Abstract
Background:
Death of any of siblings is an overwhelming, severe, and prolonged challenge in children development process and is a major risk factor for psychiatric disorders in childhood and later. Interventions for bereaved families following a child’s death have been examined over the last several decades. However, no effective treatment for bereavement siblings prolonged grief disorder (PGD) and post-traumatic stress disorder (PTSD) has been found yet.Objectives:
The study aimed at determining the effect of Theraplay on the symptoms of prolonged grief (PG) and post-traumatic stress disorder (PTSD) in siblings of a deceased child with cancer.Methods:
In this preliminary study, a multiple baseline single-subject design with a follow-up period was used. The statistical population included siblings and mothers of children aged 6-10 years who had been under treatment at Mahak Child Cancer Hospital and died 1or 2 years ago. From this population, 4 mother-child pairs were selected as the study sample by convenience sampling. Each mother-child pair participated in 15 Theraplay sessions once a week (45-minute section). Assessments were performed using the inventory of prolonged grief for children (IPG-C) and the University of California at Los Angeles Posttraumatic Stress disorder reaction index for DSM-5 (UCLA PTSD-RI) at baseline, intervention sessions and follow-up stages. Visual analysis of graphic displays of level, reliable change index (RCI) and clinical significance were used to analyze the data. Data analysis and drawing graphs were performed in Microsoft Excel 2016.Results:
Results of visual and quantitative analysis of data showed that PG symptoms decreased in all 4 participants during the treatment and follow-up. Also, according to the results, Theraplay intervention significantly reduced PTSD in all participants.Conclusions:
Theraplay appears to be effective in reducing PG and PTSD in bereaved siblings. However, the reduction rate varied in different subjects. According to the findings, Theraplay helped subjects accept grief and loss and this method can be used to help the mental health of other bereaved children.Keywords
1. Background
Medical events such as severe injuries and life-threatening illnesses are diagnosed as potentially traumatic events. Among fatal diseases, childhood cancer is frequently considered as a traumatic event (1). When children are exposed to the situation in which their siblings are suffering from life-threatening illnesses, such as cancer, they are usually unprepared and find themselves in a critical situation. Such events affect the pattern of family life so that they experience disintegration of life every day and confront the unpleasant feeling of tension (2). Bowlby’s theory of attachment suggests that if a child in this situation perceives the threat to the life of their sibling who is deeply connected to, it results in anxiety and grief (3). Grief, as an emotion, is differently experienced by each individual and is partly dependent on the individual’s stage of life (2, 3). Reaction to death depends on the child’s maturity, personal experiences, and their understanding of death consequences (2, 4-6). Reactions to grief over the death of a sibling typically include severe sadness and depression for prolonged periods. Aggression is a common reaction and siblings may have behavioral problems (2, 7). Eilegard et al. in a survey on 174 bereaved siblings and 219 non- bereaved siblings’ experience showed that bereaved siblings had low self-esteem, minimum personal growth, and high levels of anxiety and depression (8). Reactions to death in children may be multifaceted and include cognitive distortions, strong emotions, physical issues, and psychological adjustment disorders (9). Grief for siblings is inadvertently ignored because the emphasis of social and family support is constantly on the parent’s loss experience (10). Also, the grief of these children may be not visible to other family members in the crisis because they are focusing on the death of the deceased child at this time (11-13). In addition, most children are well aware that their parents are disturbed and saddened by the death of their deceased child, so they do not express their own inner problems in order not to add to their parents’ grief. Furthermore, these children usually do not express their feelings freely, and this may mislead family members to think that the child is doing well. For this reason, and also because of the preoccupations, pain, and anguish of parents they often neglect the needs of bereaved siblings (13). Maercker reported that this could lead to the development of persistent complex bereavement disorder in surviving siblings, also known as prolonged grief disorder (PGD) (14). PGD is a proposed diagnostic category that is intended to classify bereaved individuals who experience notable dysfunction for atypically long periods of time following a significant loss (15). Core symptoms include a pervasive yearning for the deceased or persistent preoccupation with the deceased accompanied by intense emotional pain (16), a syndrome, which occurs in about 10% of bereaved adults. Similar to adults, 10% of children who are bereaved by sudden parental death have high and sustained prolonged grief reactions (PGR) nearly 3 years after death (17). A case study by Allen et al. (18) on a 16-year-old boy showed that he was experiencing symptoms of depression, anxiety, physical symptoms, and Post-traumatic stress disorder (PTSD) 8 years after the death of his older brother in an accident. In individual treatment sessions, he reported feeling guilt for his older brother’s death and anger with his mother for not speaking openly with him about his brother’s death (18). Many previous studies have shown that childhood cancer-related PTSD by focusing on the parents or the patient, and siblings have typically been excluded from these studies while they have witnessed pain, the severity of illness, or loss of weight and hair of their sick siblings. In addition, they may be away from the child with cancer for a long time, being afraid of their death possibility, do not understand the disease and treatment process, and greatly lose their parents’ support because of being involved in the patient’s treatment process. Furthermore, their daily routines being disrupted, and they have to stay with relatives or friends (1, 11, 19, 20). The results of a recent systematic review of the psychological adjustment of siblings of children with cancer showed that they are at risk for adjustment disorders and suggested that the distresses they experience can be conceptualized in a PTSD framework. They reported that 29% - 38% of siblings of children with cancer experience moderate to severe PTSD symptoms (1, 21). In a study in 2013, Kaplan et al. (1) showed that more than 60% of siblings of children with cancer reported moderate to severe PTSD, and 22% of them had all of the PTSD criteria. Considering the adjustment problems of siblings of children with cancer during illness, conditions that the family experiences before the death of the child, and major changes that occur after the death, these children often appear to face with problems that require early and appropriate psychological interventions to prevent more serious harm in subsequent years of development. However, much of the research on child bereavement has focused on losing a parent and limited research has been done on children who have experienced sibling loss (22-24). Numerous approaches have been proposed based on different approaches to the treatment of PGD. While these interventions usually emphasize the importance of talking about the lost person and feelings of grief, children are unable to express their emotions and feelings due to their low level of abstract thinking (25). Some of them avoid talking about their loss in order not to face the reality, pain and consequences of their loved one’s death (26). Theraplay is based on the Bowlby’s theory of attachment, where treatment is adjusted according to the early stages of the child’s development, where the child’s emotional development stops, and the attachment process is disrupted. Theraplay can explore the emotions and feelings of these children and provide them with a positive, warm and compassionate care, and a sense of value, as well as, fulfil their needs to adjust to their emotions and the child can achieve what they have lost before. Theraplay is not based on cognitive representation but rather on emotions and can be applicable to a wide range of emotional, social, and behavioral problems at different ages from childhood to adulthood (3, 27). In general, the main focus of this intervention is on connection, and its therapeutic model is based on the attachment theory including sensitive, responsive, and playful interaction between the caregiver and the child to facilitate child development, create positive internal working models of self and others, and its long-term impact on the child’s behavior and emotions. Activities are not the key to Theraplay efficiency! Rather, activities are merely tools that facilitate connection. The key is to pay attention to the child and to teach parents to pay attention to the child and to “wholeheartedly” help children become healthier and happier. This method is useful for all ages, from infancy to adolescence, but is used in the age range of 18 months to 12 years (28).The results of a study by Makela and Vierikko (29) have shown that Theraplay is effective for both boys and girls in reducing behavioral and emotional problems, especially aggressive behaviors, and this reduction has been persistent in follow-up studies. The goal of this treatment was to help the child to adjust their emotions and behaviors and challenge their negative internal working models (30).
2. Objectives
Less research has been conducted to determine the efficacy of psychological interventions on Prolonged grief disorder (PGD) and post-traumatic stress disorder (PTSD) in bereaved siblings; therefore, this study aimed at examining the effectiveness of Theraplay on PGD and PTSD in bereaved siblings.
3. Methods
The protocol of the study was approved by the Ethics Committee of University of Social Welfare and Rehabilitation Sciences (code: IR.USWR.REC.1398.050). This is preliminary quasi-experimental study with a multiple baseline single-subject design. The statistical population of this study comprised all 6-10-year-old siblings and mothers of children with cancer who were treated at the Mahak Child Cancer Hospital and died in 2017 - 2018. Samples were selected by convenience sampling. The siblings of deceased children with cancer were assessed for inclusion and exclusion criteria, and finally, 4 mother-child pairs were selected as the sample. The most important inclusion criteria were having an inventory of prolonged grief for children (IPG-C) score higher than the cut-off point of 40 (31) and the experience of losing a sibling due to cancer for at least one year, and the age range of 6 - 10 years for the child. The most important exclusion criteria were psychological disorders in the mother or, either the mother or the child be under treatment. Written informed consent was obtained from the parents of the subjects. To determine the baseline before the intervention sessions, all children were assessed by IPG-C and UCLA PTSD reaction index for DSM‐5 (UCLA PTSD-RI) three times with one-month intervals. They then participated in 15 individual 45-minute weekly sessions. Participants were re-evaluated by the questionnaires in the third, fifth, seventh, ninth, eleventh, thirteenth, and fifteenth sessions. The first and second follow-up results were obtained two weeks and one and a half months after the intervention.
3.1. Statistical Analysis
Visual analysis of graphic displays of level, reliable change index (RCI), and clinical significance were used to analyze the data. Statistical significance was evaluated by a reliable change index and clinical significance was determined by calculating the effect size.
In the reliable change index, the pre-test score was subtracted from the post-test score and the result was divided by the standard error of the difference between the two scores. If the absolute value of the result was equal to or greater than 1.96, it indicated that the obtained result was mostly due to experimental manipulation factors than measurement error (32).
The mean baseline reduction (MBLR) method was used to calculate the effect size. In this method, the mean of the treatment or follow-up phase observations is subtracted from the mean of baseline observations, then divided by the mean baseline observations, and the result is multiplied by 100 (33).
The formula for calculating effect size at treatment and follow-up stages was as follows:
Effect size = Mean 100 × Mean baseline observations - Mean treatment or follow-up stages observations)/(Baseline observations
3.2. Participants
Participant 1: (Girl, 9 years old), she and her sister were identical twins and her sister died due to nephroblastoma in 2017 at the age of 7.
Participant 2: (Boy, 10 years old) He was the first child of the family. His younger sister died in 2018 due to neuroblastoma at the age of 3.
Participant 3: (Girl, 7 years old) She was the first child of the family and her younger sister died in 2018 due to synovial sarcoma at the age of 1.
Participant 4: (Girl, 8 years old) She was the second child of the family, and her older sister died in 2017 due to glioma.
3.3. Theraplay for Bereaved Siblings: Treatment Plan
Theraplay focused on the mother and child. In addition to the therapy sessions where the mother and child were present, parenting sessions were planned for mothers. Under the supervision of the advisor professor, the researcher designed and implemented the intervention program based on the circle of security (34) and Theraplay-based parenting programs (35) and play therapy techniques. The protocol had 3 parts. The first part, which included play therapy sessions, was implemented by two trained play therapists. These sessions aimed at providing a safe and relaxed environment for children to express negative emotions, share memories and feelings, normalize painful emotions after the death of their siblings, increase their sense of control over events around them, and increase their self-esteem and self-confidence. The first interview session was allocated to gathering data from parents (the interview focused on attachment and parent-child relationship). In the second intervention session, the observation session was conducted using the Marschak interaction method in which, a parent and child perform a series of tasks together. Interactions were recorded and later analyzed by the therapist to prepare for a meeting with parents. In the third session, the therapist and the parents talked about their interactions and observations and then agreed on the therapeutic goals (feedback session with mother). The fourth to seventh sessions particularly dealt with the emotions of sadness, fear, anger, guilt, and loneliness caused by the sibling’s death. The eighth to tenth sessions dealt with wishes and changes after the sibling’s death; the eleventh and twelfth sessions dealt with the concept of security, safe base, and safe place; and the thirteenth and fourteenth dealt with the positive characteristics and abilities of the child. The fifteenth session included an end-of-course celebration and award-giving. The second part of the protocol included mothers’ group meetings. The purpose of these meetings was to provide a safe and secure environment for expressing negative emotions arising from loss of a child, to examine children’s problems and parent-child interactions, as well as to provide attachment-centered education tailored to bereaved children’s special needs. The third part of the protocol included mothers’ and children’s home games and homework, part of which was emotion-oriented and another part was relationship-oriented in order to achieve these goals.
Theraplay was administered weekly in 15 sessions of 45 minutes at the Mother and Child Clinic of Shahid Beheshti University.
3.4. Measurement Tools
3.4.1. Inventory of Prolonged Grief for Children (IPG-C)
Diagnosis of prolonged grief in children was based on the DSM definition and clinical symptoms with a score above 40 on the prolonged grief scale in children. Prolonged grief disorder is a syndrome that includes persistent, disruptive yearning, trouble accepting the death, detachment, excessive bitterness, difficulties to move on, and a sense that the loss has shattered one’s view of self, life, and future, present to the point of impairment beyond 6 months’ post-loss (30-36).
Spuij et al. (37) developed IPG-C based on the 30-item Inventory of Complicated Grief-Revised (ICG-R) by Prigerson and Jacobs (38). ICG-R was designed to assess prolonged grief symptoms in adults (formerly called complicated grief), and also they developed a version for children of 8 - 12 years old based on that. IPG-C consists of 30 items assessing PG symptoms in the past month and on a three-point Likert scale of “1 = almost never”, “2 = sometimes” and “3 = always”. PG symptoms score can be obtained from the sum of the item scores; therefore, each person can obtain a total score of 30 - 90 (36). In a study by Spuij et al. (37), on 169 bereaved children, the Cronbach’s alpha coefficient was 0.91 and temporal stability was obtained by the test-retest method. Also, to determine the concurrent validity of the test, its correlation was assessed with the scale of PTSD, depression, childhood traumatic grief, positive memory, and child behavioral checklist. Correlation coefficients were 0.78, 0.62., 0.38, and 0.11, respectively; and, contrary to expectation, IPG-C was not significantly correlated with the child behavioral checklist (37).
3.4.2. University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index for DSM-5
The current diagnostic criteria for PTSD (diagnostic and statistical manual of mental disorders, 4th Edition, text revision (DSM-IV-TR)) require that children have experienced, witnessed, or learned of a traumatic event, defined as one that is terrifying, shocking, and potentially threatening to life, safety, or physical integrity of self or others. Children must also meet at least one re-experiencing criteria, three avoidant/numbing criteria, and two hyperarousal criteria. Children must meet minimal duration criteria of at least 1 month, and they must show functional impairment in an important area (school, peers, family, and the like) (35).
The University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index for DSM-5 (UCLA PTSD-RI) is a self-report tool used to screen for trauma exposure and assess PTSD symptoms in children and adolescents (39).
The tool includes an extensive trauma history section, providing material to determine details of each type of traumatic event. The next section includes 27 items to assess PTSD symptoms as well as 4 additional items to assess structured disruption. Participants are evaluated for the frequency of symptoms experienced in the past months (from 0 = never to 4 = mostly). When answering questions, the participant should think about the traumatic event that is most distressing. Scores range from 0 to 80.
Items that evaluate the main symptoms of PTSD according to DSM criteria are classified into 4 scales (40): 5 questions to measure B scale (entering of intrusive thoughts), 2 questions to measure C scale (avoidance), 7 questions to measure D scale (negative and traumatic event-related changes in cognition (intellectual and mental activities, and mood), 6 questions to measure E scale (arousal and response style), and 4 additional items to measure disruption symptoms, that individual’s symptoms have the necessary criteria for PTSD. In response to stressors, one exhibits symptoms of disruption of either depersonalization or derealization (39).
Good translations and psychometric evaluations have been reported for this tool in which internal consistency was 0.88 - 0.91 (41). Kaplow et al. (42) reported internal consistency of 0.85 in a study to determine the psychometric properties of this questionnaire on a sample of 318 children and adolescents. In this study, the correlation between scores of PTSD-RI and trauma symptom checklist for children (TSCC) was determined in all samples and showed convergent validity. Cronbach’s alpha was 0.85 for the whole questionnaire, 0.82 for boys, and 0.84 for girls. Cronbach’s alpha was 0.75 and 0.90 in entrance of intrusive thoughts subscale; 0.42 and 0.85 in avoidance subscale; 0.77 and 0.88 in changes in cognition and mood subscale; and 0.70 and 0.82 in arousal subscale for boys and girls, respectively. There was a significant correlation between the total score of PTSD-RI and the B (r = 0.907), D (r = 0.676), C (r = 0.944), and E (r = 0.852) subscales. There was also a significant correlation between subscales (43).
4. Results
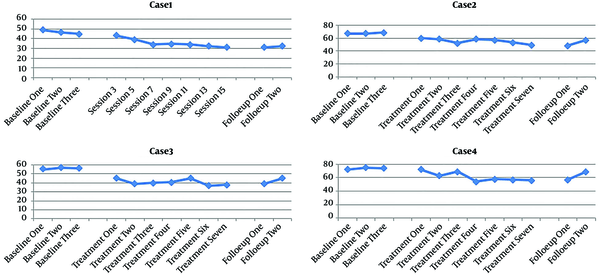
Participants’ scores for inventory of prolonged grief for children (IPG-C) and University of California at Los Angeles posttraumatic stress disorder reaction index for DSM-5 (UCLA PTSD-RI) are presented in Tables 1 and 2 and also Figures 1 and 2.
| Participant | Base line | Treatment | Follow-Up | Effect Size (Percentage of Recovery) | Significance | ||
|---|---|---|---|---|---|---|---|
| Baseline-Treatment | Baseline-Follow-Up | Absolute Value | Significance | ||||
| Participant 1 | 46.66 (2.08) | 35.42 (4.19) | 31.5 (0.707) | 24.08 | 32.49 | 4.37 | Significant |
| Participant 2 | 67.66 (1.154) | 55.28 (3.98) | 52.5 (6.36) | 18.29 | 22.4 | 5.124 | Significant |
| Participant 3 | 56 (1) | 40.71 (3.19) | 42 (4.24) | 27.3 | 25 | 7.867 | Significant |
| Participant 4 | 73.66 (1.52) | 61.28 (6.92) | 63 (8.48) | 16.8 | 14.47 | 2.969 | Significant |
| Total | 61 (10.97) | 48.17 (11.6) | 47.25 (13.27) | 21.03 | 22.54 | 3.25 | Significant |
| Participant | Base line | Treatment | Follow-Up | Effect Size (Percentage of Recovery) | Significance | ||
|---|---|---|---|---|---|---|---|
| Baseline-Treatment | Baseline-Follow-Up | Absolute Value | Significance | ||||
| Participant 1 | 23.33 (0.577) | 8.85 (5.81) | 3 (0) | 62.06 | 87.14 | 4.159 | Significant |
| Participant 2 | 66 (2) | 34 (8.3) | 33 (2.82) | 48.48 | 50 | 6.385 | Significant |
| Participant 3 | 58.33 (1.52) | 14.57 (8.44) | 8 (2.82) | 75.02 | 86.28 | 8.628 | Significant |
| Participant 4 | 76 (1.73) | 39.71 (17.48) | 28 (8.48) | 47.75 | 63.15 | 3.468 | Significant |
| Total | 55.91 (20.75) | 24.28 (16.7) | 18 (14.08) | 56.57 | 67.8 | 5.102 | Significant |
PG changes in participants 1, 2, 3, and 4 at baseline, intervention, and follow-up stages
PTSD total score changes in participants 1, 2, 3, and 4 at baseline, intervention and follow-up stages
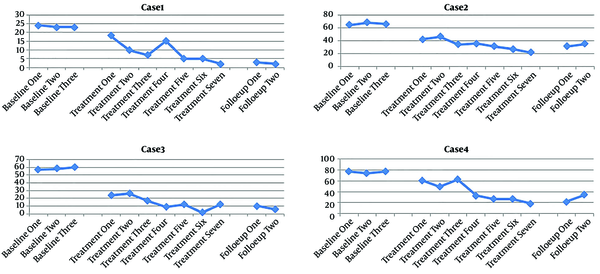
4.1. The Effect Size of Prolonged Grief Disorder (PGD) and Post-Traumatic Stress Disorder
Symptoms in the first participant was 24.08% and 32.49% in the intervention stage and 62.06% and 87.14% in the follow-up, respectively. Despite a steady decreasing trend during the sessions, the graphs of PG and post-traumatic stress disorder (PTSD) symptoms showed less decrease in the final treatment sessions compared to the other sessions.
PG and PTSD in the second participant reduced 18.29% and 48.48% in the intervention stage and 22.4% and 50% in the follow-up compared to the baseline, respectively. Therefore, it can be said that Theraplay was relatively effective in reducing the mentioned variables.
According to Figures 1 and 2, the overall trend of PG and PTSD changes decreased in the third participant and slightly increased in the follow-up stage. According to Tables 1 and 2, PG and PTSD effect sizes were 27.3% and 25% in the intervention stage and 75.02% and 28.86% in the follow-up, respectively.
In the fourth participant, the PG and PTSD overall trend was slightly decreasing with high variability. Regarding the effect size obtained (Table 1 and 2), PG and PTSD were 16.8% and 56.57% in the intervention and 14.47% and 67.8% in the follow-up stages compared to the baseline, respectively.
5. Discussion
The present study aimed at reducing prolonged grief disorder (PGD) and post-traumatic stress disorder (PTSD) symptoms in bereaved siblings. Findings showed that PG symptoms reduced in all 4 participants during treatment and follow-up, and considering the significant absolute value greater than 1.96 in all participants, Theraplay had a positive and significant effect on decreasing PG symptoms. Other findings of the present study showed that Theraplay significantly reduced PTSD total score in all participants.
It appears that this course of treatment has been effective in reducing the symptoms of prolonged grief (PG) and post-traumatic stress disorder (PTSD) in bereaved siblings by increasing awareness of emotions, reducing physical tension, training parents to provide care and contact and its effects on the agitation in children, facilitating the release of negative emotions in children and calming them after emotional release, reducing the feeling of loneliness regarding negative emotions (such as remorse, guilt and anger), accepting the loss, and regaining of strength.
The Reduction in subjects’ PG and PTSD scores are consistent with studies by Mahmudi Gharaii et al. (44), Wagner (45), Wethington et al. (46), Holmes et al. (47), and Hoagwood et al. (48). Wethington et al. (46) examined the effects of the cognitive-behavioral intervention on children affected by traumatic events. Their results showed that therapeutic intervention is effective in reducing the psychological damage caused by traumatic events in children and adolescents.
Numerous methods, based on different approaches, have been proposed for treating grief disorder. The use of psychotherapy intervention has been effective in several studies which aimed at reducing grief symptoms in children (49, 50). However, the severity of the distress experienced by the bereaved children, their cognitive capabilities, and developmental differences are ignored in the treatment of PG, an omission that can affect the effectiveness of this type of treatment in these children (31).
Siblings of children with cancer face several challenges including uncertainty concerning the progression of the disease, feeling of loneliness, poor family relationships, fear of death, and unresolved grief, all of which increase the risk of PTSD (51). Previous research has shown the effects of various therapeutic interventions on reducing the levels of distress, isolation, and anxiety, as well as, on improving social competence, social acceptance (52), and children’s adaptability (53) and on increasing the quality of life and personal development and reducing depression (54) in these children. Research on the psychological well-being of the siblings of the deceased children with cancer is still scanty, and due to the psychological problems of these children, they require specific specialized help (54).
Changes in parenting behavior, severe emotional distress, and internalization problems such as depression, anxiety, and PTSD in the mother are some of the most important factors affecting the adjustment problems of bereaved siblings. Among these factors, mothers’ depression is especially harmful to children (55) because these mothers will not be able to meet the needs of their children. Likewise, the decrease in mother’s patience, endurance, and energy following her grief reduces her parenting capacity and making it difficult for her to balance her personal grief and the needs of her children (56, 57). Considering these points, Theraplay may help surviving siblings in several ways and reduce the symptoms of PG and PTSD.
The Theraplay therapist provides safe organization (structure dimension), confident leadership, and sensitive adjustment of demands (challenge dimension), and models this approach for parents so that when children seek consolation from their parents, they can support their stressed children with the necessary peace and relief (28).
Theraplay first offers a progressive experience of safety and mutual social participation (58) and then co-regulation so that the parent forms a close attunement with the child and attend to the child’s emotion regulation and the repair of a situation that is not going well (affect synchrony and interactive repair) (59). It helps children become calmer, more compliant, and more extroverted (28) by creating more positive modes of relationship (internal working models) (3).
Theraplay is a “moment-to-moment” experience of the co-regulation of emotional and psychological states, through synchronous, face-to-face interactions using movement, proximity, and touch (all the features that Porges calls “polyvagal play” as a whole), in the form of a mutual game. It also gradually makes the mother more aware of the child’s responses and emotional state and offers a chain of playful activities (up-regulation) and relaxing ones (down-regulation), which provide opportunities for enjoyable and relaxing moments, help her understand and feel the child’s regulation state better and realize whether the child needs up-regulation or down-regulation, and find ways to help the child maintain the capacity to tolerate this level of arousal and avoid triggering stressful responses. In this process, the child becomes more capable of forming relationships instead of reacting defensively. This type of game chain can be described as a "neural exercise" to regulate the state (60).
The increase in parent-child emotional synchrony and response to the child’s emotional needs in Theraplay intervention occurs through 4 dimensions of structure, challenge, engagement, and nurture.
In general, whenever the primary caregiver can relieve the child’s stress, communicate emotionally with the child, and share happy moments with it, the child’s nervous system is able to deal with the loss, and various behavioral and emotional problems in children, which may be the result of their response to the death of a loved one, can be reduced through the development of secure attachment relationships by parents and their support for bereaved children (61).
Research showed that families with children with cancer undergo major changes after the death of the child (62). In some marriages, stronger ties are formed and some become weaker. Bereaved parents report lower marital satisfaction, less sexual intimacy, more frequent thoughts of separation, and higher divorce rates than non-bereaved parents (63). The above highlights the importance of parental adjustment to loss when the target group involves bereaved siblings. Alleviating the distress of bereaved mothers, emotional support of parents to improve the mental health of caregivers of surviving children, and the use of appropriate psychological interventions to resolve bereaved parents’ marital conflicts can influence the better adjustment of bereaved siblings and the long-term impact of treatment interventions (56).
The present study had also some limitations: random sampling was not practical and the convenience sampling method was used, and the sample size was small. It is recommended that the study be repeated with the larger sample size and random sampling. Furthermore, the implementation of the current intervention in 3 groups including 1 group comprising only mothers, 1 group comprising only children, and 1 group including mothers and children, and comparing the three groups, can clarify the effects of the intervention more accurately.
5.1. Conclusions
Theraplay is effective in reducing PG and PTSD symptoms in bereaved siblings. The therapeutic protocol used in this study provides a suitable model for dealing with bereaved children. Therefore, considering Theraplay as a kind of attachment-based play therapy in working with children, can help them accept their grief and loss of a loved one and this treatment can be used to improve children’s mental health.
Acknowledgements
References
-
1.
Kaplan LM, Kaal KJ, Bradley L, Alderfer MA. Cancer-related traumatic stress reactions in siblings of children with cancer. Fam Syst Health. 2013;31(2):205-17. [PubMed ID: 23795631]. [PubMed Central ID: PMC3780963]. https://doi.org/10.1037/a0032550.
-
2.
Jenholt Nolbris M, Enskar K, Hellstrom AL. Grief related to the experience of being the sibling of a child with cancer. Cancer Nurs. 2014;37(5):E1-7. [PubMed ID: 24145249]. https://doi.org/10.1097/NCC.0b013e3182a3e585.
-
3.
Bowlby J. A secure base: Parent-child attachment and healthy human development. Basic books; 2008.
-
4.
Giovanola J. Sibling involvement at the end of life. J Pediatr Oncol Nurs. 2005;22(4):222-6. [PubMed ID: 15994340]. https://doi.org/10.1177/1043454205276956.
-
5.
Mahon MM, Page ML. Childhood bereavement after the death of a sibling. Holist Nurs Pract. 1995;9(3):15-26. [PubMed ID: 7721965]. https://doi.org/10.1097/00004650-199504000-00006.
-
6.
Forward DR, Garlie N. Search for New Meaning: Adolescent Bereavement after the Sudden Death of a Sibling. Can J Sch Psychol. 2016;18(1-2):23-53. https://doi.org/10.1177/082957350301800103.
-
7.
Eilertsen MB, Lovgren M, Wallin AE, Kreicbergs U. Cancer-bereaved siblings' positive and negative memories and experiences of illness and death: A nationwide follow-up. Palliat Support Care. 2018;16(4):406-13. [PubMed ID: 28641585]. https://doi.org/10.1017/S1478951517000529.
-
8.
Hoffmann R, Kaiser J, Kersting A. Psychosocial outcomes in cancer-bereaved children and adolescents: A systematic review. Psychooncology. 2018;27(10):2327-38. [PubMed ID: 30120901]. https://doi.org/10.1002/pon.4863.
-
9.
Golden AM, Dalgleish T. Facets of pejorative self-processing in complicated grief. J Consult Clin Psychol. 2012;80(3):512-24. [PubMed ID: 22329823]. https://doi.org/10.1037/a0027338.
-
10.
Dickens N. Prevalence of Complicated Grief and Posttraumatic Stress Disorder in Children and Adolescents Following Sibling Death. Fam J. 2013;22(1):119-26. https://doi.org/10.1177/1066480713505066.
-
11.
Nolbris M, Enskar K, Hellstrom AL. Experience of siblings of children treated for cancer. Eur J Oncol Nurs. 2007;11(2):106-12. discussion 113-6. [PubMed ID: 17141569]. https://doi.org/10.1016/j.ejon.2006.10.002.
-
12.
Davidson D. Sibling loss - disenfranchised grief and forgotten mourners. Bereavement Care. 2018;37(3):124-30. https://doi.org/10.1080/02682621.2018.1535882.
-
13.
Howard Sharp KM, Russell C, Keim M, Barrera M, Gilmer MJ, Foster Akard T, et al. Grief and growth in bereaved siblings: Interactions between different sources of social support. Sch Psychol Q. 2018;33(3):363-71. [PubMed ID: 30234359]. [PubMed Central ID: PMC7450671]. https://doi.org/10.1037/spq0000253.
-
14.
Maercker A. When grief becomes a disorder. Eur Arch Psychiatry Clin Neurosci. 2007;257(8):435-6. [PubMed ID: 18000638]. https://doi.org/10.1007/s00406-007-0742-2.
-
15.
Lundorff M, Holmgren H, Zachariae R, Farver-Vestergaard I, O'Connor M. Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. J Affect Disord. 2017;212:138-49. [PubMed ID: 28167398]. https://doi.org/10.1016/j.jad.2017.01.030.
-
16.
World Health Organization. ICD-11 Beta Draft - Joint Linearization for Mortality and Morbidity Statistics. Geneva: WHO; 2016. Available from: http://apps.who.int/classifications/icd11/release/l-m/en#!/http%3A%2F%2Fid.who.int%2Ficd%2Fentity%2F1494673323.
-
17.
Melhem NM, Porta G, Walker Payne M, Brent DA. Identifying prolonged grief reactions in children: dimensional and diagnostic approaches. J Am Acad Child Adolesc Psychiatry. 2013;52(6):599-607 e7. [PubMed ID: 23702449]. [PubMed Central ID: PMC3664016]. https://doi.org/10.1016/j.jaac.2013.02.015.
-
18.
Allen B, Oseni A, Allen KE. The evidence-based treatment of chronic posttraumatic stress disorder and traumatic grief in an adolescent: A case study. Psychol Trauma. 2012;4(6):631-9. https://doi.org/10.1037/a0024930.
-
19.
Wilkins KL, Woodgate RL. A review of qualitative research on the childhood cancer experience from the perspective of siblings: a need to give them a voice. J Pediatr Oncol Nurs. 2005;22(6):305-19. [PubMed ID: 16216893]. https://doi.org/10.1177/1043454205278035.
-
20.
Prchal A, Landolt MA. How siblings of pediatric cancer patients experience the first time after diagnosis: a qualitative study. Cancer Nurs. 2012;35(2):133-40. [PubMed ID: 21760484]. https://doi.org/10.1097/NCC.0b013e31821e0c59.
-
21.
Alderfer MA, Long KA, Lown EA, Marsland AL, Ostrowski NL, Hock JM, et al. Psychosocial adjustment of siblings of children with cancer: a systematic review. Psychooncology. 2010;19(8):789-805. [PubMed ID: 19862680]. https://doi.org/10.1002/pon.1638.
-
22.
Worden JW. Children and grief: When a parent dies. New York: Guilford Press; 1996.
-
23.
Davies B. Shadows in the sun: The experiences of sibling bereavement in childhood. Philadelphia: Psychology Press; 1999.
-
24.
Daaleman TP, Elder GJ. Family medicine and the life course paradigm. J Am Board Fam Med. 2007;20(1):85-92. [PubMed ID: 17204740]. https://doi.org/10.3122/jabfm.2007.01.060012.
-
25.
Ray DC, Schottelkorb A, Tsai M. Play therapy with children exhibiting symptoms of attention deficit hyperactivity disorder. International Journal of Play Therapy. 2007;16(2):95-111. https://doi.org/10.1037/1555-6824.16.2.95.
-
26.
Haasl B, Marnocha J. Bereavement support group program for children: Leader manual. 2nd ed. Milton Park, Didcot: Taylor & Francis; 2000. 100 p.
-
27.
Munns E. Application of family and Group Theraplay. . 56. Maryland: Aronson; 2009.
-
28.
Lender DV. Theraplay The Practitioner's Guide. London: Jessica Kingley Publishers; 2020.
-
29.
Makela J, Vierikko I. From heart to heart: interactive therapy for children in care. Report on the Theraplay project in SOS Children’s Villages in Finland. 2001.
-
30.
Booth PB, Jernberg AM. Theraplay: Helping parents and children build better relationships through attachment-based play. Hoboken, New Jersey: John Wiley & Sons; 2009.
-
31.
Spuij M, van Londen-Huiberts A, Boelen PA. Cognitive-Behavioral Therapy for Prolonged Grief in Children: Feasibility and Multiple Baseline Study. Cogn Behav Pract. 2013;20(3):349-61. https://doi.org/10.1016/j.cbpra.2012.08.002.
-
32.
Khanipour H, Borjali A, Mohammadkhani P, Sohrabi F. Effectiveness of Mindfulness-Based Cognitive Therapy on Reducing Depression and Rumination Symptoms in Individuals with a Major Depression Record: A SingleCase Design. Clin Psychol Stud. 2013;4(13):23-42.
-
33.
Campbell JM. Statistical comparison of four effect sizes for single-subject designs. Behav Modif. 2004;28(2):234-46. [PubMed ID: 14997950]. https://doi.org/10.1177/0145445503259264.
-
34.
Marvin R, Cooper G, Hoffman K, Powell B. The Circle of Security project: attachment-based intervention with caregiver-pre-school child dyads. Attach Hum Dev. 2002;4(1):107-24. [PubMed ID: 12065033]. https://doi.org/10.1080/14616730252982491.
-
35.
Norris V, Rodwell H. Parenting with theraplay. London and Philadelphia: Jessica Kingsley Publisher; 2016. 320 p.
-
36.
Kaplan HI, Sadock BJ, Grebb JA. Kaplan and Sadock's synopsis of psychiatry: Behavioral sciences, clinical psychiatry. Wolters Kluwer; 1994.
-
37.
Spuij M, Prinzie P, Zijderlaan J, Stikkelbroek Y, Dillen L, de Roos C, et al. Psychometric properties of the Dutch Inventories of Prolonged Grief for Children and Adolescents. Clin Psychol Psychother. 2012;19(6):540-51. [PubMed ID: 21774035]. https://doi.org/10.1002/cpp.765.
-
38.
Prigerson HO, Jacobs SC. Traumatic grief as a distinct disorder: a rationale, consensus criteria, and a preliminary empirical test. In: Stroebe MS, Stroebe W, Hansson RO, Schut H, editors. Handbook of bereavement research; consequences, coping and care. Washington, DC: American Psychological Association; 2001. p. 613-37.
-
39.
Steinberg AM, Brymer MJ, Kim S, Briggs EC, Ippen CG, Ostrowski SA, et al. Psychometric properties of the UCLA PTSD reaction index: part I. J Trauma Stress. 2013;26(1):1-9. [PubMed ID: 23417873]. https://doi.org/10.1002/jts.21780.
-
40.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. https://doi.org/10.1176/appi.books.9780890425596.
-
41.
Doric A, Stevanovic D, Stupar D, Vostanis P, Atilola O, Moreira P, et al. UCLA PTSD reaction index for DSM-5 (PTSD-RI-5): a psychometric study of adolescents sampled from communities in eleven countries. Eur J Psychotraumatol. 2019;10(1):1605282. [PubMed ID: 31105904]. [PubMed Central ID: PMC6507911]. https://doi.org/10.1080/20008198.2019.1605282.
-
42.
Kaplow JB, Rolon-Arroyo B, Layne CM, Rooney E, Oosterhoff B, Hill R, et al. Validation of the UCLA PTSD Reaction Index for DSM-5: A Developmentally Informed Assessment Tool for Youth. J Am Acad Child Adolesc Psychiatry. 2020;59(1):186-94. [PubMed ID: 30953734]. https://doi.org/10.1016/j.jaac.2018.10.019.
-
43.
Takada S, Kameoka S, Okuyama M, Fujiwara T, Yagi J, Iwadare Y, et al. Feasibility and psychometric properties of the UCLA PTSD reaction index for DSM-5 in japanese youth: A multi-site study. Asian J Psychiatr. 2018;33:93-8. [PubMed ID: 29549818]. https://doi.org/10.1016/j.ajp.2018.03.011.
-
44.
Mahmudi Gharaii J, Bina M, Yasami M, Emami A, Naderi F. [Effect of group play therapy on symptoms associated with grief and damage caused by the incident Bam earthquake in children 3 to 6 years: A before and after study]. J Iran Pediatr. 2006;16(2):137-42. Persian.
-
45.
Wagner AW. Cognitive-behavioral therapy for posttraumatic stress disorder: applications to injured trauma survivors. Semin Clin Neuropsychiatry. 2003;8(3):175-87. [PubMed ID: 12874738]. https://doi.org/10.1016/s1084-3612(03)00018-2.
-
46.
Wethington HR, Hahn RA, Fuqua-Whitley DS, Sipe TA, Crosby AE, Johnson RL, et al. The effectiveness of interventions to reduce psychological harm from traumatic events among children and adolescents: a systematic review. Am J Prev Med. 2008;35(3):287-313. [PubMed ID: 18692745]. https://doi.org/10.1016/j.amepre.2008.06.024.
-
47.
Holmes CM, Goodwin D, Redhead ES, Goymour KL. The Benefits of Equine-Assisted Activities: An Exploratory Study. Child and Adolescent Social Work Journal. 2011;29(2):111-22. https://doi.org/10.1007/s10560-011-0251-z.
-
48.
Hoagwood KE, Acri M, Morrissey M, Peth-Pierce R. Animal-Assisted Therapies for Youth with or at risk for Mental Health Problems: A Systematic Review. Appl Dev Sci. 2017;21(1):1-13. [PubMed ID: 28798541]. [PubMed Central ID: PMC5546745]. https://doi.org/10.1080/10888691.2015.1134267.
-
49.
Jamshidi Sianaki M, Mazaheri MA. Grief intervention for helping bereaved children. Rooyesh-e-Ravanshenasi J. 2016;5(1):129-64.
-
50.
Zare S, Pourshahriari M, Rahimi C. [The effectiveness of play therapy on symptoms of grief in children (7-10) under supervision of Imam Khomeini Relief Foundation]. J Counsel Res. 2017;16(63):81-98. Persian.
-
51.
Long KA, Lehmann V, Gerhardt CA, Carpenter AL, Marsland AL, Alderfer MA. Psychosocial functioning and risk factors among siblings of children with cancer: An updated systematic review. Psychooncology. 2018;27(6):1467-79. [PubMed ID: 29441699]. https://doi.org/10.1002/pon.4669.
-
52.
Sidhu R, Passmore A, Baker D. The effectiveness of a peer support camp for siblings of children with cancer. Pediatr Blood Cancer. 2006;47(5):580-8. [PubMed ID: 16317733]. https://doi.org/10.1002/pbc.20653.
-
53.
Bokhorst CL, Sumter SR, Westenberg P. Social Support from Parents, Friends, Classmates, and Teachers in Children and Adolescents Aged 9 to 18 Years: Who Is Perceived as Most Supportive? Soc Develop. 2010;19(2):417-26. https://doi.org/10.1111/j.1467-9507.2009.00540.x.
-
54.
Greenwald N, Barrera M, Neville A, Hancock K. Feasibility of group intervention for bereaved siblings after pediatric cancer death. J Psychosoc Oncol. 2017;35(2):220-38. [PubMed ID: 27786614]. https://doi.org/10.1080/07347332.2016.1252823.
-
55.
Winnicott D. Winnicott D, editor. Distorção do ego em termos de falso e verdadeiro "self". O ambiente e os processos de maturação Porto Alegre: Artes Médicas; 2008. p. 128-39.
-
56.
Howard Sharp KM, Meadows EA, Keim MC, Winning AM, Barrera M, Gilmer MJ, et al. The Influence of Parent Distress and Parenting on Bereaved Siblings’ Externalizing Problems. J Child Fam Stud. 2019;29(4):1081-93. https://doi.org/10.1007/s10826-019-01640-0.
-
57.
Andrade MLD, Mishima-Gomes FKT, Barbieri V. Children’s Grief and Creativity: The Experience of Losing a Sibling. Psico-USF. 2018;23(1):25-36. https://doi.org/10.1590/1413-82712018230103.
-
58.
Porges SW, Dana DA. Clinical Applications of the Polyvagal Theory: The Emergence of Polyvagal-Informed Therapies (Norton Series on Interpersonal Neurobiology). New York: WW Norton & Company; 2018.
-
59.
Schore AN. Affect dysregulation and disorders of the self (Norton Series on Interpersonal Neurobiology). New York: WW Norton & Company; 2003.
-
60.
Lindaman S, Makela J. The polyvagal foundation of Theraplay treatment: Combining social engagement, play and nurture to create safety, regulation and resilience. Clin Appl Polyvagal Theory. 2018:227-47.
-
61.
Auman MJ. Bereavement support for children. J Sch Nurs. 2007;23(1):34-9. [PubMed ID: 17253893]. https://doi.org/10.1177/10598405070230010601.
-
62.
Martinson IM, McClowry SG, Davies B, Kuhlenkamp EJ. Changes over time: a study of family bereavement following childhood cancer. J Palliat Care. 1994;10(1):19-25. [PubMed ID: 8035252].
-
63.
Lang A, Gottlieb L. Marital intimacy in bereaved and nonbereaved couples: A comparative study. In: Papadatou D, Papadatos C, editors. Series in death education, aging, and health care Children and death. Washington, DC: Hemisphere Publishing Corp; 1991.