Abstract
Background:
Compared to other breast surgery methods, the accurate determination of pathologic margin in oncoplastic technique can affect its development and further employment of this technique. The current study aimed at evaluating positive pathologic margin after oncoplastic surgery and comparing it to that of the conventional breast-conserving surgery.Methods:
The current cross sectional and prospective study enrolled patients with breast cancer referring to the surgical clinic of Tehran Cancer Institute from 2010 to 2013. In this study, patients with breast cancer were evaluated based on the type of surgery (oncoplastic or conventional breast-conserving) they had undergone. Accordingly, the positive or negative result of the margin surgery was compared between the groups.Results:
In the current study, 317 patients with breast cancer underwent the surgery during the study period (154 patients in the oncoplastic and 163 patients in the conventional breast-conserving surgery groups). The highest frequency in the oncoplastic surgery belonged to Omega method (27.3%). The pathological evaluations after surgery showed ductal breast carcinoma in most of the cases in both groups (oncoplastic surgery = 94.2%; conventional breast-conserving surgery = 90.8%; P = 0.053). Positive margin in oncoplastic surgery and conventional breast-conserving surgery groups were 10.4% and 18.4%, respectively (P = 0.043). Among the 317 studied subjects, 14 relapse cases were observed; in 7 cases, mastectomy and in the rest, re-excision were conducted. Two out of 14 cases belonged to the positive margin group.Conclusions:
Using oncoplastic surgery as a method for breast surgery may play an important role in reducing the prevalence of positive margins compared to the conventional breast-conserving surgery.Keywords
Breast Cancer Oncoplastic Surgery Conventional Breast-Conserving Surgery
1. Background
In recent years, breast cancer surgery gradually tends from radical techniques toward complete tumor resection with the conservation of normal parenchymal tissue. In addition, to achieve the desired oncological results, this change may play an important role to get good cosmetic outcomes and improve quality of life in patients (1, 2). New innovations are created in the mentioned surgical techniques, emphasizing more on the cosmetic results after surgery through the reconstruction of partial mastectomy, called oncoplastic (3-5). Different studies showed desirable and appropriate therapeutic results for this method such as good cosmetic outcomes, better control over tumor margin, high satisfaction of patients, and high probability of breast conservation (6-11).
Candidates for breast oncoplastic surgery should be evaluated from different aspects by the surgeon before the operation. First, the location and size of removing tissue and the proper method of reconstruction for the defected location should be determined. At this stage, it can be determined if the patients is a suitable candidate for the surgery or not. The appropriate therapeutic program before the surgery may increase the capability of the surgeon regarding the type of cuts and size of removing tissue. The size of tumor is reduced in these patients after chemotherapy and they can be placed on the list of candidates for oncoplastic surgery (12-14).
The reconstruction of surgical site in oncoplastic technique lets the surgeon remove bigger tumors, using this method with breast-conserving; they were previously removed through mastectomy (15, 16). Breast reconstruction during the surgery depends on the ration of breast size to the tumor volume. In the smaller breasts, less glandular tissues are provided for the surgeon for reconstruction; hence, it is more probable to use local flaps for these patients. Mastectomy flap surgery has good cosmetic outcomes for patients with larger tumors (the resection ration ≥ 1/5) compared to the method conserving smaller breasts. In addition, the breasts’ symmetry should be considered; however, there is a disagreement regarding the restoration time to maintain symmetry in breasts (17-21). Considering the 0.1% to 5% probability of the metastasis to the opposite breast and also significant decrease in the level of breast cancer incidence in females over 50 years due to reduction in breast size may reduce the possibility of cancer incidence (22-26). Evaluations show the 15% to 30% complications after oncoplastic in the patients. These complications are skin flap necrosis, nipple or areole necrosis, seroma, hematoma, infection, open wound, and fat tissue necrosis. The most prevalent complication in T-reverse or Wise pattern techniques is delay in the restoration of wound edge due to decrease in vessel perfusion. Since the duration of the oncoplastic surgery is longer than those of the other methods, the candidates should be selected carefully (27, 28).
The hypothesis of oncoplastic surgery is that local restoration may affect the recurrence of illness and its diagnosis. Different studies conducted in this regard did not confirm the hypothesis and indicated that the rate of tumor recurrence was lower than that of the conventional breast-conserving surgery (29).
The current study aimed at evaluating the positive pathology margin after oncoplastic surgery and compared it with that of the conventional breast-conserving surgery.
2. Methods
The current cross sectional prospective study was conducted on patients with breast cancer referring to the surgical clinic of Tehran cancer institute from 2010 to 2013. This study was approved by ethics committee of Tehran Cancer Institute.
In the current study, patients with breast cancer were evaluated based on the type of surgery (oncoplastic and/or conventional breast-conserving) they underwent. The first result, which was compared between the groups, was the positive or negative surgical margin. The positive margin was defined in the current study as follows: 1) the tumor cell in the periphery or the closed tumor; 2) ductal carcinoma in-situ (DCIS) positive in periphery. The patients were followed-up for 2 years and the therapeutic results were evaluated. Inclusion criteria were as follow: stage I to III cancer of the breast incidence, unilateral cancer and healthy opposite breast, undergoing oncoplastic, or conventional breast-conserving surgeries.
The sample size was calculated by formula, using the results in Kaur et al.’s study (30).
The analyses were performed, using the SPSS software for Windows, version 21. The data were presented as proportion, mean, and conventional deviation. We used Chi-square and Fisher’s exact test for quantitative and qualitative variables. P values less than 0.05 were considered significant.
3. Results
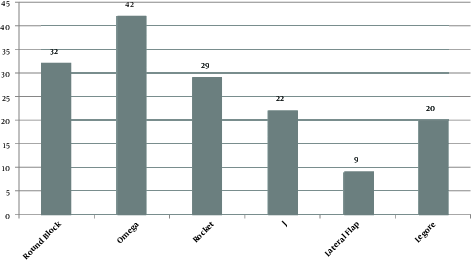
The current study classified 317 patients into 2 groups (154 subjects in the oncoplastic surgery and 163 subjects in the conventional breast-conserving surgery). The clinical features of the patients are presented in Table 1. The most prevalent type of the oncoplastic surgery was Omega (27.3%). The prevalence of different types of the oncoplastic surgery is illustrated in Figure 1. The pathological indices of the studied tumors were evaluated separately (Table 2).
The Clinical Features of the Patients
| Variables | Oncoplastic Group (N = 154) (100%) | Conventional Group (N = 163) (100%) | P Value |
|---|---|---|---|
| Tumor location | 0.002 | ||
| Central | 9 (5.8) | 6 (3.7) | |
| 6 | 11 (7.1) | 9 (5.5) | |
| 12 | 25 (16.2) | 13 (8.0) | |
| UOQ | 57 (37.0) | 88 (54.0) | |
| UIQ | 25 (16.2) | 37 (22.7) | |
| LOQ | 15 (9.7) | 5 (3.1) | |
| LIQ | 12 (7.8) | 5 (3.1) | |
| Biopsy | 0.001 | ||
| CNB | 111 (60.0) | 105 (64.4) | |
| Open Biopsy | 43 (47.2) | 43 (47.2) | |
| FNA | 0 (0.0) | 0 (0.0) | |
| Frozen in Surgery | 0 (0.0) | 0 (0.0) | |
| Axillary lymphadenopathy | 0.000 | ||
| SLNB | 84 (54.5) | 51 (31.3) | |
| ALNB | 42 (27.3) | 76 (46.6) | |
| SLNB + ALNB | 28 (18.2) | 36 (22.1) | |
| Frozen margin | 0.043 | ||
| Positive | 16 (10.4) | 30 (18.4) | |
| Negative | 138 (89.6) | 133 (81.6) |
The prevalence of different types of the oncoplastic surgery
The Pathological Indexes of the Studied Tumors
| Pathological Variables | Oncoplastic Group (N =154) (100%) | Conventional (Group N = 163) (100%) | P Value |
|---|---|---|---|
| Grade | 0.002 | ||
| I | 31 (20.1) | 41 (25.2) | |
| II | 97 (63.0) | 89 (54.6) | |
| III | 26 (16.9) | 33 (20.2) | |
| Tumor Size | 0.001 | ||
| T1 | 48 (31.2) | 57 (35.0) | |
| T2 | 98 (63.6) | 101 (62.0) | |
| T3 | 8 (5.2) | 5 (3.0) | |
| Node | 0.000 | ||
| Positive | 47 (30.5) | 56 (34.4) | |
| Negative | 107 (69.5) | 107 (65.6) | |
| Position | 0.043 | ||
| Lateral | 5 (31.3) | 6 (20.0) | |
| Medial | 1 (6.3) | 3 (10.0) | |
| Superior | 8 (50.0) | 10 (33.3) | |
| Inferior | 1 (6.3) | 5 (16.7) | |
| All Margin | 1 (6.3) | 6 (20.0) |
Therapeutic actions following the surgery were mastectomy, re-excision, and radiotherapy. Out of 16 subjects in the oncoplastic group with positive margin, 2 subjects did not refer. Hence, 14 subjects in the oncoplastic group and 30 subjects in the conventional breast-conserving surgery group were medically followed-up and the results are shown in Table 3.
The Outcome of Tumors with Positive Margin
| Variable | Oncoplastic Group (N = 14) (100%) | Conventional Group (N = 30) (100%) |
|---|---|---|
| Mastectomy | 8 (57.1) | 12 (40.0) |
| Re-excision | 5 (35.7) | 10 (33.3) |
| Radiotherapy | 1 (7.2) | 8 (26.7) |
There were 14 relapses among the 317 subjects; mastectomy was conducted for 7 cases and re-excision was performed for the rest 7 cases. Two relapse cases out of 14 belonged to positive margin group.
The pathological evaluations after surgery showed that most of the subjects in 2 groups were ductal (oncoplastic = 94.2%; conventional = 90.8%; P = 0.053). The distribution of pathology margins is shown in Table 4. Positive margin in oncoplastic group was 10.4% and in the conventional breast-conserving surgery group was 18.4% (P = 0.043).
The Distribution of Pathology Margins
| Pathological Index | Oncoplastic Group (N = 154) (100%) | Conventional Group (N = 163) (100%) |
|---|---|---|
| Tumor margin | ||
| Positive | 6 (3.9) | 13 (7.9) |
| Negative | 148 (96.1) | 150 (92.1) |
| Tumor closed | ||
| Positive | 6 (3.9) | 5 (3.1) |
| Negative | 148 (96.1) | 158 (96.9) |
| DCIS | ||
| Positive | 2 (1.2) | 8 (4.9) |
| Negative | 152 (98.8) | 155 (95.1) |
| DCIS closed | ||
| Positive | 2 (1.2) | 4 (2.5) |
| Negative | 152 (98.8) | 159 (97.5) |
4. Discussion
In the current study, 10.4% of the cases in the oncoplastic group needed surgery, while the rate for the conventional breast-conserving surgery was 18.4%, which could be because of more removal of breast tissue in breast-conserving and maintenance of the natural appearance of it in the oncoplastic surgeries. Similar results were also obtained in the similar studies. In a study conducted by Matrai et al. (31) the data of 60 cases with oncoplastic and 60 cases with conventional breast-conserving surgeries were compared. The size of tumor, the prevalence of quadrantectomy, metastasis to the local lymph nodes, and adjuvant chemotherapy were significantly higher in the oncoplastic group compared to the other group. Longer surgery time, higher weight of the cases, and less positive margin cases were reported in the oncoplastic group compared to the other group. There was a significant statistical difference between the groups regarding the prevalence of complications and adjuvant therapy onset time interval. The surgery cosmetic outcomes were significantly better in the oncoplastic group compared to the other group. Also, the level of pain in hand, shoulders, and chest were lower in the oncoplastic group. Totally, the researchers reported that the oncoplastic surgery was preferred to the conventional breast-conserving surgery regarding the extraction of breast tumors, even big ones. Oncoplastic surgery with less complication does not cause any delay in the adjuvant therapies; therefore, this method does not increase the risk of recurrence. Likewise, the good cosmetic outcomes of this method should also be considered (31).
Although breast oncoplastic surgeries let the surgeon perform a wider resection of tissue, the conducted tissue repair can make the evaluation of positive margin difficult. In the conducted studies, the rates of positive margin were reported as 2.7% to 22%, which were in association with the higher stages of cancer, positive lymph nodes, and positive lymphovascular invasion, using neoadjuvant chemotherapy, larger T, estrogen receptor, and lower age (32). In many oncoplastic margin methods, dermoglandular flaps are used, which transfer breast tissue from one side to another. If the surgery should be followed-up in the second stage, due to the malignancy on the peripheries, it turns into a challenge and makes the decision making for the cuts difficult (33). Frozen section is also used as a diagnosis method to evaluate tumor margin during the surgeries. Compared with those of paraffin method, the sensitivity and the accuracy of this method were 83% and 96%, respectively (34).
In another study, 440 cases of conventional breast-conserving surgery and 150 cases of oncoplastic surgery (in 146 females) were compared and the results showed that the rate of second surgery in the oncoplastic group was lower than that of the conventional one (2.7% compared to 13.4%). Local relapse in the conventional and the oncoplastic groups were 2.7% and 1.3%, respectively. Authors concluded that the probability of the second surgery in the oncoplastic group was lower than that of the conventional group (29).
In a study carried out by Down et al. (35) the conventional breast-conserving and the oncoplastic surgeries were employed for 121 and 37 subjects, respectively. In their study, the size of tumor in the groups with conventional and oncoplastic surgeries were 23.9 and 17.6 mm respectively, which showed statistically significant difference (P = 0.002). Also, the mean weight and size of tumor in the subjects of oncoplastic and conventional surgery groups were 231.1 and 58.1 g, respectively. The rate of margin in the oncoplastic and conventional surgery groups were 14.3 and 6.1 mm, respectively, which showed statistically significant difference (P = 0.00001). The suitable margin for the oncoplastic group can reduce the rate of need for the second surgery to 5.4%, compared to 28.9% rate of surgery need in the conventional group. The oncoplastic breast-conserving surgery is more successful compared to the conventional surgery regarding the treatment of large breast tumors by creating safe and suitable margin, which reduces the risk of subsequent surgeries in the positive margin subjects.
The present study proposed surgical therapy to the cases with positive margin. The radiotherapy was performed as an alternative treatment to the cases, who did not agree to the surgery (9 out of 44 cases with positive margin). No relapse was reported in the radiotherapy group during the two-year follow-up.
In the current study, 89.6% and 81.6% of the cases in the oncoplastic surgery and conventional breast-conserving surgery groups had negative margin (P= 0.043), which was compatible with the result of the other studies. Kaur et al. (30) evaluated 60 patients with breast cancer in 2 groups of oncoplastic surgery and conventional surgery. In the oncoplastic surgery and conventional surgery groups, 80.4% and 56.7% of the cases had negative margin, respectively (P = 0.05). The average distance between the surgical margin of the oncoplastic group and that of the conventional group were 8.5 and 6.5 mm, respectively, which had no statistically significant differences (P = 0.074). Researchers reported that the oncoplastic surgery was preferred to the conventional surgery since more size of tissue with higher margin can be removed by this method and it reduces the risk of positive margin (30).
The main objective of this study was to compare surgical margin after breast cancer surgery between oncoplastic technique and conventional breast-conserving surgery. Positive margin in oncoplastic group was less than that of in conventional breast-conserving surgery group (10.4 % vs 18.4 %), meaning that the oncoplastic method, as a breast cancer surgery, can play an important role in reducing positive margin cases, compared to the conventional breast-conserving surgery.
Acknowledgements
References
-
1.
Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med. 2002;347(8):567-75. [PubMed ID: 12192016]. https://doi.org/10.1056/NEJMoa020128.
-
2.
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233-41. [PubMed ID: 12393820]. https://doi.org/10.1056/NEJMoa022152.
-
3.
Clough KB, Ihrai T, Oden S, Kaufman G, Massey E, Nos C. Oncoplastic surgery for breast cancer based on tumour location and a quadrant-per-quadrant atlas. Br J Surg. 2012;99(10):1389-95. [PubMed ID: 22961518]. https://doi.org/10.1002/bjs.8877.
-
4.
Veiga DF, Veiga-Filho J, Ribeiro LM, Archangelo-Junior I, Mendes DA, Andrade VO, et al. Evaluations of aesthetic outcomes of oncoplastic surgery by surgeons of different gender and specialty: a prospective controlled study. Breast. 2011;20(5):407-12. [PubMed ID: 21530253]. https://doi.org/10.1016/j.breast.2011.04.001.
-
5.
Losken A, Pinell-White X, Hart AM, Freitas AM, Carlson GW, Styblo TM. The oncoplastic reduction approach to breast conservation therapy: benefits for margin control. Aesthet Surg J. 2014;34(8):1185-91. [PubMed ID: 25121787]. https://doi.org/10.1177/1090820X14545618.
-
6.
Barnea Y, Inbal A, Barsuk D, Menes T, Zaretski A, Leshem D, et al. Oncoplastic reduction using the vertical scar superior-medial pedicle pattern technique for immediate partial breast reconstruction. Can J Surg. 2014;57(4):E134-40. [PubMed ID: 25078939].
-
7.
Chan SW, Cheung PS, Lam SH. Cosmetic outcome and percentage of breast volume excision in oncoplastic breast conserving surgery. World J Surg. 2010;34(7):1447-52. [PubMed ID: 19936979]. https://doi.org/10.1007/s00268-009-0278-x.
-
8.
Losken A, Dugal CS, Styblo TM, Carlson GW. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg. 2014;72(2):145-9. [PubMed ID: 23503430]. https://doi.org/10.1097/SAP.0b013e3182605598.
-
9.
Chang EI, Peled AW, Foster RD, Lin C, Zeidler KR, Ewing CA, et al. Evaluating the feasibility of extended partial mastectomy and immediate reduction mammoplasty reconstruction as an alternative to mastectomy. Ann Surg. 2012;255(6):1151-7. [PubMed ID: 22470069]. https://doi.org/10.1097/SLA.0b013e31824f9769.
-
10.
Clough KB, Lewis JS, Couturaud B, Fitoussi A, Nos C, Falcou MC. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg. 2003;237(1):26-34. [PubMed ID: 12496527]. https://doi.org/10.1097/01.SLA.0000041230.77663.22.
-
11.
Peled AW, Sbitany H, Foster RD, Esserman LJ. Oncoplastic mammoplasty as a strategy for reducing reconstructive complications associated with postmastectomy radiation therapy. Breast J. 2014;20(3):302-7. [PubMed ID: 24750512]. https://doi.org/10.1111/tbj.12257.
-
12.
Fisher B, Bryant J, Wolmark N, Mamounas E, Brown A, Fisher ER, et al. Effect of preoperative chemotherapy on the outcome of women with operable breast cancer. J Clin Oncol. 1998;16(8):2672-85. [PubMed ID: 9704717]. https://doi.org/10.1200/JCO.1998.16.8.2672.
-
13.
Wolmark N, Wang J, Mamounas E, Bryant J, Fisher B. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;(30):96-102. [PubMed ID: 11773300].
-
14.
van der Hage JA, van de Velde CJ, Julien JP, Tubiana-Hulin M, Vandervelden C, Duchateau L. Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol. 2001;19(22):4224-37. [PubMed ID: 11709566]. https://doi.org/10.1200/JCO.2001.19.22.4224.
-
15.
Mauriac L, MacGrogan G, Avril A, Durand M, Floquet A, Debled M, et al. Neoadjuvant chemotherapy for operable breast carcinoma larger than 3 cm: a unicentre randomized trial with a 124-month median follow-up. Institut Bergonie Bordeaux Groupe Sein (IBBGS). Ann Oncol. 1999;10(1):47-52. [PubMed ID: 10076721].
-
16.
Mieog JS, van der Hage JA, van de Velde CJ. Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev. 2007;(2). CD005002. [PubMed ID: 17443564]. https://doi.org/10.1002/14651858.CD005002.pub2.
-
17.
Sbitany H, Wang F, Peled AW, Lentz R, Alvarado M, Ewing CA, et al. Immediate implant-based breast reconstruction following total skin-sparing mastectomy: defining the risk of preoperative and postoperative radiation therapy for surgical outcomes. Plast Reconstr Surg. 2014;134(3):396-404. [PubMed ID: 25158699]. https://doi.org/10.1097/PRS.0000000000000466.
-
18.
Clough KB, Baruch J. [Plastic surgery and conservative treatment of breast cancer. Indications and results]. Ann Chir Plast Esthet. 1992;37(6):682-92. [PubMed ID: 1340172].
-
19.
Berry MG, Cucchiara V, Davies DM. Breast augmentation: Part II--Adverse capsular contracture. J Plast Reconstr Aesthet Surg. 2010;63(12):2098-107. [PubMed ID: 20579948]. https://doi.org/10.1016/j.bjps.2010.04.011.
-
20.
Bong J, Parker J, Clapper R, Dooley W. Clinical series of oncoplastic mastopexy to optimize cosmesis of large-volume resections for breast conservation. Ann Surg Oncol. 2010;17(12):3247-51. [PubMed ID: 20549563]. https://doi.org/10.1245/s10434-010-1140-y.
-
21.
Chang E, Johnson N, Webber B, Booth J, Rahhal D, Gannett D, et al. Bilateral reduction mammoplasty in combination with lumpectomy for treatment of breast cancer in patients with macromastia. Am J Surg. 2004;187(5):647-50. discussion 650-1. [PubMed ID: 15135684]. https://doi.org/10.1016/j.amjsurg.2004.01.002.
-
22.
Kakagia D, Fragia K, Grekou A, Tsoutsos D. Reduction mammaplasty specimens and occult breast carcinomas. Eur J Surg Oncol. 2005;31(1):19-21. [PubMed ID: 15642421]. https://doi.org/10.1016/j.ejso.2004.07.026.
-
23.
Petit JY, Rietjens M, Contesso G, Bertin F, Gilles R. Contralateral mastoplasty for breast reconstruction: a good opportunity for glandular exploration and occult carcinomas diagnosis. Ann Surg Oncol. 1997;4(6):511-5. [PubMed ID: 9309343].
-
24.
Rietjens M, Urban CA, Rey PC, Mazzarol G, Maisonneuve P, Garusi C, et al. Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast. 2007;16(4):387-95. [PubMed ID: 17376687]. https://doi.org/10.1016/j.breast.2007.01.008.
-
25.
Boice JJ, Persson I, Brinton LA, Hober M, McLaughlin JK, Blot WJ, et al. Breast cancer following breast reduction surgery in Sweden. Plast Reconstr Surg. 2000;106(4):755-62. [PubMed ID: 11007385].
-
26.
Baildam AD. Oncoplastic surgery of the breast. Br J Surg. 2002;89(5):532-3. [PubMed ID: 11972541]. https://doi.org/10.1046/j.1365-2168.2002.02077.x.
-
27.
Hudson DA. A modified excision for combined reduction mammoplasty and breast conservation therapy in the treatment of breast cancer. Aesthetic Plast Surg. 2007;31(1):71-5. [PubMed ID: 17235466]. https://doi.org/10.1007/s00266-005-0063-7.
-
28.
Munhoz AM, Montag E, Arruda EG, Aldrighi C, Gemperli R, Aldrighi JM, et al. The role of the lateral thoracodorsal fasciocutaneous flap in immediate conservative breast surgery reconstruction. Plast Reconstr Surg. 2006;117(6):1699-710. [PubMed ID: 16651939]. https://doi.org/10.1097/01.prs.0000209943.13682.42.
-
29.
Chakravorty A, Shrestha AK, Sanmugalingam N, Rapisarda F, Roche N, Querci Della Rovere G, et al. How safe is oncoplastic breast conservation? Comparative analysis with standard breast conserving surgery. Eur J Surg Oncol. 2012;38(5):395-8. [PubMed ID: 22436560]. https://doi.org/10.1016/j.ejso.2012.02.186.
-
30.
Kaur N, Petit JY, Rietjens M, Maffini F, Luini A, Gatti G, et al. Comparative study of surgical margins in oncoplastic surgery and quadrantectomy in breast cancer. Ann Surg Oncol. 2005;12(7):539-45. [PubMed ID: 15889210]. https://doi.org/10.1245/ASO.2005.12.046.
-
31.
Matrai Z, Gulyas G, Kovacs E, Sandor Z, Polgar C, Bartal A, et al. [Oncoplastic versus conventional breast conserving surgery. A comparison of clinicopathological findings, cosmetic results and quality of life in 60 cases]. Magy Onkol. 2014;58(2):116-27. [PubMed ID: 25010760].
-
32.
Laucirica R. Intraoperative assessment of the breast: guidelines and potential pitfalls. Arch Pathol Lab Med. 2005;129(12):1565-74. [PubMed ID: 16329729]. https://doi.org/10.1043/1543-2165(2005)129[1565:IAOTBG]2.0.CO;2.
-
33.
Iwuchukwu OC, Harvey JR, Dordea M, Critchley AC, Drew PJ. The role of oncoplastic therapeutic mammoplasty in breast cancer surgery--a review. Surg Oncol. 2012;21(2):133-41. [PubMed ID: 21411311]. https://doi.org/10.1016/j.suronc.2011.01.002.
-
34.
Rusby JE, Paramanathan N, Laws SA, Rainsbury RM. Immediate latissimus dorsi miniflap volume replacement for partial mastectomy: use of intra-operative frozen sections to confirm negative margins. Am J Surg. 2008;196(4):512-8. [PubMed ID: 18809053]. https://doi.org/10.1016/j.amjsurg.2008.06.026.
-
35.
Down SK, Jha PK, Burger A, Hussien MI. Oncological advantages of oncoplastic breast-conserving surgery in treatment of early breast cancer. Breast J. 2013;19(1):56-63. [PubMed ID: 23301761]. https://doi.org/10.1111/tbj.12047.