Abstract
Background:
Supraclavicular fossa masses have usually been malignant lesions. When fine needle aspiration biopsy results have not been satisfactory excisional biopsy of supraclavicular lymphadenopathy would be mandatory.Methods:
In this study we investigated 18 patients who had supraclavicular region metastasis from infraclavicular primary sites.Results:
Distant metastatic sites were mostly lung in origin. Other sites were breast, prostate, pancreas, cervix, urothelial, gastric carcinoma and pleural mesothelioma. All of our patients except the one with mesothelioma have died within one year after diagnosis of supraclavicular metastasis due to disseminated disease.Conclusions:
Supraclavicular neck masses should be evaluated carefully, since they were mostly malignant in origin. Lung has been the most common origin site. Early diagnosis would be critical because supraclavicular metastasis indicates poor prognosis with decreased survival. Excisional biopsy should be performed promptly when fine needle aspiration biopsy was not diagnostic.Keywords
Supraclavicular Metastasis Infraclavicular Excisional Biopsy
1. Introduction
Supraclavicular lymph node area lies above the manubrium, laterally to medial edge of common carotid artery, and medially to the clavicula and lateral rib margin (1). Metastasis to supraclavicular fossa could originate from head and neck or infraclavicular tumors. Primary metastatic sites from the head and neck region were usually hypopharynx, tonsil and nasopharynx. Infraclavicular region tumors, mostly lung, could also metastasize to supraclavicular region (2). Utility of fine needle aspration biopsy (FNAB), as a first line of investigation for lymph nodes, has assumed highly importance during the recent years (3). It would be simple, safe and cost effective. But when FNAB does not give enough diagnostic material, excisional biopsy should be planned. In this study we have retrospectively investigated excisional biopsy results of 18 patients with supraclavicular lymphadenopathy; the origin sites and histopathological types have discussed in the light of current literature.
2. Methods
18 patients (10 male, 8 female patients with ages between 42 to 78 and median age of 54) with supraclavicular lymphadenopathy for whom FNAB results were non-diagnostic or suspicious of malignancy have retrospectively analysed from years 2010 to 2014. Excisional biopsies from supraclavicular region have administered to all of them.
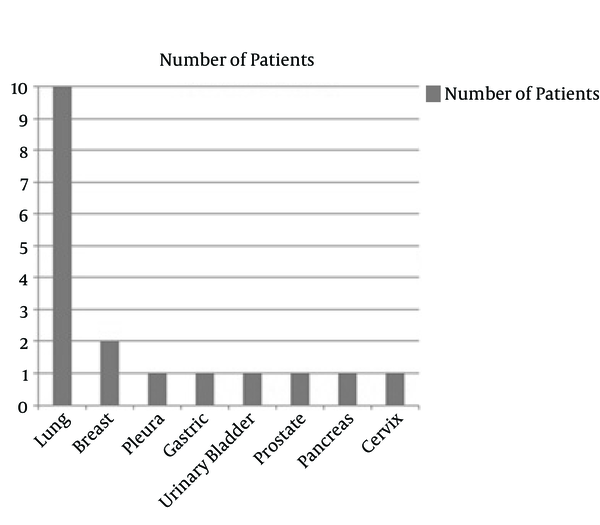
Distant metastatic sites: From 18 patients, 10 patients (55.5 %) of them were lung in origin, two patients (11%) were breast cancer, one patient (5.5%) was pleural mesothelioma, one patient (5.5%) was prostate carcinoma, one patient (5.5%) was pancreas, one patient (5.5 %) was cervix carcinoma, one patient (5.5%) was urinary bladder urothelial carcinoma metastasis, one patient (5,5%) was gastric carcinoma metastasis. Distant metastatic sites have summarized in Figure 1.
Number of 18 Patients According to Distant Metastatic Site
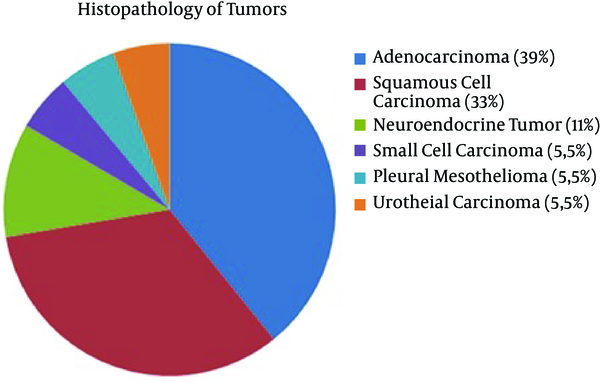
Histological types: From lung cancers; 5 cases (50%) were squamous cell carcinoma (SCC), two cases (20%) adenocarcinoma, two cases (20%) were neuroendocrine tumor (NET) and one case (10%) was small cell carcinoma. Gastric cancer, pancreatic cancer, prostatic cancer were adenocarcinoma, two breast cancers were invasive ductal carcinoma. Cervix cancer's case was SCC, one case was urothelial carcinoma from urinary bladder, one case was pleural mesothelioma. Totally there were 7 cases (39%) adenocarcinoma including invasize ductal carcinoma of breast, 6 cases (33%) SCC, two cases (11%) NET, one case (5.5%) pleural mesothelioma, one case (5.5 %) small cell carcinoma of lung, one case (5.5%) urothelial carcinoma. Histopathological types of tumors have shown in Figure 2.
Histopathological Types and Percentages of Tumors
Supraclavicular site of the metastasis were as follows: gastric, pancreatic, prostate, urothelial cancer of urinary bladder, cervix and 5 of cancers of the lung (totally 14% - 77.7%) have metastasized to left supraclavicular region whereas remaining 4 cancers of the lung (22.3%) metastasized to right supraclavicular fossa.
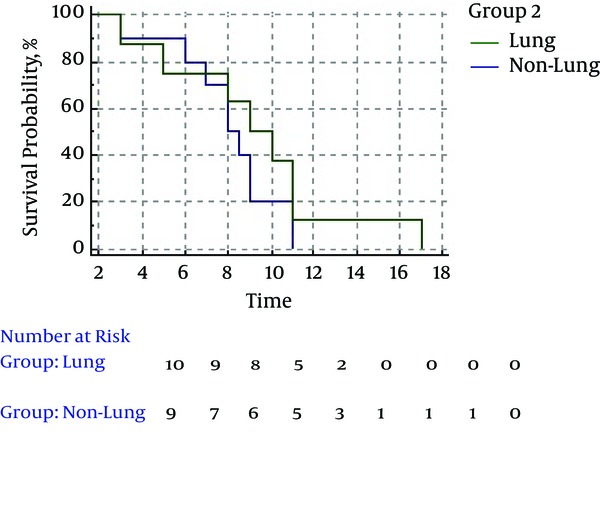
Survival rates: All of our patients except the one with mesothelioma have died within one year after diagnosis of supraclavicular metastasis due to disseminated disease. Survival rates of lung and non-lung cancers have shown in Figure 3 with Kaplan-Meiere curve.
Survival Analysis of Patients with Kaplan-Meiere Curve
Clinical features of the patients with survival analysis have summarized in Table 1.
Clinical Features of Patients with Survival Analysis Were Shown
| Patient No. | Age | Sex | Primary Site | Metastasis Site | Pathology | Survival, mo |
|---|---|---|---|---|---|---|
| 1 | 54 | Male | Lung | Left | SCC | 9 |
| 2 | 51 | Male | Lung | Left | SCC | 8.5 |
| 3 | 57 | Female | Lung | Left | SCC | 8 |
| 4 | 53 | Female | Lung | Right | SCC | 9 |
| 5 | 48 | Male | Lung | Right | SCC | 11 |
| 6 | 63 | Male | Lung | Right | Adenocarcinoma | 7 |
| 7 | 51 | Male | Lung | Left | Adenocarcinoma | 6 |
| 8 | 54 | Male | Lung | Right | NET | 8 |
| 9 | 57 | Male | Lung | Left | NET | 11 |
| 10 | 50 | Male | Lung | Left | Small cell carcinoma | 3 |
| 11 | 58 | Female | Breast | Left | Invasive ductal carcinoma | 5 |
| 12 | 57 | Female | Breast | Left | Invasive ductal carcinoma | 3 |
| 13 | 42 | Female | Pleura | Left | Mesothelioma | 17 |
| 14 | 52 | Male | Prostate | Left | Adenocarcinoma | 11 |
| 15 | 48 | Female | Pancreas | Left | Adenocarcinoma | 10 |
| 16 | 44 | Female | Cervix | Left | SCC | 9 |
| 17 | 78 | Male | Urinary Bladder | Left | Urothelial carcinoma | 11 |
| 18 | 55 | Female | Gastric | Left | Adenocarcinoma | 8 |
3. Discussion
The supraclavicular area is the final common pathway of the lymphatic system from infraclavicular sites as it joined to central venous system. Malignancies which have shown tendency to metastasize to supraclavicular region have mentioned as: lung, head and neck (mostly hypopharynx, tonsil and nasopharynx), breast, esophageal, gastric, pancreatic, gynecologic and prostate cancers (1).
Differential diagnosis of supraclavicular lymphadenopathy was broad and it has included benign lymphadenopathy, congenital cysts and tumors, specific infections, nonspecific inflammation, primary and metastatic malignancies (4). Supraclavicular lymphadenopathy would often be (58% - 83%) malignant. From these, majority (65% - 90%) were metastatic carcinomas from infraclavicular region. It has occured mainly on the left side such as in our study (3, 5).
Histopathological investigation of supraclavicular lymphadenopathy has shown that adenocarcinomas were mostly from pimaries of the breast, lung, prostate, stomach, pancreas and endometrium. Whereas SCC metastasis were primarily from cervix, mediastinum, esophagus, lung and head and neck region (6). Predominant histopathologic subtype of tumors metastasizing to supraclavicular region has differed according to authors. Giridharan et al. has published that majority of supraclavicular lymphadenopathy was SCC and next common histological diagnosis was lymphoma, followed by adenocarcinoma and undifferentiated carcinoma (7). But in the study of Carson et al. with 100 patients, the most common histological diagnosis was adenocarcinoma; second common histologic type was SCC. They have reported that adenocarcinoma has mostly metastasized to left region whereas SCC was to the right (6). All of these series were FNAB results. In our series of excisional biopsy results, most of them were adenocarcinoma (39%) followed by SCC (33%).
Site of the supraclavicular metastasis has differed according to distant metastatic site. Common iliac and paraaortic lymph nodes drain into thoracic duct. The thoracic duct communicates with systemic venous system at the junction of left subclavian and internal juguler vein. Left sided supraclavicular lymph node (Virchow's) has represented the final common pathway of the infradiaphragmatic sites (8). As a result; infradiaphragmatic tumors from abdominopelvic region has mostly metastasized to left supraclavicular fossa whereas supradiaphragmatic tumors from thoracic cavity could metastasize to both right and left region (9). Left supraclavicular lymph nodes might be involved in gastric carcinoma metastasis (Virchow's node) (3). In our study all of the infradiaphragmatic tumors, involving gastric, urinary bladder, cervix, pancreas, and prostate have metastasized to left supraclavicular region. Five of lung cancers have metastasized to left and four of them to the right.
Mass in the supraclavicular region should be evaluated seriously since most of them were malign in origin (3, 5). Metastatic lymphadenopathy in the supraclavicular region was mostly asymptomatic, and associated symptoms have mostly related to primary site such as odynophagia, dysphonia, otalgia and weight loss (7). When there were enlarged lymph nodes in the supraclavicular region, the digestive track, tracheobronchial tree, the breast, genitourinary tract and the thyroid gland should be taken into consideration as primary sites and these sites should be evaluated (7). FNAB has routinely used as a first line diagnostic test (10). When supraclavicular lymph nodes were palpable, it would be easy to achieve pathological material. Furthermore; non palpable lymph nodes in this region has not precluded metastasis from a distant site.
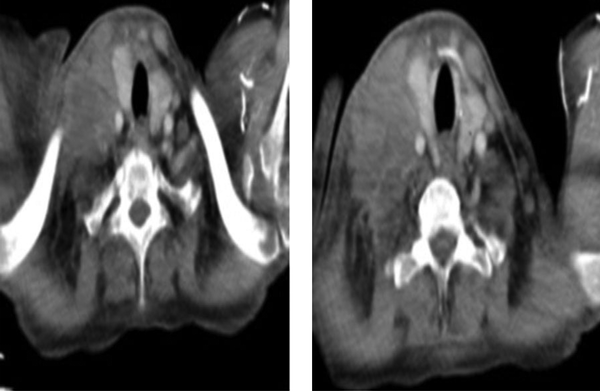
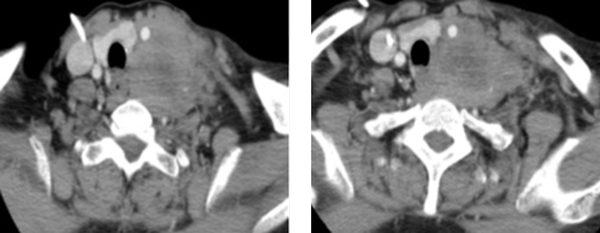
Most tumors of the lung have divided into two categories: non-small cell and small cell carcinomas. Non-small cell has also divided into SCC, large cell carcinoma, adenocarcinoma, alveolar cell carcinoma (11). Neuroendocrine tumors were a different group of tumors with neuroendocrine histopathological morphology and they could be either small cell or non-small cell (12). Supraclavicular nodal metastasis in lung cancer has considered as a contraindication to surgery of primary tumor, so diagnosis of metastatic supraclavicular lymphadenopathy would be too important (11). Spread from lung cancer to neck was rare; mostly adenocarcinoma and large cell carcinoma metastasize beyond thorax (11). But in our study most of the lung cancers were SCC and adenocarcinoma was the second most common histological type. Neck Computerized tomography (CT) of one of our patients with lung scc metastasizing to right supraclavicular region has shown in Figure 4. Patient with a history of known infraclavicular malignancy especially lung cancer should be evaluated with ultrasound for supraclavicular metastasis when there was no palpable lymph node in the neck (1, 10). In generally, 20% - 31% of patients with lung cancer had nonpalpable neck metastasis and when there was mediastinal lymphadenopathy on chest CT, nonpalpable lymph nodes in the supraclavicular region might not be seen in chest CT. In these cases ultrasonography (USG) was mandatory to see the metastatic lymph nodes in the supraclavicular region and to take pathological material by FNAB (1). In the study of Van Overhagen et al. sensitivities of palpation, CT and USG was 0.33, 0.83, and 1.00 respectively for detecting supraclavicular metastasis (13). In case of suspicion, only palpation was not sensitive for detecting supraclavicular lymphadenopathies, imaging studies should be performed. In most series lung cancer was the dominant primary site for supraclavicular lymph node metastasis (4-6, 10). The results of the our current study were similar with lung cancers comprising 55.5% of all cancers metastasizing to supraclavicular region. For small cell carcinoma of lung, mediastinal level 2 and 3 lymph node metastasis has seemed to be a predisposing factor for supraclavicular involvement, for these tumors prophylactic supraclavicular radiotherapy might have benefits for treatment (14, 15). In our study there were 2 cases of neuroendocrine tumor metastasis from lung. One of them was high grade (grade 3 - 4) and the other was grade 1. Small cell carcinoma of lung in our study was negative for neuroendocrine tumor marker chromogranin, so it was categorized as a different pathology.
Pleural Mesothelioma have known as malignant tumors of mesothelial cells with diffuse growth pattern originating from mostly pleura and less commonly peritoneum. Major predisposing factor was asbestos exposure. Lympathic invasion pattern was mostly to local lymph nodes intrathoracically. Supraclavicular lymph node metastasis was mostly in previously diagnosed mesothelioma patients, primary diagnosis with FNAB of supraclavicular lymph node was very rare (16). There has been no data revealing benefit of surgery for supraclavicular lymph node involvement. Our patient with mesothelioma has still followed with medical oncology department since 14 months after diagnosis of cervical lymph node metastasis.
Supraclavicular metastasis from breast cancer was rare (2.3% - 4.3%) (11). Presence of neck metastasis in breast cancer was an indicative of poor prognosis. Tumor grade and localization, systemic adjuvant treatment, patient age had no effect on supraclavicular metastasis in breast cancer whereas estogen and progesteron receptor negativity seems to be a predisposing factor for supraclavicular metastasis in breast cancer (17). There was a wide spread inconsistency among head and neck surgeons, breast oncologists, breast surgeons for the management of breast cancer with supraclavicular metastasis because of the limited reliable randomized data, so role of neck dissection was on debate for cervical metastatic breast cancer (11, 18). There were two breast cancer patients with supraclavicular metastasis in our study. They have died four and nine months after the diagnosis of supraclavicular metastasis despite appropriate chemotherapy (Figure 4).
Computerized Tomography Scans of the Patient with Lung Squamous Cell Carcinoma Metastasizing to Right Supraclavicular Fossa
Gastric cancer was the second most common cause of cancer-related death in the world (11). Left supraclavicular lymph nodes might be involved in gastric carcinoma metastasis (Virchow's node) (3, 19, 20). One of our cases was gastric adenocarcinoma with Virchow's node involvement (Figure 5). She had seven cure of chemotherapy including granisetron, cysplatin and fluorouracil with radiotherapy. She has died 10 months after diagnosis of supraclavicular lymph node metastasis due to widespread disease.
Computerized Tomography Scans of the Patient with Gastric Adenocarcinoma Metastasizing to Left Supraclavicular Fossa
Prostate adenocarcinoma was the most common malignancy in men. Most common metastatic sites of prostate adenocarcinoma have been: lymph nodes, bones, lungs, bladder and liver. Supraclavicular lymph node metastasis were rare (0.3%), and if occured it would be a poor prognostic indicator (21). Every male patient over 50 years with supraclavicular neck mass should be evaluated with serum prostate specific antigen (PSA) to rule out prostate cancer. FNAB of supraclavicular lymph node could be stained with PSA for further diagnosis (21). Supraclavicular lymph node involvement indicated systemic disease, there seems to be no role for curative neck dissection (11), although four patients in the series of Hemapour et al. (21) had survival of one year, three years, six years and three years after diagnosis respectively. One of our cases was prostate adenocarcinoma and he died after 11 months of diagnosis. Probable reason for short term survival rate was hepatic, pelvic, bone and lung metastasis at the time of diagnosis for our case.
Metastasis in carcinoma of cervix has initially involved pelvic lymph nodes, followed by paraaortic nodes and distant sites. Supraclavicular lymph node metastasis was extremely rare and reported inicidence is 0.1% - 1.5% (8). There was no evidence based benefit of neck dissection for supraclavicular metastasis form cervix cancer (11). One of our patients was cervix carcinoma who died after 10 months of diagnosis.
Lymphatic metastases have found in 20% - 25% of patients with urothelial carcinoma in the literature. Primary lympatic drainage is to external and internal iliac lymph nodes and obturatuar lymph nodes. Secondary drainage is to common iliac lymph nodes. There is no difference between transitional cell carcinoma and squamous cell carcinoma for frequency and location of metastasis. Urinary urothelial carcinoma could rarely occur in a lymphoma-like pattern with supraclavicular lymph node involvement (22). For supraclavicular metastasis of urothelial cancer, there were no reported cases for curative neck dissection in the literature.
Pancreatic cancer was the fourth common cancer related death in both men and women (23). Pancreatic cancer has mostly metastasized to liver and peritoneal cavities, supraclavicular lymph nodes have rarely affected with pancreatic cancer (24). Prevalance of supraclavicular metastasis from pancreas cancer was 1.9% - 2.4% (23, 24). There have isolated rare case reports regarding pancreatic cancer and supraclavicular lymph node metastasis (23, 24). In our study for one of the patients with supraclavicular lymph node metastasis, excisional biopsy result has revealed pancreatic or hepatobiliary system tumor. Abdominopelvic tomography of the patient has shown multiple enlarged conglomerated lymph nodes in the retroperitoneal region from pancreas to hepatic and perigastric region. Primary site has accepted to be pancreas and chemotherapy regimen including aprepitant, granisetron, cysplatin, gemcitabine has started by Medical Oncology department. She died four months after diagnosis of supraclavicular metastasis due to pulmonary nasocomial infection in the intensive care unit and disseminated cancer.
Although FNAB has been a first line investigation method for supraclavicular lymph node metastasis; when material was not diagnostic or suspicious of malignancy, open excisional biopsy was mandatory. In the study of Gupta et al. they have investigated diagnostic value of FNAB for supraclavicular lymph node enlargement in 218 cases, overall sensitivity of FNAB was 92.7% and specificity was 98.5%, but 46 cases have needed to be further investigated with open biopsy to confirm the diagnosis (3). We have thought that excisional biopsy of supraclavicular lymph node as early as possible was very important for suspicion of malignancy, since only one patient (5.5 %) in our series could survive after one years of diagnosis.
When supraclavicular metastases were from infraclavicular region there were rare tumors that neck dissection might have a benefit for survival and tumor spread. Upper and mid-thoracic esophagus cancers were one of these tumors. Nakagawa et al. has stated that for these tumors neck dissecton was beneficial for prognosis (25). For residual neck metastasis after chemotherapy or late neck relapse in testicular cancer patients, neck dissection might have a role for prognosis (11, 26). Kojima et al. has presented a case report of supraclavicular lymph node metastatic endometrium cancer succesfully treated with middle and lower juguler neck dissection and they have concluded that neck dissection as a salvage treatment might be beneficial in endometrium cancer patients (27). So; among cancers metastasizing to supraclavicular lymph nodes from infraclavicular region thoracic esophagus, testicular and endometrium cancer neck dissection might have a role in prognosis. In our study none of the patients had neck dissection for surgical control of supraclavicular metastasis.
As a conclussion, although most metastatic lymph nodes in the neck region arised from the head and neck primaries, supraclavicular lymph node metastasis should alert the surgeon to think of infraclavicular primary cancers, especially lung. Early excisional biopsy for suspicion of malignancy was crucial due to low survival rate and bad prognosis of infraclavicular tumors with supraclavicular metastasis.
References
-
1.
Fultz PJ, Harrow AR, Elvey SP, Feins RH, Strang JG, Wandtke JC, et al. Sonographically guided biopsy of supraclavicular lymph nodes: a simple alternative to lung biopsy and other more invasive procedures. AJR Am J Roentgenol. 2003;180(5):1403-9. [PubMed ID: 12704059]. https://doi.org/10.2214/ajr.180.5.1801403.
-
2.
Ismi O, Vayisoglu Y, Karabacak T, Unal M. Supraclavicular metastases from a sex cord stromal tumor of the ovary. Tumori. 2009;95(2):254-7. [PubMed ID: 19579877].
-
3.
Gupta RK, Naran S, Lallu S, Fauck R. The diagnostic value of fine needle aspiration cytology (FNAC) in the assessment of palpable supraclavicular lymph nodes: a study of 218 cases. Cytopathology. 2003;14(4):201-7. [PubMed ID: 12873313].
-
4.
Ellison E, LaPuerta P, Martin SE. Supraclavicular masses: results of a series of 309 cases biopsied by fine needle aspiration. Head Neck. 1999;21(3):239-46. [PubMed ID: 10208667].
-
5.
Gupta N, Rajwanshi A, Srinivasan R, Nijhawan R. Pathology of supraclavicular lymphadenopathy in Chandigarh, north India: an audit of 200 cases diagnosed by needle aspiration. Cytopathology. 2006;17(2):94-6. [PubMed ID: 16548994]. https://doi.org/10.1111/j.1365-2303.2006.00285.x.
-
6.
Carson HJ, Candel AG, Gattuso P, Castelli MJ. Fine-needle aspiration of supraclavicular lymph nodes. Diagn Cytopathol. 1996;14(3):216-20. [PubMed ID: 8732650]. https://doi.org/10.1002/(SICI)1097-0339(199604)14:3<216::AID-DC4>3.0.CO;2-F.
-
7.
Giridharan W, Hughes J, Fenton JE, Jones AS. Lymph node metastases in the lower neck. Clin Otolaryngol Allied Sci. 2003;28(3):221-6. [PubMed ID: 12755760].
-
8.
Tunio MA, Al Asiri M, Mohamed R, Al-Dandan S. Supraclavicular lymphadenopathy: initial manifestation of metastasis in carcinoma of cervix. Case Rep Obstet Gynecol. 2013;2013:409196. [PubMed ID: 23533864]. https://doi.org/10.1155/2013/409196.
-
9.
Nasuti JF, Mehrotra R, Gupta PK. Diagnostic value of fine-needle aspiration in supraclavicular lymphadenopathy: a study of 106 patients and review of literature. Diagn Cytopathol. 2001;25(6):351-5. [PubMed ID: 11747230].
-
10.
Mitra S, Ray S, Mitra PK. Analysis of FNAC of cervical lymph nodes: experience over a three-year period. J Indian Med Assoc. 2013;111(9):599-602. [PubMed ID: 24968522].
-
11.
Aldridge T, Kusanale A, Colbert S, Brennan PA. Supraclavicular metastases from distant primaries: what is the role of the head and neck surgeon? Br J Oral Maxillofac Surg. 2013;51(4):288-93. [PubMed ID: 22591766]. https://doi.org/10.1016/j.bjoms.2012.03.016.
-
12.
Moran CA, Suster S, Coppola D, Wick MR. Neuroendocrine carcinomas of the lung: a critical analysis. Am J Clin Pathol. 2009;131(2):206-21. [PubMed ID: 19141381]. https://doi.org/10.1309/AJCP9H1OTMUCSKQW.
-
13.
van Overhagen H, Brakel K, Heijenbrok MW, van Kasteren JH, van de Moosdijk CN, Roldaan AC, et al. Metastases in supraclavicular lymph nodes in lung cancer: assessment with palpation, US, and CT. Radiology. 2004;232(1):75-80. [PubMed ID: 15166326]. https://doi.org/10.1148/radiol.2321030663.
-
14.
Feng ZX, Zhao LJ, Guan Y, Sun Y, Meng MB, Ji K, et al. Identification of risk factors and characteristics of supraclavicular lymph node metastasis in patients with small cell lung cancer. Med Oncol. 2013;30(1):493. [PubMed ID: 23397085]. https://doi.org/10.1007/s12032-013-0493-z.
-
15.
Rossi G, Bisagni A, Cavazza A. High-grade neuroendocrine carcinoma. Curr Opin Pulm Med. 2014;20(4):332-9. [PubMed ID: 24811834]. https://doi.org/10.1097/MCP.0000000000000061.
-
16.
Tafazzoli A, Raza A, Martin SE. Primary diagnosis of malignant mesothelioma by fine-needle aspiration of a supraclavicular lymph node. Diagn Cytopathol. 2005;33(2):122-5. [PubMed ID: 16007670]. https://doi.org/10.1002/dc.20314.
-
17.
Siponen ET, Vaalavirta LA, Joensuu H, Leidenius MH. Axillary and supraclavicular recurrences are rare after axillary lymph node dissection in breast cancer. World J Surg. 2012;36(2):295-302. [PubMed ID: 22202994]. https://doi.org/10.1007/s00268-011-1399-6.
-
18.
Bisase B, Kerawala C. Survey of UK practice for management of breast cancer metastases to the neck. Ann R Coll Surg Engl. 2012;94(7):484-9. [PubMed ID: 23031766]. https://doi.org/10.1308/003588412X13171221591736.
-
19.
Yamashita K, Sakuramoto S, Kikuchi S, Katada N, Kobayashi N, Watanabe M. Validation of staging systems for gastric cancer. Gastric Cancer. 2008;11(2):111-8. [PubMed ID: 18595018]. https://doi.org/10.1007/s10120-008-0466-7.
-
20.
Iwazawa T, Kinuta M, Yano H, Matsui S, Tamagaki S, Yasue A, et al. An oral anticancer drug, TS-1, enabled a patient with advanced gastric cancer with Virchow's metastasis to receive curative resection. Gastric Cancer. 2002;5(2):96-101. [PubMed ID: 12111585]. https://doi.org/10.1007/s101200200016.
-
21.
Hematpour K, Bennett CJ, Rogers D, Head CS. Supraclavicular lymph node: incidence of unsuspected metastatic prostate cancer. Eur Arch Otorhinolaryngol. 2006;263(9):872-4. [PubMed ID: 16830117]. https://doi.org/10.1007/s00405-006-0066-2.
-
22.
Kancharla VP, Gulmi FA, Agheli A, Degen M, Gohari A, Jiang M, et al. Transitional Cell Carcinoma of the Bladder Manifestating as Malignant Lymphoma with Generalized Lymphadenopathy. Case Rep Oncol. 2010;3(2):125-30. [PubMed ID: 20740184]. https://doi.org/10.1159/000312424.
-
23.
Farma JM, Santillan AA, Melis M, Walters J, Belinc D, Chen DT, et al. PET/CT fusion scan enhances CT staging in patients with pancreatic neoplasms. Ann Surg Oncol. 2008;15(9):2465-71. [PubMed ID: 18551347]. https://doi.org/10.1245/s10434-008-9992-0.
-
24.
Soman AD, Collins JM, DePetris G, Decker GA, Silva A, Moss A, et al. Isolated supraclavicular lymph node metastasis in pancreatic adenocarcinoma: a report of three cases and review of the literature. JOP. 2010;11(6):604-9. [PubMed ID: 21068495].
-
25.
Nakagawa S, Nishimaki T, Kosugi S, Ohashi M, Kanda T, Hatakeyama K. Cervical lymphadenectomy is beneficial for patients with carcinoma of the upper and mid-thoracic esophagus. Dis Esophagus. 2003;16(1):4-8. [PubMed ID: 12581247].
-
26.
van Vledder MG, van der Hage JA, Kirkels WJ, Oosterhuis JW, Verhoef C, de Wilt JH. Cervical lymph node dissection for metastatic testicular cancer. Ann Surg Oncol. 2010;17(6):1682-7. [PubMed ID: 20333552]. https://doi.org/10.1245/s10434-010-1036-x.
-
27.
Kojima M, Yokoyama J, Ito S, Ohba S, Fujimaki M, Ikeda K. Impact of middle and lower jugular neck dissection on supraclavicular lymph node metastasis from endometrial carcinoma. World J Surg Oncol. 2012;10:143. [PubMed ID: 22788987]. https://doi.org/10.1186/1477-7819-10-143.