 22523701]. https://doi.org/10.5402/2012/279051.
-
25.
Szyszkowicz M, Stieb DM, Rowe BH. Air pollution and daily ED visits for migraine and headache in Edmonton, Canada. Am J Emerg Med. 2009;27(4):391-6. [PubMed ID: 19555607]. https://doi.org/10.1016/j.ajem.2008.03.013.
-
26.
Vodonos A, Novack V, Zlotnik Y, Ifergane G. Ambient air pollution, weather and daily emergency department visits for headache. Cephalalgia. 2015;35(12):1085-91. [PubMed ID: 25653308]. https://doi.org/10.1177/0333102415570300.
-
27.
Dales RE, Cakmak S, Vidal CB. Air pollution and hospitalization for headache in Chile. Am J Epidemiol. 2009;170(8):1057-66. [PubMed ID: 19741041]. https://doi.org/10.1093/aje/kwp217.
-
28.
Mukamal KJ, Wellenius GA, Suh HH, Mittleman MA. Weather and air pollution as triggers of severe headaches. Neurology. 2009;72(10):922-7. [PubMed ID: 19273827]. https://doi.org/10.1212/01.wnl.0000344152.56020.94.
-
29.
Szyszkowicz M, Kaplan GG, Grafstein E, Rowe BH. Emergency department visits for migraine and headache: a multi-city study. Int J Occup Med Environ Health. 2009;22(3):235-42. [PubMed ID: 19819836]. https://doi.org/10.2478/v10001-009-0024-5.
-
30.
Dominici F, Samet JM, Zeger SL. Combining evidence on air pollution and daily mortality from the 20 largest US cities: a hierarchical modelling strategy. J R Stat Soc. 2000;163(3):263-302. https://doi.org/10.1111/1467-985X.00170.
-
31.
Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133(2):144-53. [PubMed ID: 1985444].
-
32.
Janes H, Sheppard L, Lumley T. Case-crossover analyses of air pollution exposure data: referent selection strategies and their implications for bias. Epidemiology. 2005;16(6):717-26. [PubMed ID: 16222160].
-
33.
Bateson TF, Schwartz J. Control for seasonal variation and time trend in case-crossover studies of acute effects of environmental exposures. Epidemiology. 1999;10(5):539-44. [PubMed ID: 10468428].
-
34.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-88. https://doi.org/10.1016/0197-2456(86)90046-2.
-
35.
Partti-Pellinen K, Marttila O, Vilkka V, Jaakkola JJ, Jappinen P, Haahtela T. The South Karelia Air Pollution Study: effects of low-level exposure to malodorous sulfur compounds on symptoms. Arch Environ Health. 1996;51(4):315-20. [PubMed ID: 8757412]. https://doi.org/10.1080/00039896.1996.9936031.
-
36.
Bouthillier L, Vincent R, Goegan P, Adamson IYR, Bjarnason S, Stewart M, et al. Acute effects of inhaled urban particles and ozone: lung morphology, macrophage activity, and plasma endothelin-1. Am J Pathol. 1998;153(6):1873-84. https://doi.org/10.1016/S0002-9440(10)65701-X.
-
37.
Gold DR, Litonjua A, Schwartz J, Lovett E, Larson A, Nearing B, et al. Ambient pollution and heart rate variability. Circulation. 2000;101(11):1267-73. [PubMed ID: 10725286].
-
38.
Mukae H, Vincent R, Quinlan K, English D, Hards J, Hogg JC, et al. The effect of repeated exposure to particulate air pollution (PM10) on the bone marrow. Am J Respir Crit Care Med. 2001;163(1):201-9. [PubMed ID: 11208647]. https://doi.org/10.1164/ajrccm.163.1.2002039.
-
39.
Tao F, Kobzik L. Lung macrophage-epithelial cell interactions amplify particle-mediated cytokine release. Am J Respir Cell Mol Biol. 2002;26(4):499-505. [PubMed ID: 11919087]. https://doi.org/10.1165/ajrcmb.26.4.4749.
-
40.
Vincent R, Kumarathasan P, Goegan P, Bjarnason SG, Guenette J, Berube D, et al. Inhalation toxicology of urban ambient particulate matter: acute cardiovascular effects in rats. Res Rep Health Eff Inst. 2001;(104):5-54. discussion 55-62. [PubMed ID: 11833973].