Abstract
Background:
One of the 3 main goals of any health system is to meet the non-medical expectations of individuals while interacting with health system. The purpose of this study is to evaluate the health system responsiveness before and after the implementation of the health transformation plan (HTP) in Iran.Methods:
In this longitudinal study, a household survey was conducted at the district 17 of Tehran, Iran in 2003, 2008, and 2015. A sample of 600 families was selected using a two-stage cluster sampling approach. Data were collected using a questionnaire and face-to-face interview. Chi square and One Way Anova were used to analyze the data in the SPSS 16.Results:
The importance of all dimensions of responsiveness has decreased compared to previous years in 2015. Dignity (83.46%) had the best performance (high score) and choice (69.23%) had the worst performance (low score) in outpatient services. The best performance score was confidentiality (81.7%) in inpatient services and the worst was autonomy (67.76%). Private centers performed better than other centers in all dimensions of responsiveness. This difference was statistically significant in outpatient services (P value < 0.05) and was significant in inpatient services only in 2001. Principal component analysis found for out-patient care responsiveness are 2 main factors explaining 69.5% of the variance and for in-patient care responsiveness 1 factor explaining 91.7% of the variance. Overall responsiveness level has increased.Conclusions:
Given the increasing level of responsiveness in outpatient and inpatient services after the implementation of the HTP, it can be concluded that this plan has been effective. Interaction of patients and service providers is an issue that should be addressed by health sector reform.Keywords
Health System Responsiveness Inpatient Services Outpatient Services Health Transformation Plan
1. Background
Although preservation and improvement of population health is the main responsibility of any health system, responsiveness and fairness of financial contributions are another of its essential goals (1, 2).
Responsiveness is related to the system’s ability to address the rightful performance of client non-medical expectations while interacting with health care providers (3). The responsiveness concept has 8 domains, including: autonomy, prompt attention, confidentiality, choice of provider, dignity, clarity of communication, quality of basic amenities, and social support. These non-medical domains are important to all human beings (4, 5). These can further be categorized into 2 major domains: “Respect for human rights”: containing of the domains dignity, autonomy, confidentiality, and communication and “Client-orientation”: containing of the domains choice, prompt attention, quality of basic amenities, and social support (6).
Improving these non-health functions of a health system is important because it is an undisputable element to increasing people’s well-being, that being a total and ultimate mission of a health system (7).
Jones et al. showed that low level of responsiveness may lead to less access to health services, resulting in low utilization of some of these services in certain groups in the population (8). Improving responsiveness can be a better utilization of health services and can improve the health of individuals (9).
World health organization report 2000 ranked 191 countries in terms of health system responsiveness. In this ranking, Iran received 100th place, which represented serious need for attention to this important goal of the health system (3, 5). Ministry of Health in Iran, as the main stewardship of health care system in the country, implemented the health transformation plan (HTP) since May 5, 2014 that one of its ultimate objectives was to increase responsiveness (10). HTP includes 8 executive packages: reducing out of pocket for hospitalized patients, supporting doctors to stay in deprived areas, presenting of specialist physicians in hospitals, promoting hoteling quality, promoting natural delivery, financial protection for patients with specific disease, and setting up air emergency (10).
Given that one of the ultimate goals of the HTP is to increase responsiveness, the findings of the present study will help policy makers assess the success of the plan in reaching its ultimate goals in order to review and revise it if needed.
2. Methods
In this longitudinal study a household survey was conducted in 2003, 2008, and 2015. The study population indcluded the households located in district 17 of Tehran, Iran. The district (population: 248,589, households: 75,872) (11) is located southwest of Tehran and has a relatively low socioeconomic status compared with the rest of Tehran. Data gathering instrument was responsiveness module of world health survey (WHS) questionnaire. This module contains questions about “health services utilization”, “importance of responsiveness domains“, and “people’s view about responsiveness domain of outpatient and inpatient services, which were used. The validity and reliability of the translated version of the questionnaire has been confirmed in the previous study (5). Inclusion criteria were (1) participation in the studies of 2003 and 2008, (2) being an adult (18 years old or older), and (3) receiving outpatient care during the past 12 months or inpatient care in the past 5 years. Data collection involved face-to-face interviews. Descriptive statistics, Chi-square, and One-Way Anova were used to analyze the data in the SPSS 16. All graphs and tables were produced using Microsoft Excel and Microsoft word 2007.
Household views have been evaluated on responsiveness of outpatient and inpatient services in 2003 and 2008 in the 17th district of Tehran. In order to assess the effect of HTP, this study measures responsiveness in the same population in 2015, thus measuring the trend of responsiveness in this district.
In the 1st and 2nd surveys in this district in 2003 and 2008, two-stage cluster sampling approach was used. In the 1st stage, 64 clusters were identified using a systematic sampling frame developed by the Iran statistics center. Each cluster included up to 18 households. Then, from each household, an adult individual who was 18 years or older was randomly selected by Kish method method after completing the household list (5). The same households (603 households) were referred and the responsiveness questionnaire was completed for them in 2015. Of the households, there were 52 addresses that were not replaced by the right side of the cluster. The principal component analysis (PCA) was used to extract the main factors affecting the health system responsiveness. The study was approved by the ethics committee of the Tehran University of Medical Sciences. Participation in this study was optional for individuals. They were assured that all of their information would remain confidential. The participants signed or marked (if illiterate) the informed consent forms.
3. Results
The socio-demographic characteristics of the study population are displayed in Table 1. The mean age of the population has increased 6.62 years in the duration of study. The majority of the population was male (51.7%, 52.10%) and had a high school education. Furthermore, the numbers of people who are married have increased during the study.
Socio-Demographic Characteristics of the Study Sample
| Variable | 2003a | 2008a | 2015a |
|---|---|---|---|
| Education | |||
| Less than elementary schoolb | 22 | 21.8 | 23.8 |
| Elementary school | 21 | 20.6 | 18.7 |
| Guidance school | 21.7 | 19.4 | 18.5 |
| High school | 30 | 29.6 | 27.1 |
| University degree | 5.3 | 8.6 | 11.9 |
| Marital status | |||
| Never married | 49.2 | 48.5 | 42.6 |
| Married | 46.9 | 47.1 | 50.5 |
| Separated | 0.3 | 0.4 | 0.4 |
| Divorced | 0.4 | 0.3 | 1.1 |
| Widow/Widower | 3.2 | 3.7 | 5.3 |
| Gender | |||
| Female | - | 48.3 | 47.9 |
| Male | - | 51.7 | 52.10 |
| Mean age | 30.2 | 31.9 | 36.82 |
| Median age | 25 | 28 | 35 |
Table 2 shows the rate of service utilization for outpatient (in the previous 12 months) and inpatient services (in the previous 5 years). Most of the participants used public services for outpatient (58.5% in 2003, 62.1% in 2008, and 75.3% in 2015) and inpatient (89% in 2003, 79% in 2008, and 91.9% in 2015) care. Also, the use of public services had the highest share in 2015.
Health Services Utilization Based on Type of Service
| Type of Services | Outpatient Services | Inpatient Services | ||||
|---|---|---|---|---|---|---|
| 2003 | 2008 | 2015 | 2003 | 2008 | 2015 | |
| Public | 395 (58.5) | 365 (62.1) | 420 (75.3) | 269 (89) | 162 (79) | 217 (91.9) |
| Private | 267 (39.3) | 200 (34) | 131 (23.5) | 24 (9) | 33 (16.1) | 18 (7.6) |
| Charity | 15 (2.2) | 23 (3.9) | 7 (1.2) | 6 (2) | 10 (4.9) | 1 (0.4) |
| Total | 677 (100) | 588 (100) | 558 (100) | 299 (100) | 205 (100) | 236 (100) |
Our results showed more than 78% of individuals rated all aspects of responsiveness as very important or important. Quality of basic amenities (98%) and dignity (97.5%) in 2003, quality of basic amenities, communication and prompt attention (97%) in 2008, and communication (90%) in 2015 were the most important aspects during the study. It should be noted that the importance of all aspects of responsiveness has decreased compared to previous years in 2015 (Figure 1).
Comparing the Importance of Responsiveness Domains in Different Years
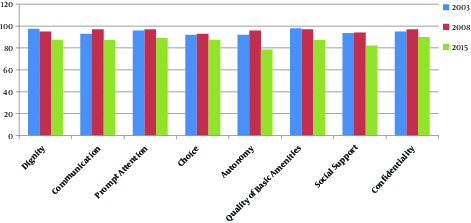
Figure 2 shows the scores of outpatient service responsiveness domains in 2003, 2008, and 2015. The scores of all aspects of responsiveness were higher than other years in 2003 except choice and autonomy. The trend for dignity and confidentiality was descending from 2003 to 2015. Also, responsiveness scores in all dimensions except dignity and confidentiality increased in 2015 compared to 2008. In general, for most aspects, responsiveness scores were the lowest in 2008.
Comparison of Responsiveness Dimensions in Outpatient Services from 2003 to 2015
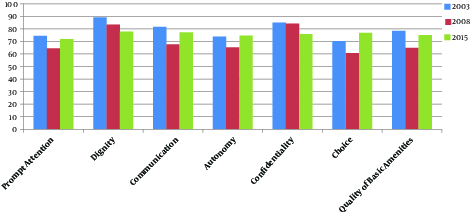
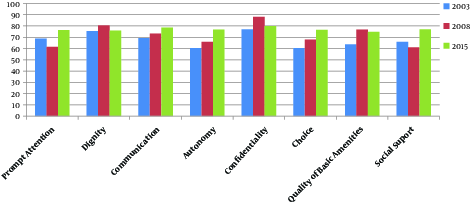
Figure 3 shows the proportion of people reported responsiveness of inpatient services as “good or very good” in all domains in 3 periods. Overall, the scores of all aspects of responsiveness have increased in 2008 and 2015 compared to 2003. Most of responsiveness domains (social support, choice, autonomy, communication, and prompt attention) had the most score in 2015. The trend for autonomy, communication, and choice was increasing from 2003 to 2015.
Comparison of Responsiveness Dimensions in Inpatient Services from 2003 to 2015
Comparison of responsiveness aspects of outpatient and inpatient services in public, private, and charity centers have been shown in Table 3. In outpatient services, private centers performed better than other centers in all aspects during the study. (P value < 0.05 except for dignity and confidentiality in 2015).
Percentage of People Rated Responsiveness Domains of Outpatient and Inpatient Services as “Good” or “Very Good” Based on Type of Center
| Dimensions of Responsiveness | Year | Outpatient | Inpatient | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Public | Private | Charity | P Value | Public | Private | Charity | P Value | ||
| Prompt attention | 2003 | 77 | 80 | 58 | < 0.001 | 70 | 89 | 50 | < 0.001 |
| 2008 | 53 | 61.3 | 44.4 | 0.02 | 45.3 | 47.1 | 33.3 | 0.534 | |
| 2015 | 68.25 | 82.44 | 83.33 | 0.01 | 75.57 | 94.44 | 0 | 0.03 | |
| Dignity | 2003 | 88 | 92 | 92 | < 0.001 | 75 | 84 | 73 | < 0.001 |
| 2008 | 71 | 80 | 78 | 0.04 | 57.8 | 70.6 | 57.1 | 0.211 | |
| 2015 | 75.29 | 86.15 | 83.33 | 0.06 | 76.03 | 83.33 | 0 | 0.1 | |
| Communication | 2003 | 81 | 89 | 67 | < 0.001 | 70 | 78 | 64 | <0.001 |
| 2008 | 60.4 | 71.6 | 62.3 | 0.007 | 51.9 | 58.8 | 52.4 | 0.648 | |
| 2015 | 73.44 | 87.02 | 100 | 0.006 | 78.50 | 88.88 | 0 | 0.08 | |
| Autonomy | 2003 | 78 | 87 | 66 | < 0.001 | 62 | 62 | 60 | < 0.001 |
| 2008 | 54 | 60 | 46 | 0.01 | 48.9 | 47.1 | 57.1 | 0.727 | |
| 2015 | 70.67 | 85.49 | 100 | 0.003 | 76.30 | 88.88 | 0 | 0.08 | |
| Confidentiality | 2003 | 81 | 88 | 91 | < 0.001 | 78 | 88 | 60 | < 0.001 |
| 2008 | 58 | 70 | 49 | 0.001 | 68.4 | 78.4 | 61.9 | 0.263 | |
| 2015 | 73.74 | 81.67 | 100 | 0.1 | 79.9 | 88.88 | 0 | 0.08 | |
| Choice | 2003 | 67.5 | 79 | 75 | <0.001 | 62 | 56 | 50 | < 0.001 |
| 2008 | 60 | 73.4 | 70.3 | 0.003 | 60 | 77.2 | 58.3 | 0.231 | |
| 2015 | 73.03 | 88.54 | 83.33 | 0.003 | 76.52 | 83.33 | 0 | 0.1 | |
| Quality of basic amenities | 2003 | 77 | 83 | 83 | < 0.001 | 67 | 72 | 28 | < 0.001 |
| 2008 | 56 | 69 | 50 | 0.005 | 52.7 | 70.7 | 42.9 | 0.31 | |
| 2015 | 72.07 | 83.96 | 100 | 0.02 | 74.29 | 88.88 | 0 | 0.08 | |
| Social support | 2003 | 70 | 72 | 54 | < 0.001 | ||||
| 2008 | 53.4 | 58.8 | 61.9 | 0.599 | |||||
| 2015 | 76.63 | 88.88 | 0 | 0.08 | |||||
In inpatient services, private centers performed better than public and charity centers in all aspects (except autonomy and choice in public centers in 2008 and 2003 respectively and social support in charity centers in 2008) during the study. These differences were significant in all aspects of responsiveness in 2003 (P value < 0.001), and for other years, it was only significant for “prompt attention” in 2015. Generally, performances of public and private centers were promoted in 2015.
The results of the study showed that there is no statistically difference between participants’ characteristics (gender, marital, and educational status) and responsiveness scores.
PCA revealed that one main component explains 91.7% of the variance for inpatient service responsiveness and 2 main components explaining 69.5% of the variances for outpatient services responsiveness. The 1 factor for inpatient care responsiveness included 15 items with 2 each on prompt attention, dignity, communication, autonomy, confidentiality, quality of basic amenities, social support, and with one for choice (explaining 91.7% of the variance). The 2 factors for the outpatient care responsiveness included 1) 8 items with 2 each on prompt attention, dignity, communication, and autonomy (explaining 39.4% of the variance) and 2) 5 items with 2 each on Confidentiality and Quality of basic amenities and with 1for choice (explaining 30.1% of the variance).
4. Discussion
In order to achieve the goals of the health system, the HTP was implemented in Iran since May 5, 2014. The plan has 3 general approaches to protecting people from financing, providing access to health services, and improving service quality. One of its main goals is to increase the responsiveness of the health system (9).
According to the findings, the majority of the respondents (over 80%) rated all aspects of responsiveness as very important or important. However, the importance of all dimensions has decreased compared to the previous years in 2015. Perhaps due to the implementation of the HTP and the establishment of its service packages that reduce financial burden for patients, the importance of responsiveness dimensions has diminished. Communication, quality of basic amenities, and prompt attention received the highest scores and autonomy received a lower score in terms of their importance. These findings have been repeated in several previous studies in Iran (4, 12-14). It means that service recipients kept their preferences about the importance of responsiveness domains. In addition, in other studies, communication, dignity, quality, and prompt attention were identified as the most important aspects (15, 16).
In our study, dignity was the best performing domain in outpatient services in all the years of the study. This means that the health system in Iran has been able to provide a respectful and non-discriminatory setting/care for patients. The same result is found in the studies in India and Thailand that survey socio-economic disparities in health system responsiveness and health system responsiveness for delivery care, respectively (1, 17).
The 2nd rank in terms of performance in outpatient services was dedicated to confidentiality. It means being able to talk privately to providers and keeping patient information secret. This finding is in line with the studies from Tehran and Sannandaj (18, 19). Furthermore, in studies done in Tehran as well as Germany, confidentiality and dignity had the best ranks in term of performance respectively (4, 14, 20). However, unfortunately, the trend of these dimensions has been declining from 2003 to 2015. Perhaps one of the reasons for this decline is the high pressure on health personnel that has been created due to the increased load of referrals, which is the consequence of the implementation of the HTP.
The worst performing domains in outpatient services were choice and prompt attention. This finding (worst of choice in terms of performance) is in line with the study done in Germany (20). It is notable that our study population is in a low socio-economic level district of Tehran and has less opportunity for choice health care providers due to the fact that they are less likely to live/work in this area. However, health system responsiveness in choice is improved as time passes. Perhaps one of the reasons for this improvement is the implementation of HTP in Iran and supporting the retention of physicians in deprived areas since 2014. This makes patients more free to choose a health care provider.
In this study, most respondents (89%) selected prompt attention as the most important domain, while the lowest score was in terms of performance. In addition, in a study on health system responsiveness among older adults in South Africa, prompt attention was the greatest concern of service users (21). Although prompt attention has increased compared to the previous period in 2015. One of the reasons for this increase could be the implementation of the HTP and increase access to healthcare as a result of reduced waiting and traveling times.
In inpatient services, confidentiality had the best performance score. This finding is in line with the findings of several studies (3, 4, 22, 23).
As with other previous studies in Iran (3-5, 24), autonomy has had the lowest score in 3 periods, however, fortunately, it has an increasing trend. Therefore, it is necessary that health care providers inform patients about other types of treatments and involve them in the decision making about their care to achieve a higher score in the autonomy.
As seen in this research, in outpatient and inpatient services, private centers were better than public centers in all aspects during the study. This finding was similar to the reports of other previous studies (9, 25-27). Therefore; public hospitals must compete to private hospitals in terms of good service delivery. Implementation of HTP packages including the presence of specialist physicians residing in public hospitals, improvement of hoteling quality and improving the quality of visiting services, as well as provide potential capability for public hospitals to improve their responsiveness by proper utilization of them. However, most participants used public services for outpatient and inpatient care. Given the low socio-economic status of district, it seems that implementation of HTP and reduction in out of pocket payment and improving geographical access, could be a main factor for using public services despite the better performance of private centers.
In this study PCA found that responsiveness in outpatient and inpatient services was included as a major factor in all dimensions of the WHO model.
In a study done in Taiwan, PCA produced 5 factors (respect, access, confidentiality, basic amenities, and social support) that explained 63.5% of the total variances (7). Studies in South Africa and Iran showed different clustering patterns of responsiveness (12, 21). For example, “autonomy” in these studies was not conceptualized as a unique domain. Further studies are required to find the structure of health systems responsiveness domains in the developing countries.
4.1. Conclusions
Based on the results, overall responsiveness level in inpatient and outpatient services has increased. Although it cannot be commented definitively, this can be due to the implementation of HTP supportive packages. Due to the fact that one of the final objectives of the HTP is to increase responsiveness, the interaction of patients and service providers is a topic that has been less addressed by health sector reforms. In order to increase responsiveness, it is suggested that some reforms (for example: training staff about confidentiality of personal information, privacy, talking to patients etc.) be made alongside such plans as the HTP.
Acknowledgements
References
-
1.
Malhotra C, Do YK. Socio-economic disparities in health system responsiveness in India. Health Policy Plan. 2013;28(2):197-205. [PubMed ID: 22709921]. https://doi.org/10.1093/heapol/czs051.
-
2.
Robone S, Rice N, Smith PC. Health systems' responsiveness and its characteristics: a cross-country comparative analysis. Health Serv Res. 2011;46(6pt2):2079-100. [PubMed ID: 21762144]. https://doi.org/10.1111/j.1475-6773.2011.01291.x.
-
3.
Ebrahimipour H, Vafaei Najjar A, Khani Jahani A, Pourtaleb A, Javadi M, Rezazadeh A, et al. Health system responsiveness: a case study of general hospitals in iran. Int J Health Policy Manag. 2013;1(1):85-90. [PubMed ID: 24596841]. https://doi.org/10.15171/ijhpm.2013.13.
-
4.
Karami-Tanha F, Moradi-Lakeh M, Fallah-Abadi H, Nojomi M. Health system responsiveness for care of patients with heart failure: evidence from a university hospital. Arch Iran Med. 2014;17(11):736-40. [PubMed ID: 25365611].
-
5.
Rashidian A, Kavosi Z, Majdzadeh R, Pourreza A, Pourmalek F, Arab M, et al. Assessing health system responsiveness: a household survey in 17th district of tehran. Iran Red Crescent Med J. 2011;13(5):302-8. [PubMed ID: 22737485].
-
6.
Rottger J, Blumel M, Fuchs S, Busse R. Assessing the responsiveness of chronic disease care - is the World Health Organization's concept of health system responsiveness applicable? Soc Sci Med. 2014;113:87-94. [PubMed ID: 24852659]. https://doi.org/10.1016/j.socscimed.2014.05.009.
-
7.
Hsu CC, Chen L, Hu YW, Yip W, Shu CC. The dimensions of responsiveness of a health system: a Taiwanese perspective. BMC Public Health. 2006;6:72. [PubMed ID: 16542462]. https://doi.org/10.1186/1471-2458-6-72.
-
8.
Jones AM, Rice N, Robone S, Dias PR. Inequality and polarisation in health systems' responsiveness: a cross-country analysis. J Health Econ. 2011;30(4):616-25. [PubMed ID: 21696839]. https://doi.org/10.1016/j.jhealeco.2011.05.003.
-
9.
Arab M, Rahimi-Foroushani A, Akbari Sari A, Khammarnia M, Sadeghi A, Siavashi E. Comparison of Responsiveness Rate among Private and Social Security Hospitals in Tehran City. Hospital. 2012;14(4):29-39.
-
10.
Piroozi B, Moradi G, Nouri B, Mohamadi Bolbanabad A, Safari H. Catastrophic Health Expenditure After the Implementation of Health Sector Evolution Plan: A Case Study in the West of Iran. Int J Health Policy Manag. 2016;5(7):417-23. [PubMed ID: 27694669]. https://doi.org/10.15171/ijhpm.2016.31.
-
11.
Iran Statistics Center. National population and housing census 2011. Tehran; 2011.
-
12.
Askari R, Arab M, Rashidian A, Akbari-Sari A, Hosseini SM, Gharaee H. Designing Iranian Model to Assess the Level of Health System Responsiveness. Iran Red Crescent Med J. 2016;18(3). e24527. [PubMed ID: 27247795]. https://doi.org/10.5812/ircmj.24527.
-
13.
Dormohammadi T, Asghari F, Rashidian A. What do patients expect from their physicians? Iran J Public Health. 2010;39(1):70-7. [PubMed ID: 23112992].
-
14.
Forouzan S, Padyab M, Rafiey H, Ghazinour M, Dejman M, San Sebastian M. Measuring the Mental Health-Care System Responsiveness: Results of an Outpatient Survey in Tehran. Front Public Health. 2015;3:285. [PubMed ID: 26858944]. https://doi.org/10.3389/fpubh.2015.00285.
-
15.
Valentine NB, Bonsel GJ, Murray CJ. Measuring quality of health care from the user's perspective in 41 countries: psychometric properties of WHO's questions on health systems responsiveness. Qual Life Res. 2007;16(7):1107-25. [PubMed ID: 17624815]. https://doi.org/10.1007/s11136-007-9189-1.
-
16.
Mohammed S, Bermejo JL, Souares A, Sauerborn R, Dong H. Assessing responsiveness of health care services within a health insurance scheme in Nigeria: users' perspectives. BMC Health Serv Res. 2013;13:502. [PubMed ID: 24289045]. https://doi.org/10.1186/1472-6963-13-502.
-
17.
Liabsuetrakul T, Petmanee P, Sanguanchua S, Oumudee N. Health system responsiveness for delivery care in Southern Thailand. Int J Qual Health Care. 2012;24(2):169-75. [PubMed ID: 22215759]. https://doi.org/10.1093/intqhc/mzr085.
-
18.
Sajjadi F, Moradi-Lakeh M, Nojomi M, Baradaran HR, Azizi F. Health system responsiveness for outpatient care in people with diabetes Mellitus in Tehran. Med J Islam Repub Iran. 2015;29:293. [PubMed ID: 26913256].
-
19.
Piroozi B, Mohamadi Bolban Abad A, Moradi GH. Assessing health system responsiveness after the implementation of health system reform: a case study of Sanandaj, 2014-2015. Iran J Epidemiol. 2016;11(4):1-9.
-
20.
Bramesfeld A, Wedegartner F, Elgeti H, Bisson S. How does mental health care perform in respect to service users' expectations? Evaluating inpatient and outpatient care in Germany with the WHO responsiveness concept. BMC Health Serv Res. 2007;7:99. [PubMed ID: 17605786]. https://doi.org/10.1186/1472-6963-7-99.
-
21.
Peltzer K, Phaswana-Mafuya N. Patient experiences and health system responsiveness among older adults in South Africa. Glob Health Action. 2012;5:1-11. [PubMed ID: 23195515]. https://doi.org/10.3402/gha.v5i0.18545.
-
22.
Valentine N, Verdes-Tennant E, Bonsel G. Health systems' responsiveness and reporting behaviour: Multilevel analysis of the influence of individual-level factors in 64 countries. Soc Sci Med. 2015;138:152-60. [PubMed ID: 26093073]. https://doi.org/10.1016/j.socscimed.2015.04.022.
-
23.
Valentine NB, Lavallee R, Liu B, Bonsel GJ, Murray CJL. Classical Psychometric Assessment of the Responsiveness Instrument in the WHO Multicountry Survey Study on Health and Responsiveness 2000-2001. In: Christopher J. L. Murray DB, editor. Health Systems Performance Assessment: Debates, methods and Empiricism. WHO; 2001. p. 616-20.
-
24.
Najafi F, Karami-Matin B, Rezaei S, Rajabi-Gilan N, Soofi M. Health system responsiveness after health sector evolution plan (HSEP): An inpatient survey in Kermanshah in 2015. Med J Islam Repub Iran. 2016;30:387. [PubMed ID: 27493931].
-
25.
Peltzer K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv Res. 2009;9:117. [PubMed ID: 19602290]. https://doi.org/10.1186/1472-6963-9-117.
-
26.
Mosallam RA, Aly MM, Moharram AM. Responsiveness of the health insurance and private systems in Alexandria, Egypt. J Egypt Public Health Assoc. 2013;88(1):46-51. [PubMed ID: 23528532]. https://doi.org/10.1097/01.EPX.0000427042.54093.c4.
-
27.
Bazzaz MM, Taghvaee MR, Salehi M, Bakhtiari M, Shaye ZA. Health System's Responsiveness of Inpatients: Hospitals of Iran. Glob J Health Sci. 2015;7(7 Spec No):106-13. [PubMed ID: 26153210]. https://doi.org/10.5539/gjhs.v7n7p106.