Abstract
Background:
Resource allocation is one of the major challenges of health systems. Various criteria are used to allocate health resources worldwide.Objectives:
The current study aimed to identify and prioritize key factors related to the resource allocation in the health sector of the Iranian Oil Industry using the Decision-Making Trial and Evaluation Laboratory (DEMATEL) method.Methods:
This cross-sectional case study was conducted in two main phases during 2017. In the first phase, the literature review and interviews with experts (n = 6) were used to identify initial criteria for resource allocation. Then, considering the views of high and middle managers in the health sector of the Iranian Oil Industry, the final criteria were selected. In the second phase, the DEMATEL technique was used to assess the interactions among the selected criteria.Results:
A total of nine criteria were entered into the DEMATEL final questionnaire. Criteria were divided into two main groups of influencing and influenced factors. The high-level documents and general policies of the health system (C1), the burden of diseases (C2), the number of population covered (C4), the infrastructure of the covered regions (C5), and population health needs (C8) were among factors that influenced other factors. Factors such as current budget (C3), the expected benefits of people (C6), the expected benefits of policymakers (C7), and the financial returns of the resource allocation (C9) were among the factors that were influenced by other factors. The number of covered population (C4) and the infrastructure of the regions (C5) were not influenced by other factors but could affect other factors. High-level documents (C1) and the burden of diseases (C2) were identified as independent factors.Conclusions:
While allocating resources, policymakers should pay particular attention to influencing factors. The number of population covered in each region and the infrastructure available in each region were identified as key and important criteria in the resource allocation process. It is suggested that these factors be considered while allocating resources to different regions of the country.Keywords
1. Background
The scarcity of resources, along with increased demand for health services are among the main challenges that health systems face worldwide (1, 2). This is a major challenge in maximizing the health of individuals, which is an important goal for the health systems (3). Hence, the decision on how to allocate resources is of crucial importance (4, 5). Meanwhile, resource allocation is one of the most controversial issues that health policymakers are dealing with (4, 6). Meeting the real needs of the population is an important goal of resource allocation within the health sector (7). The allocation of health resources is a complex process that affects various factors (6, 8). To allocate resources within the health system, several factors should be considered such as cost-effectiveness (9, 10), cost of interventions, budget impact and policy directions (11), ability to pay (10), fairness/equality, interests of different groups of stakeholders (9), equity (4, 10), number of potential beneficiaries (10), the severity of illness and socioeconomic status of patients (12), needs (9, 11), and the availability of human resources and local capacities (4). Maintaining a balance between these various factors and objectives, while involving various stakeholders, is so important. Besides, resource allocation certainly has a substantial impact on the health outcomes of the community. Meanwhile, considering that health is a public good or a universal right, the allocation of health resources composes many social and ethical responsibilities for health policymakers (2).
Despite their importance, decisions about resource allocation are usually made implicitly based on limit criteria. At the macro level, the allocation of health resources is usually based on the historical pattern of resource allocation and the bargaining power of various stakeholders or regions, which led to an increased role of explicit approaches, including decision-making techniques, in the process of resource allocation during the recent years. Therefore, the use of multi-criteria decision-making methods can help to increase transparency in the resource allocation process and to ensure its fairness and effectiveness. One of the techniques widely applied to solve such complex problems is the Decision-Making Trial and Evaluation Laboratory (DEMATEL) technique, developed between 1972 and 1976 by the Battelle Memorial Institute of Geneva (13, 14). DEMATEL is a mathematical multi-criteria approach that analyzes the relationships between a set of factors and attempts to identify causal relationships among them (15). Globally, different studies used this technique to solve health problems at various levels (6, 16-24). For instance, this technique alone or combined with other methods is used to identify key factors influencing the quality of hospital services, developing strategies for improving the performance of general hospitals (17), identifying key performance indicators for hospital management (18), to select allied hospitals in outpatient services (22), to analyze associations and to prioritize the social factors affecting health (23), and to prioritize the compensation mechanisms for nurses working in the emergency department (24). Multi-criteria decision-making methods are useful in making clear and transparent decisions. Using multi-criteria approaches is useful for decision-makers to systematically capture their concerns, compare value trade‐offs, and elicit their value preferences (2). In the current study, a multivariate decision-making model was applied to investigate how such approaches can be used to solve complex problems, including rational resource allocation, which may contribute to more efficient, rational, and legitimate resource allocation decisions.
It seems that there is no comprehensive and evidence-based method for allocating health resources in different geographic regions of Iran. Long-term use of traditional methods such as bargaining and historical patterns has led to increased inequity in the distribution of resources as well as misuse of limited resources of the Iranian health system. The health sector of the Iranian Oil Industry is an independent body that is responsible for the provision of healthcare services to the Oil industry’s employees and their families across the country (almost 800,000 people) through a network of hospitals and health facilities. The allocation of resources in the health sector of the Iranian Oil Industry is faced with several challenges that are similar to those of the national health system and have not been addressed yet.
2. Objectives
To provide information to solve such problems, the present study aimed to identify and prioritize the key factors related to the allocation of resources in the health sector of the Iranian Oil Industry using the DEMATEL method.
3. Methods
The current cross-sectional study, which was conducted in two phases during 2017 applied qualitative and quantitative methods for data collection. In the first step, a literature review was conducted and a series of interviews were performed with experts. At this step, the primary resources allocation criteria were defined, and then, using the opinions of the top and middle-level managers of the healthcare sector of Iran’s Oil Industry, final criteria were selected. In the second phase, the DEMATEL technique was used to examine the interaction between the criteria and to prioritize them.
3.1. Phase I: Selecting Criteria
In this phase, first, through a systematic review, which was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyzes) guideline, the effective measures on resource allocation were identified. Cochrane, PubMed, and SCOPUS databases were systematically searched from 2005 to 2016 to identify articles that reported criteria for resource allocation in the health sector (25). Then, the identified criteria were reviewed by experienced health experts to discuss their similarities and identify conceptual overlap among them. To identify experts, the purposeful sampling technique was used. In total, eight experts were identified, and finally, six of them accepted to participate in the study. Among them, there were high-level managers in budgeting and financial organizations (such as executive officers, executive officer vice-chancellors, financial officers, financial officer vice-chancellors, development officers, development officer vice-chancellors, strategic purchasing officers, and strategic purchasing officer vice-chancellors) from the health sector of the Iranian oil industry with at least five years of experience in budgeting and financial management. All participants were male and their mean age was 38. After obtaining expert opinions, a questionnaire was designed to prioritize all criteria and to select the most important ones to be included in the final phase of the study. Then, the questionnaire was distributed among 250 financial managers with relevant experience (with more than two years of experience), considering the organizational chart of the Oil Industry healthcare sector. The questionnaire contained 19 criteria and the respondents were asked to prioritize them using a five-point Likert scale ranging from 0 (i.e., least important) to 4 (‘the most important’). After calculating the relative importance of each criterion, the research team reviewed the results and the final list of the criteria was approved to be used in the final phase of the study.
3.2. Phase II: DEMATEL Technique
Based on the final list of criteria, the DEMATEL questionnaire was developed and presented to the 15 members of the expert group on resource-allocation and decision-making. Experts were asked to evaluate the impact of each criterion on other criteria using pairwise comparison. The steps of the DEMATEL technique were as follows (6, 13, 16):
3.2.1. Developing a Direct-Relation Matrix
To assess the internal impact of the identified factors, experts were asked to determine the effect of the factors in each row (factor i) on other factors of each column (factor j) using a five-point Likert scale (0: “No influence”, 1: “low influence”, 2: “medium influence”, 3: “high influence” and 4: “very high influence”). The D direct relation matrix was calculated using the mean scores.
3.2.2. Calculating the Normalized Direct-Relation Matrix
The Mean Normalized Matrix (N) was defined as N = k × D, which D was direct relation matrix and k was the reverse of the sum of the largest number of rows or columns of matrix D. Which was obtained by the following formula:
3.2.3. Calculating the Total-Relation Matrix
The complete relation matrix (T) was obtained from the direct relation normal matrix (N) and the matrix of the unit (I) as follows: T = N × (I-N) ^ (-1). This matrix calculates the overall impact of each factor over others and vice versa. It serves as a basis for determining the overall degree of influence of each criterion as well as its importance.
In the relation matrix (T), the sum of the rows (r) represents the effect of a criterion over other criteria, and the sum of the columns (c) represents the extent to which a criterion influences by other criteria. r + c represents the degree of importance that this criterion, among the total criteria, has in solving the problem. r - c shows the degree of impact of a criterion among the total criteria. r - c being positive indicates the criterion has an impact on others and the r - c being negative indicates the criterion affects by other criteria. If r - c > 0, the criterion is more influencing rather than being affected.
3.2.4. Setting up a Threshold Value and Obtaining the Impact-Digraph Map
Each value of the T matrix provides information on how each criterion affects others. If all information of the T-matrix is converted to an impact-digraph map, the map will be very complex to provide the required information for decision making. Therefore, it is necessary to determine the threshold value by decision-makers to demonstrate major effects and to eliminate the minor effects of the criteria. Only some of the criteria that their impact level on the matrix T is higher than the threshold should be selected and will be demonstrated on the map. The threshold value was obtained through discussions between experts or by calculating the mean values of the matrix T.
4. Results
4.1. Phase I: Selecting the Criteria
In total, 20 criteria in four main categories were identified through systematic review, which are as follow: (1) economic criteria, including cost-effectiveness, cost of the interventions, value of money, budget impact; (2) managerial criteria, including poverty reduction, financial protection, national priority, responsiveness, equity and equality, donors’ participation, leadership style, stakeholders’ power; (3) contextual criteria, including disease severity, the burden of disease, potential caregivers and vulnerable groups, socioeconomic factors, age, race, gender, racial and ethnic groups; and (4) structural criteria, including need, and local capacity (24). Subsequently, these criteria were given to the six experts for further investigation. The experts expressed their opinions by removing/revising a criterion or suggesting new criteria. After applying the experts’ comments and aggregating their views, 19 criteria were selected and used in the next steps, which were as follow: high-level documents and general policies of the health system, number of population covered in different regions, burden of diseases, current total budget, responding to population health needs, the number of the vulnerable population, financial protection, infrastructure and equipment of various regions, the age of target groups, disease severity, fairness and equity, the expected benefits of people/patients, donors’ participation, health workforce, the expected benefits of policymakers, degree of underdevelopment of different regions, health needs of different regions, economic status of covered regions, and cost-benefit (financial return). Then, 250 experts were asked to prioritize the selected criteria using a questionnaire, of which 211 returned the questionnaire (response rate = 84.5%). Since the high number of criteria caused difficulties for respondents while pairwise comparison, they were resubmitted to the experts to obtain a shortened list. After calculating the importance of criteria, eventually, nine criteria were selected for the final phase of the study, of which their importance was more than 75%, (Table 1).
The Criteria Included in the Modeling and Their Symbol in the DEMATEL Technique
| Criteria | Definition |
|---|---|
| C1 | High-level documents and general policies of the health system |
| C2 | The burden of diseases |
| C3 | Current total budget |
| C4 | Number of population covered in different regions |
| C5 | Infrastructure and equipment in the regions |
| C6 | The expected benefits of people / patients |
| C7 | The expected benefits of policymakers |
| C8 | Population health needs in the region |
| C9 | Cost-benefit (financial return) due to resource allocation |
4.2. Phase II: DEMATEL Technique
The DEMATEL questionnaire, which was developed based on the final list of criteria, was presented to 15 experts with expertise in resource allocation decision-making. The questionnaire designed for pairwise comparison to evaluate the influence of each score, where scores of 0, 1, 2, 3 and 4 represent: (no influence), (very low influence), (low influence), (high influence), and (very high influence), respectively. The calculations of the DEMATEL method were performed based on the views of the experts and the results are as follows:
1. D direct-relation matrix, which was obtained using experts’ views, is presented in Table 2. The C8 criterion had a great impact on the C4 criterion, the C7 criterion was slightly affected by C9 c, and the impact of the C3 criterion on C9 was almost modest.
The Direct-Relation Matrix, D
| Criteria’s | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | Sum |
|---|---|---|---|---|---|---|---|---|---|---|
| C1 | 0.000 | 0.333 | 0.417 | 0.583 | 0.250 | 0.500 | 0.417 | 0.500 | 0.250 | 3.250 |
| C2 | 0.083 | 0.000 | 0.500 | 0.250 | 0.333 | 2.250 | 1.500 | 0.667 | 0.500 | 6.083 |
| C3 | 0.250 | 0.750 | 0.000 | 0.167 | 1.333 | 1.750 | 2.250 | 1.250 | 1.500 | 9.250 |
| C4 | 0.167 | 0.917 | 2.083 | 0.000 | 1.500 | 2.917 | 2.167 | 3.000 | 2.000 | 14.750 |
| C5 | 0.083 | 0.667 | 1.500 | 0.083 | 0.000 | 1.750 | 1.750 | 2.000 | 1.750 | 9.583 |
| C6 | 0.750 | 0.583 | 1.500 | 0.500 | 0.917 | 0.000 | 1.917 | 1.250 | 0.917 | 8.333 |
| C7 | 0.417 | 0.500 | 2.000 | 0.417 | 0.667 | 2.417 | 0.000 | 1.250 | 1.000 | 8.667 |
| C8 | 0.250 | 0.917 | 1.833 | 0.250 | 0.917 | 2.833 | 2.750 | 0.000 | 1.417 | 11.167 |
| C9 | 0.167 | 0.417 | 2.000 | 0.182 | 0.750 | 1.250 | 1.833 | 1.250 | 0.000 | 7.848 |
| Sum | 2.167 | 5.083 | 11.833 | 2.432 | 6.667 | 15.667 | 14.583 | 11.167 | 9.333 | - |
2. The Mean Normalized Matrix (N) was obtained by normalizing the mean matrix. The largest number of rows and columns in the D matrix was 15.667 and its reverse was 0.0638. By multiplying this number in the D matrix, the normal matrix N was obtained (Table 3).
The Normalized Direct-Relation Matrix, N
| Criteria’s | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | Sum |
|---|---|---|---|---|---|---|---|---|---|---|
| C1 | 0.000 | 0.021 | 0.027 | 0.037 | 0.016 | 0.032 | 0.027 | 0.032 | 0.016 | 0.207 |
| C2 | 0.005 | 0.000 | 0.032 | 0.016 | 0.021 | 0.144 | 0.096 | 0.043 | 0.032 | 0.388 |
| C3 | 0.016 | 0.048 | 0.000 | 0.011 | 0.085 | 0.112 | 0.144 | 0.080 | 0.096 | 0.590 |
| C4 | 0.011 | 0.059 | 0.133 | 0.000 | 0.096 | 0.186 | 0.138 | 0.191 | 0.128 | 0.941 |
| C5 | 0.005 | 0.043 | 0.096 | 0.005 | 0.000 | 0.112 | 0.112 | 0.128 | 0.112 | 0.612 |
| C6 | 0.048 | 0.037 | 0.096 | 0.032 | 0.059 | 0.000 | 0.122 | 0.080 | 0.059 | 0.532 |
| C7 | 0.027 | 0.032 | 0.128 | 0.027 | 0.043 | 0.154 | 0.000 | 0.080 | 0.064 | 0.553 |
| C8 | 0.016 | 0.059 | 0.117 | 0.016 | 0.059 | 0.181 | 0.176 | 0.000 | 0.090 | 0.713 |
| C9 | 0.011 | 0.027 | 0.128 | 0.012 | 0.048 | 0.080 | 0.117 | 0.080 | 0.000 | 0.501 |
| Sum | 0.138 | 0.324 | 0.755 | 0.155 | 0.426 | 1.000 | 0.931 | 0.713 | 0.596 | - |
3. The complete relation matrix is as follows (Table 4):
The Total Relation Matrix, T
| Criteria’s | C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | Sum |
|---|---|---|---|---|---|---|---|---|---|---|
| C1 | 0.010 | 0.041 | 0.073 | 0.046 | 0.043 | 0.089 | 0.082 | 0.072 | 0.052 | 0.508 |
| C2 | 0.027 | 0.035 | 0.116 | 0.034 | 0.068 | 0.232 | 0.187 | 0.110 | 0.092 | 0.901 |
| C3 | 0.044 | 0.097 | 0.127 | 0.036 | 0.148 | 0.254 | 0.277 | 0.178 | 0.182 | 1.344 |
| C4 | 0.056 | 0.141 | 0.326 | 0.041 | 0.205 | 0.416 | 0.372 | 0.344 | 0.272 | 2.172 |
| C5 | 0.035 | 0.095 | 0.221 | 0.032 | 0.074 | 0.262 | 0.261 | 0.224 | 0.201 | 1.406 |
| C6 | 0.070 | 0.083 | 0.201 | 0.054 | 0.119 | 0.140 | 0.245 | 0.169 | 0.141 | 1.222 |
| C7 | 0.053 | 0.081 | 0.233 | 0.050 | 0.110 | 0.281 | 0.144 | 0.173 | 0.150 | 1.275 |
| C8 | 0.051 | 0.116 | 0.256 | 0.047 | 0.139 | 0.341 | 0.333 | 0.123 | 0.193 | 1.598 |
| C9 | 0.035 | 0.072 | 0.226 | 0.034 | 0.108 | 0.208 | 0.238 | 0.164 | 0.083 | 1.169 |
| Sum | 0.383 | 0.761 | 1.779 | 0.375 | 1.013 | 2.224 | 2.139 | 1.557 | 1.365 |
Based on Table 4, the C6 was the most important criteria with the highest r + c (3.415), whereas C1 was the least important criteria with the lowest value r + c (0.891). Based on the values of r + c, the importance of the nine selected criteria was C6 > C7 > C8 > C3 > C4 > C9 > C5 > C2 > C1, respectively. Based on the r - c column, the criteria were divided into two groups: influencing and influenced factors. Positive r - c values were considered as influencing criteria that directly affect other criteria. The negative value of r - c was an influenced factor that was directly affected by other factors. C1, C2, C4, C5 & C8 were among influencing criteria and C3, C6, C7, and C9 criteria were among the influenced factors (Table 5).
The Direct and Indirect Effects of the Criteria
| Criteria’s | r | c | r + c | Rank | r - c | Impact |
|---|---|---|---|---|---|---|
| C1: high-level document and general policies of the health system | 0.508 | 0.383 | 0.891 | 9 | 0.125 | Cause |
| C2: burden of disease | 0.901 | 0.761 | 1.663 | 8 | 0.140 | Cause |
| C3: current budget | 1.344 | 1.779 | 3.123 | 4 | -0.436 | Effect |
| C4: health needs | 2.172 | 0.375 | 2.547 | 5 | 1.798 | Cause |
| C5: infrastructure | 1.406 | 1.013 | 2.419 | 7 | 0.394 | Cause |
| C6: expected benefit by people | 1.222 | 2.224 | 3.446 | 1 | -1.002 | Effect |
| C7: expected benefit by policymakers | 1.275 | 2.139 | 3.415 | 2 | -0.864 | Effect |
| C8: number of the covered population | 1.598 | 1.557 | 3.156 | 3 | 0.041 | Cause |
| C9: financial return | 1.169 | 1.365 | 2.534 | 6 | -0.196 | Effect |
4. To limit the data obtained from the DEMATEL method (Table 5), after calculating the mean values of the full-matrix relation (T) and having experts’ opinions, the value of 0.250 was determined as a threshold value and the impact-digraph map was plotted (Figure 1).
Causality diagram of criteria
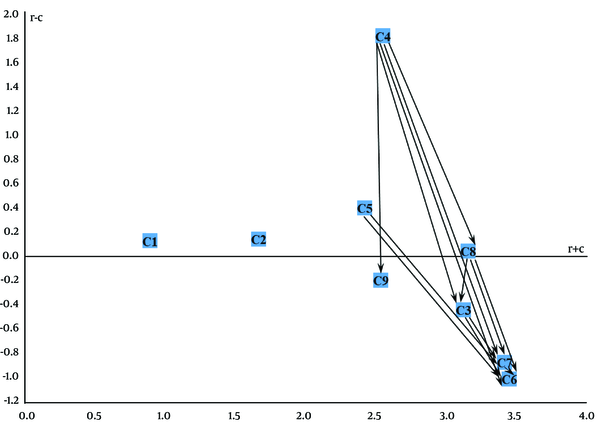
The digraph shows that the C4 was not affected by other criteria, but it had an impact on the C8, C9, C3, C7, and C6 criteria. The C5 was not influenced by other criteria, similar to C4, but it affected the C7 and C6. The criteria C1 and C2 were independent of other criteria. Taken together, when allocating resources, policymakers should pay particular attention to influencing criteria (C4, C5, C2, C8 & C1). The criteria C4 and C5 were regarded as important and key criteria, since not only they were influential criteria but also were not affected by other criteria.
5. Discussion
All around the world, health systems face resource scarcity. Therefore, equitable allocation of resources is one of the main challenges of any health care system. In health sector decisions regarding the resource allocation and priority setting are usually implicit and without clear criteria in practice, which is increasingly recognized as unacceptable (26). The priority setting requires clear and explicit criteria to make fair and transparent decisions (27). Decisions related to resource allocation should be made based on the best available information. However, due to the inaccessibility of appropriate and on-time information, decisions associated with resource allocation in many developing countries often make implicitly, rather than using explicit consideration of the risks and benefits of alternative options (28). Like other developing countries, Iran is also facing several health challenges such as limited resources of the health sector, increasing demand for health services due to increased awareness of the population, demographic changes, aging of the population, and the advent of advanced technologies. Therefore, priority setting is of great importance. However, relevant studies indicated that most decisions on priority setting of health interventions are made implicitly (29). The present study aimed to identify and evaluate the key factors related to resource allocation in the health system of the Iranian oil system using the DEMATEL method. Using this method, nine criteria were recognized as the most important factors in resource allocation, and the causal relationships among them were identified.
Various economic, managerial, contextual, and structural factors can be used as criteria for resource allocation in the health sector. The findings showed that high-level documents and general policies of the health system, burden of diseases, number of population covered, the infrastructure of the region, and the health needs of the population (C1, C2, C8, C5, and C4) were among influencing factors. Also, factors such as the expected benefits of the people, the expected benefits of policymakers, the current budget, and the financial returns of the allocated resources (C6, C7, C3, and C9) were recognized as the influenced factors. In general, the health needs of the population (C8) and the high-level documents and general policies of the health system (C1) were factors with the least impact. The needs of the population (C4) and the infrastructure of the regions (C5) had the highest impact on other criteria. The health needs of the population (C4) had the most impact on the expected benefits of the people (C6).
Cost-related factors have a high influence on resource allocation decisions. Currently, cost-effectiveness is the most popular criteria used for resource allocation decisions. It is widely used in countries such as Australia, Canada, Switzerland, and the UK. It is described as a determinant factor in the development of the basic health services package or benefits package in the UK, Germany, and Switzerland (23). In Australia, it is widely used for resource allocation and economic assessment (24). In the current study, similar to previous studies, the financial returns of the allocated resources (C9) were identified as an effective factor.
High-level documents and general policies of the health system (C1), the expected benefits of people (C6), and the expected benefits of policymakers (C7), which are among managerial factors, were entered into the final model. National priorities and general health policies have been referred to determining criteria in designing health benefits package in the UK, Switzerland, and Germany (23). These factors are also reported identified in other similar studies (6), as one of the most important criteria used in resource allocation and decision-making (30).
The burden and prevalence of diseases are among the most influential criteria for allocating health resources. All around the world, policymakers consider the severity of illness as an important criterion for prioritizing (31). The burden of diseases, which includes the most important causes of death and disability, is a highly valuable indicator for planning health interventions. It can provide the most important evidence needed for evidence-based policy-making. Therefore, it seems that identifying the leading causes of the burden of diseases in different regions can be an effective step for health resources allocation. In the present study, the two criteria of the burden of diseases (C2) and the number of covered people (C8) were among the most important criteria identified for resource allocation. The results of the current study are consistent with those of a study conducted in Thailand that described the main criteria of prioritizing health interventions in developing countries, and a study conducted in Mexico, which identified the burden of diseases as an important criterion for prioritizing health interventions (32, 33). The number of covered population is reported as an important criterion to prioritize health interventions in the Netherlands, Norway, Ghana, Thailand, and Iran.
Allocating resources based on health needs can improve public health and reduce inequity in different geographic areas, which is one of the important responsibilities of health systems (7). The findings of this study showed that the health needs of the population (C4) are a very important factor that should be considered while allocating health resources. Health needs are an important criterion for allocating health resources and making health-related decisions worldwide (9). The health needs are one of the determining criteria for developing the benefits package in the UK, Germany, and Switzerland. This criterion uses in Australia for allocating health resources and economic assessment in the health system. Also, the health system of the Netherlands uses this criterion in a wide range of health interventions (34). England, Wales, and Scotland also use a needs-based approach to allocate health resources (35). In Wales, first, the entire health budget distributes between various health services programs and then distributes among different geographical areas according to the specific health needs of each region. In Scotland, a combination of direct and indirect indicators uses to allocate resources based on health needs.
The availability of infrastructure and equipment is another important criterion that uses for the allocation of health resources (6). In Ghana, the availability of human resources for health and local capacities to use financial resources are factors that affect equality in the allocation of health resources (4). In the Netherlands, among the factors that use for priority setting of health interventions, availability of health workforce, information, and technology are the most important ones (36). In the present study, it (C5) was identified as an important criterion that affects the resource allocation process. The results of the current study are consistent with studies that reported the health needs as a criterion to prioritize the allocation of resources in the UK, Germany, Switzerland, Australia, and the Netherlands (6, 24, 25).
5.1. Limitations
Like other studies the current study also had limitations. Although the criteria used to allocate resources were identified through literature review and interviews, it should be acknowledged that the criteria used to allocate health resources in each country are unique. Therefore, countries need to use a set of criteria based on their context and circumstances. Besides, despite some common polices, the health sector of the Iranian Oil Industry has its own rules and regulations, and consequently, the results may not be completely generalizable to entire Iran’s health system. However, due to the similarity of the context, it seems that similarities are more than differences.
5.2. Conclusion
When allocating resources to different geographical regions of the country, health policymakers should pay special attention to several factors, including the health needs of the regions, the infrastructure of the regions, the burden of diseases, the number of covered populations, and the high-level health documents. It is strongly recommended that the current pattern of resource allocation, which is based on the historical budget of each region and/or the bargaining power of local authorities, be substituted with a more rational approach through using appropriate criteria. Multi-criteria decision-making methods are useful in making clear and transparent decisions. In this study, a multivariate decision-making model was used for the allocation of health resources. The results of the current study showed that the DEMATEL technique can be used in health care decision makings. However, to facilitate organizational adoption of DEMATEL, as an alternative decision-making process, further research is required to develop strategies for implementation, as well as to drive key methodological aspects of the process.
Acknowledgements
References
-
1.
Sabik LM, Lie RK. Priority setting in health care: Lessons from the experiences of eight countries. International Journal for equity in health. 2008;7(1):4.
-
2.
Angelis A, Kanavos P, Montibeller G. Resource Allocation and Priority Setting in Health Care: A Multi‐criteria Decision Analysis Problem of Value? Global Policy. 2017;8:76-83.
-
3.
Shah KK. Severity of illness and priority setting in healthcare: a review of the literature. Health policy. 2009;93(2-3):77-84.
-
4.
Asante AD, Zwi AB. Factors influencing resource allocation decisions and equity in the health system of Ghana. Public Health. 2009;123(5):371-7.
-
5.
Barasa EW, Molyneux S, English M, Cleary S. Setting healthcare priorities in hospitals: a review of empirical studies. Health policy and planning. 2014;30(3):386-96.
-
6.
Guindo LA, Wagner M, Baltussen R, Rindress D, van Til J, Kind P, et al. From efficacy to equity: Literature review of decision criteria for resource allocation and healthcare decisionmaking. Cost effectiveness and resource allocation. 2012;10(1):9.
-
7.
Yousefi M, Akbari SA, Arab M, Oliaeemanesh A. Methods of resource allocation based on needs in health systems, and exploring the current Iranian resource allocation system. Hakim Research Journal. 2010;13(2):80-90.
-
8.
Jouyani Y, Palangi HS, Rahimnia R. Identifying the Criteria affecting Appropriate Allocation of Health System Resources to Different Diseases in Iran: A Qualitative inquiry. Health Scope.
-
9.
Lin C, Tzeng G. A value-created system of science (technology) park by using DEMATEL. Expert systems with applications. 2009;36(6):9683-97.
-
10.
Lee Y, Li M, Yen T, Huang T. Analysis of adopting an integrated decision making trial and evaluation laboratory on a technology acceptance model. Expert Systems with Applications. 2010;37(2):1745-54.
-
11.
Kumar A, Kaviani MA, Bottani E, Dash MK, Zavadskas EK. Investigating the role of social media in polio prevention in India: a Delphi-DEMATEL approach. Kybernetes. 2018;47(5):1053-72.
-
12.
Shieh J, Wu H, Huang K. A DEMATEL method in identifying key success factors of hospital service quality. Knowledge-Based Systems. 2010;23(3):277-82.
-
13.
Rahimi H, Bahmaei J, Shojaei P, Kavosi Z, Khavasi M. Developing a strategy map to improve public hospitals performance with balanced scorecard and dematel approach. Shiraz E-Medical Journal. 2018;19(7).
-
14.
Si S, You X, Liu H, Huang J. Identifying key performance indicators for holistic hospital management with a modified DEMATEL approach. International journal of environmental research and public health. 2017;14(8):934.
-
15.
Herat AT, Noorossana R, Serkani ES. Using DEMATEL Analytic network process (ANP) hybrid algorithm approach for selecting improvement projects of Iranian excellence model in healthcare sector. African Journal of Business Management. 2012;6(2):627-45.
-
16.
Lu M, Lin S, Tzeng G. Improving RFID adoption in Taiwan's healthcare industry based on a DEMATEL technique with a hybrid MCDM model. Decision Support Systems. 2013;56:259-69.
-
17.
Liu H, You J, Lu C, Chen Y. Evaluating health-care waste treatment technologies using a hybrid multi-criteria decision making model. Renewable and Sustainable Energy Reviews. 2015;41:932-42.
-
18.
Ortiz Barrios MA, Nino C, Patricia J, La De Hoz AA, De Felice F, Petrillo A. An integrated approach of AHP-DEMATEL methods applied for the selection of allied hospitals in outpatient service. Journal of Medical Engineering and Informatics. 2016;8(2):87-107.
-
19.
Ortíz MA, Felizzola HA, Isaza SN. A contrast between DEMATEL-ANP and ANP methods for six sigma project selection: a case study in healthcare industry. BMC medical informatics and decision making. 2015;15(3). S3.
-
20.
Bahadori M, Ravangard R. Analysis of the systematic relationships among social determinants of health (SDH) and identification of their prioritization in Iran using DEMATEL technique. Iranian journal of public health. 2013;42(12):1457.
-
21.
Mamikhani J, Tofighi S, Sadeghifar J, Heydari M, Jenab VH. Prioritizing the compensation mechanisms for nurses working in emergency department of hospital using fuzzy DEMATEL technique: A survey from Iran. Global journal of health science. 2014;6(2):86.
-
22.
Nouri S, Riahi L, Hajinabi K, Jahangiri K. Resource Allocation Criteria for Health Care System Regulation: A Comprehensive Review of the Literature. Journal of Hospital. 2018;16(4):73-82.
-
23.
Greß S, Niebuhr D, Rothgang H, Wasem J. Criteria and procedures for determining benefit packages in health care: a comparative perspective. Health policy. 2005;73(1):78-91.
-
24.
Baghbanian A, Hughes I, Khavarpour FA. Resource allocation and economic evaluation in Australia’s healthcare system. Australian Health Review. 2011;35(3):278-83.
-
25.
Youngkong S, Tromp N, Chitama D. The EVIDEM framework and its usefulness for priority setting across a broad range of health interventions. Cost Effectiveness and Resource Allocation. 2011;9(1):8.
-
26.
Hauck K, Smith PC, Goddard M. The economics of priority setting for health care: a literature review. Washington, DC: The International Bank for Reconstruction and Development; 2004.
-
27.
Kapiriri L, Norheim OF. Criteria for priority-setting in health care in Uganda: exploration of stakeholders' values. Bulletin of the world Health Organization. 2004;82:172-9.
-
28.
Working Group on Priority Setting*. Priority setting for health research: lessons from developing countries. Health policy and planning. 2000;15(2):130-6.
-
29.
Asadi Lari M, Tavadi HR, Naghavi M, Gray D. The role of Health Related Quality Of Life (HRQOL) measurement in setting priorities in the Iranian health care system. proceeding of 5th international conference on priorities in healthcare. Nov. 2003- Nov.2005; Wellington, Newzealand. 2004.
-
30.
Dehnavieh R, Rashidian A, Maleki MR, Tabibi SA, Pour HI, Hekmat SN. Criteria for priority-setting in Iran basic health insurance package: Exploring the perceptions of health insurance experts. HealthMED. 2011;5(6):1542-8.
-
31.
Lim MK, Bae EY, Choi S, Lee EK, Lee T. Eliciting public preference for health-care resource allocation in South Korea. Value in Health. 2012;15(1):S91-4.
-
32.
Youngkong S, Teerawattananon Y, Tantivess S, Baltussen R. Multi-criteria decision analysis for setting priorities on HIV/AIDS interventions in Thailand. Health Research Policy and Systems. 2012;10(1):6.
-
33.
Youngkong S, Baltussen R, Tantivess S, Koolman X, Teerawattananon Y. Criteria for priority setting of HIV/AIDS interventions in Thailand: a discrete choice experiment. BMC health services research. 2010;10(1):197.
-
34.
Sutton M, Lock P. Regional differences in health care delivery: implications for a national resource allocation formula. Health Economics. 2000;9(6):547-59.
-
35.
Kogevinas M, Porta M. Socioeconomic differences in cancer survival: a review of the evidence. IARC scientific publications. 1997;138:177-206.
-
36.
Tromp N, Baltussen R. Mapping of multiple criteria for priority setting of health interventions: an aid for decision makers. BMC Health Services Research. 2012;12:454.