Abstract
Background:
Upper respiratory tract infections (URTIs) are common in children. The cause of URTIs is usually viral, but parents' attitudes often contribute to inappropriate prescription of antibiotics, promoting antibiotic resistance.Objectives:
The objective of this study was to study the knowledge and behavior of mothers about antibiotic use in children under six years old with URTI.Methods:
Ninty-seven mothers with children under six years were evaluated in a semi-kap study about antibiotic use in children under six years old with URTI. Sampling was done with the convenient method. Data were collected using a researcher-made questionnaire.Results:
The mean age was 30.2 ± 7.2 years. Maternal knowledge was 8.2 ± 2.2 (scores ranged from zero to 12) and their performance was 4.1 ± 1.4 (scores ranged from zero to seven). Mothers had intermediate knowledge and performance. Knowledge was associated with mother and father's education, and mother and father's occupation (P < 0.05), but was not significantly correlated with the number of children. (P > 0.05) also, performance was associated with mother and father's education, and mother's occupation (P < 0.05) but was not significantly correlated with the father's education and number of children (P > 0.05).Conclusions:
The study findings suggest that mothers' knowledge and practice in the use of antibiotics is moderate, and lower parental education may lead to unnecessary antibiotic consumption and resistance.Keywords
1. Background
Acute respiratory infections in general is a title for upper and lower respiratory infections. Upper respiratory tract infections (ULRI) are common and typically mild and caused by viruses. Organisms that cause respiratory infections at a mild level are Reno, Corona viruses and respiratory syncytial viruses (1). Globally, more than half of child mortality is attributable to pneumonia, diarrhea, malaria and neonatal sepsis (2) and one out of every 50 preschool children dies of acute respiratory infection or associated factors (3). In fact, three main causes of death in acute respiratory infections are pneumonia, bronchiolitis and acute obstructive laryngitis (4). About two-third of deaths due to pneumonia occurred in ten African and Asian countries including India, Nigeria, Congo, Utopia, Pakistan, Afghanistan, Bangladesh, Angola and Niger (5). These deaths are more common in the rural population compared with the urban population (6). Acute respiratory infections could be caused by many different organisms. The clinical symptoms of viral and bacterial acute respiratory infections are the same and it is very difficult to differentiate between them. Lung or pleural aspiration of bacteria through invasive procedures (which increase the risk of serious problems) or blood cultures (which is positive in some cases) can be identified. The location and type of leakage seen on chest X-ray can be helpful to detect whether the infection is viral or bacterial (7). Because of the time-consuming nature of laboratory results and sometimes lack of necessary diagnostic equipment, specialists often make decisions to treat children with primary health facilities (without testing laboratory). Therefore, many detection methods are planned based on easy and rapid diagnostic techniques that are established as scientific approaches (8). Physicians sometimes encounter a dilemma on whether to treat acute ULRI infections with or without antibiotics (9). Unreasonable treatment with antibiotics may lead to the development of bacterial resistance and at the same time limited access to antibiotics may cause death. In developed countries, upper respiratory infections are treated with absolute limitation (10). In developing countries on the other side, problems in banning antibiotics to treat a bacterial infection due to lack of access to proper information and lack of acceptance by patients avoid the prescription of antibiotics for acute respiratory (11). Arbitrary, widely prescribed antibiotics have been reported worldwide. Generally, antibiotics are accessed from residual antibiotics from previous disease (12) or from the pharmacy without a prescription (13). Evidence from many countries shows that people are often expected that treatment with antibiotics is common for viral infections (14). Antibiotics resistance has become a major global problem. Lack of parents’ education, knowledge and no proper performance in the sense of antibiotics resistance has created disorders in the current health situation. Indiscretion in using antibiotics to treat upper respiratory tract infections by parents may be a factor leading to antibiotics resistance.
2. Objectives
The aim of this research was to study parent’s knowledges and practice about antibiotic use in less than six year-old children with URTI.
3. Methods
This cross-sectional study was carried out on 97 mothers from those who had referred to the pediatric clinic of Ali Asghar hospital located in the capital city of the province of Sistan and Baluchestan, zahedan, Iran. The present study was performed between October 2014 and 30th of November 2015. Inclusion criteria were having a child less than six years of age with URTI and exclusion criteria was lack of cooperation. This study was approved by the ethics committee of the research deputy of Zahedan University of Medical Sciences, in accordance to the declaration of Helsinki of the world medical association. The random sampling method was applied on those mothers who referred to the clinic for treating their children. A cross-sectional design was applied in order to obtain unbiased sample of referred mothers to the clinic regarding age, gender and socioeconomic status.
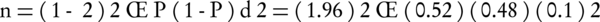
Sample size was determined using the following method and required parameters. The required parameters were: P = 0.52, d = 0.1 and α = 0.05.
Mothers were asked to participate in the study after receiving information about the goals of the study. If they were interested they were entered in the study but otherwise replaced with a new candidate. A researcher-made questionnaire was used as the tool for the measurement of the demographic data and knowledge and practices of parents related to antibiotics use in upper respiratory tract infections.
Demographic and socioeconomic questions were included maternal age, educational and job status of parents along with the number of children in the household. There were eight questions regarding parental knowledge and parents were asked to answer “YES I DO” or “NO” with a score of 1.5 and zero, respectively.
1- After receiving the drug from the drugstore, do you study the attached information sheet?
2- Do you believe that antibiotics have side effects?
3- Do you believe that to prevent infection, preventive antibiotic is effective?
4- Have you asked your child's doctor to prescribe antibiotics to recover your child from colds faster?
5- Have you asked your child's doctor to describe drug's effect sides?
6- Do you pay attention to the drug's expiration date?
7- Do you add extra substances to antibiotics due to its bad taste to allow easier intake for your child?
8- Do you pay attention to the expiry date of antibiotics?
Accordance to these questions knowledge scores ranged from 0 to 12 for each individual.
There were six questions regarding parental practice concerned with antibiotics and parents were asked to answer one of the interested items. Each question of this part was in a format of 5-point Likert scale: “1 = strongly agree”,” 0.8 = agree”,” 0.5 = uncertain”,” 0.2 = disagree” and” 0 = disagree strongly with the following questions”.
1- How much do you agree with the prescription of antibiotics for your child by the doctor?
2- Do you add extra substances to antibiotics due to its bad taste to allow easier intake for your child?
3- I follow the exact time for consumption of antibiotics for my child
4- I follow the exact dose for consumption of antibiotics for my child
5- I prefer intravenous antibiotics for my child
6- I prefer oral antibiotics for my child
In accordance to these questions, which show the maternal practice, the related scores ranged from 0 to 6 and the questions with inverse value were considered. To verify parent’s responses consistency and exclude random completion, two couples of similar questions (where each couple included the same statement expressed in a different way) and two pairs of contradictory questions (where each question included the reverse statement requiring the opposite answer) were entered in the questionnaire’s structure. The statistical analysis was conducted by using the SPSS software version 15. First we obtained Cronbach’s Alpha, resulting α = 0.78 and α = 0.72 for maternal knowledge and practice questions, respectively. For all questions except demographics, Cronbach’s Alpha was estimated as 0.75. After that Chi-square tests or Fisher’s exact test were used with a P < 0.05 for consideration of statistical significance.
4. Results
This study analyzed the knowledge and practice scores of 97 mothers of children less than six years old having upper respiratory tract infections and some affected factors. Mean maternal age was 30.2 ± 7.2 years and most of the mothers were aged from 28 to 34 years. The average number of children for every mother was 2.3 ± 1.3. Average scores of knowledge and practice were 8.22 ± 2.2 and 4.1 ± 1.4 with range of 0 to 12 and 0 to 6, respectively. Percentage distribution of 97 mothers related to knowledge was 24.7%, 41.2% and 34.00% for low, moderate and high states, respectively. These distributions related to the practice were 32%, 52.60% and 15.50% for low, moderate and high states, respectively. Maternal knowledge and maternal practice association with socioeconomic factors is shown in Table 1. The table showed that all factors except father’s job had a significant association with maternal knowledge and maternal practice. Table 2 shows that number of children per mother, did not have any correlation with both knowledge and maternal practice.
Impact of Socioeconomic Factors on Maternal Knowledge and Practice
| Variables | N | Knowledge Score Mean ± Standard Deviation | P Value |
|---|---|---|---|
| Mother education | 0.8 ± 0.0 | 0.001 | |
| Illiterate | 1 | ||
| Primary | 19 | 6.8 ± 1.7 | |
| Secondary | 14 | 7.5 ± 2.3 | |
| Diploma | 35 | 8.4 ± 2.3 | |
| Academic | 28 | 9.2 ± 1.6 | |
| Father education | 8.0 ± 0.0 | ||
| Illiterate | 1 | 0.001 | |
| Primary | 14 | 6.3 ± 1.9 | |
| Secondary | 17 | 7.8 ± 2.1 | |
| Diploma | 30 | 8.4 ± 1.9 | |
| Academic | 35 | 8.9 ± 2.0 | |
| Mother job | 0.036 | ||
| Housewife | 69 | 7.9 ± 2.2 | |
| Employee | 25 | 8.9 ± 1.8 | |
| Father job | 0.007 | ||
| Jobless | 8 | 7.4 ± 2.9 | |
| Free | 55 | 7.7 ± 2.2 | |
| Employee | 29 | 9.2 ± 1.7 | |
| Mother education | 0.003 | ||
| Illiterate | 1 | 3.0 ± 0.0 | |
| Primary | 19 | 3.3 ± 1.5 | |
| Secondary | 14 | 4.4 ± 1.1 | |
| Diploma | 35 | 3.8 ± 1.4 | |
| Academic | 28 | 4.7 ± 1.1 | |
| Father education | 0.004 | ||
| Illiterate | 1 | 3.0 ± 0.0 | |
| Primary | 14 | 3.2 ± 1.1 | |
| Secondary | 17 | 3.9 ± 1.8 | |
| Diploma | 30 | 4.2 ± 1.3 | |
| Academic | |||
| Mother job | 0.007 | ||
| Housewife | 35 | 4.5 ± 1.3 | |
| Employee | 69 | 3.8 ± 1.4 | |
| Jobless | 25 | 4.7 ± 1.2 | |
| Father job | 0.083 | ||
| Free | 8 | 3.4 ± 1.3 | |
| Employee | 55 | 3.9 ± 1.9 | |
| Housewife | 29 | 4.5 ± 1.0 |
Knowledge and Maternal Practice correlation with Number of Children
| Variables | Statistics | Number of Children |
|---|---|---|
| Knowledge | ||
| Correlation | -0.156 | |
| P. value | 0.134 | |
| Practice | ||
| Correlation | -0.169 | |
| P. value | 0.103 |
5. Discussion
The study showed that maternal knowledge and their practice increased with education. Similarly, mothers who were employed had higher knowledge and practice than housewives. Father’s education had a significant effect on both maternal knowledge and practice. However, the number of children did not show any difference in knowledge and practice. Panagakou showed that the majority of parents did not give antibiotics to their children without doctor’s advice and most of them did not believe that the disease is self-limited (15). Maternal knowledge in the study of Panagakou was higher than our study; this could be due to insufficient information and education of our mothers. However, many studies have reported low levels of parental knowledge and practice. Mohan showed that mothers with primary education had low level of understanding about the appropriate use of antibiotics for children with URTI. A significant number of mothers were advised to use antibiotics without prescription for their children (16). Yu et al. (17) suggested low level of awareness of parents on the use of antibiotics. They also reported a high prevalence of self-medication with antibiotics among parents in rural China. In a study by Chan et al. (18) in Malaysia, it was revealed that the majority of parents did not have proper functioning of knowledge about the use of antibiotics for acute respiratory infections in children and they had misconceptions about this. Trepka (19) reported that parental attitude about the effects of antibiotics and antibiotic resistances were changeable due to a direct dialogue between the physician and parents. Horwood used a video on the subject of good judgment to use antibiotics, in the waiting hall of some clinics and hospitals, which influenced parental attitude towards antibiotics. However, changing attitudes of parents did not change the rate of antibiotic prescriptions. The change in attitude of parents in this case is necessary, but is probably not enough to change the pattern of antibiotics prescription (20). An important reason for the poor parental performance or practice against disease may be is due to poor training (21) but Zsóka reported that behavioral and attitude changes among parents only through education is difficult (22). In a study by Huang, parents were divided to two case and control groups. Parents of the case group were under education of learning proper ways of using antibiotics and measured their knowledge after three years. The level of knowledge increased from 8% to 62% for controls when this increase was 7% from 54%. Regarding these two increases, Huang didn’t see significant differences. This subject showed that training course for mothers was not enough for changing their knowledge and performance (23). On the other hand, it has been known that the use of public health communication through the media effectively enhances and facilitates behavioral change (24). In this regard, the world health organization and United Nations children’s fund adopted a strategy with the aim of controlling the most common childhood diseases in developing countries by improving the skills of health workers in disease control, health system and the performance of families and the society (25). Thus, training programs with emphasis on performance in the health care system is essential. Given the widespread use of mass media in the best way and using these resources could improve the performance of mothers. The training programs should be directed for parents in order to improve their knowledge and performance at health centers.
5.1. Conclusion
The results of the present study showed that mean score of maternal knowledge and practice about antibiotics consumption are at a medium level. It was demonstrated that maternal training could reduce the unnecessary use of antibiotics and antibiotics resistance in our society.
Acknowledgements
References
-
1.
Spellberg B, Guidos R, Gilbert D, Bradley J, Boucher HW, Scheld WM, et al. The epidemic of antibiotic-resistant infections: a call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-64. [PubMed ID: 18171244]. https://doi.org/10.1086/524891.
-
2.
Earnshaw S, Monnet DL, Duncan B, O'Toole J, Ekdahl K, Goossens H. European Antibiotic Awareness Day Technical Advisory Committee. Euro Surveill. 2009;14:19280:1-8.
-
3.
Harnden A, Perera R, Brueggemann AB, Mayon-White R, Crook DW, Thomson A, et al. Respiratory infections for which general practitioners consider prescribing an antibiotic: a prospective study. Arch Dis Child. 2007;92(7):594-7. [PubMed ID: 17369279]. https://doi.org/10.1136/adc.2007.116665.
-
4.
Kouni S, Karakitsos P, Chranioti A, Theodoridou M, Chrousos G, Michos A. Evaluation of viral co-infections in hospitalized and non-hospitalized children with respiratory infections using microarrays. Clin Microbiol Infect. 2013;19(8):772-7. [PubMed ID: 23020634]. https://doi.org/10.1111/1469-0691.12015.
-
5.
Mangione-Smith R, McGlynn EA, Elliott MN, McDonald L, Franz CE, Kravitz RL. Parent expectations for antibiotics, physician-parent communication, and satisfaction. Arch Pediatr Adolesc Med. 2001;155(7):800-6. [PubMed ID: 11434847].
-
6.
Rudan I, El Arifeen S, Bhutta ZA, Black RE, Brooks A. Global Mortality from Childhood Pneumonia. PLoS Med. 2011;32(3):303-6.
-
7.
Hafner I. Respiratory emergencies. 4. 2013. 33 p.
-
8.
Bhutta M, Khurrum S, Rana A, Asad U. SCM Practices and the Health of SMEs in Pakistan. Supply Chain Manag Int J. 2007;12(6):412-22.
-
9.
Bronnum-Hansen H, Koch-Henriksen N, Stenager E. Trends in survival and cause of death in Danish patients with multiple sclerosis. Brain. 2004;127(Pt 4):844-50. [PubMed ID: 14960501]. https://doi.org/10.1093/brain/awh104.
-
10.
Petersen I, Hayward AC. Antibacterial prescribing in primary care. J Antimicrobial Chemotherapy. 2007;26:268-74.
-
11.
Bharathiraja R, Sridharan S, Chelliah LR, Suresh S, Senguttuvan M. Factors affecting antibiotic prescribing pattern in pediatric practice. Indian J Pediatr. 2005;72(10):877-9. [PubMed ID: 16272664].
-
12.
Grigoryan L, Haaijer-Ruskamp FM, Burgerhof JG, Mechtler R, Deschepper R, Tambic-Andrasevic A, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12(3):452-9. [PubMed ID: 16704784]. https://doi.org/10.3201/eid1205.050992.
-
13.
Khe ND, Toan NV, Xuan LT, Eriksson B, Hojer B, Diwan VK. Primary health concept revisited: where do people seek health care in a rural area of Vietnam? Health Policy. 2002;61(1):95-109. [PubMed ID: 12173499].
-
14.
Parimi N, Pinto Pereira LM, Prabhakar P. Caregivers' practices, knowledge and beliefs of antibiotics in paediatric upper respiratory tract infections in Trinidad and Tobago: a cross-sectional study. BMC Fam Pract. 2004;5:28. [PubMed ID: 15574193]. https://doi.org/10.1186/1471-2296-5-28.
-
15.
Panagakou SG, Spyridis N, Papaevangelou V, Theodoridou KM, Goutziana GP, Theodoridou MN, et al. Antibiotic use for upper respiratory tract infections in children: a cross-sectional survey of knowledge, attitudes, and practices (KAP) of parents in Greece. BMC Pediatr. 2011;11:60. [PubMed ID: 21729266]. https://doi.org/10.1186/1471-2431-11-60.
-
16.
Mohan S, Dharamraj K, Dindial R, Mathur D, Parmasad V, Ramdhanie J, et al. Physician behaviour for antimicrobial prescribing for paediatric upper respiratory tract infections: a survey in general practice in Trinidad, West Indies. Ann Clin Microbiol Antimicrob. 2004;3:11. [PubMed ID: 15196306]. https://doi.org/10.1186/1476-0711-3-11.
-
17.
Yu M, Zhao G, Stalsby Lundborg C, Zhu Y, Zhao Q, Xu B. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: a cross-sectional study. BMC Infect Dis. 2014;14:112. [PubMed ID: 24576064]. https://doi.org/10.1186/1471-2334-14-112.
-
18.
Chan GC, Tang SF. Parental knowledge, attitudes and antibiotic use for acute upper respiratory tract infection in children attending a primary healthcare clinic in Malaysia. Singapore Med J. 2006;47(4):266-70. [PubMed ID: 16572235].
-
19.
Trepka MJ, Belongia EA, Chyou PH, Davis JP, Schwartz B. The effect of a community intervention trial on parental knowledge and awareness of antibiotic resistance and appropriate antibiotic use in children. Pediatrics. 2001;107(1):6. [PubMed ID: 11134470].
-
20.
Horwood J, Cabral C, Hay AD, Ingram J. Primary care clinician antibiotic prescribing decisions in consultations for children with RTIs: a qualitative interview study. Br J Gen Pract. 2016;66(644):207-13. [PubMed ID: 26852795]. https://doi.org/10.3399/bjgp16X683821.
-
21.
Barkley RA. Defiant children: A clinician's manual for assessment and parent training. Guilford Press; 2013.
-
22.
Zsóka Á, Szerényi ZM, Széchy A, Kocsis T. Greening due to environmental education? Environmental knowledge, attitudes, consumer behavior and everyday pro-environmental activities of Hungarian high school and university students. J Cleaner Product. 2013;48:126-38.
-
23.
Huang SS, Rifas-Shiman SL, Kleinman K, Kotch J, Schiff N, Stille CJ, et al. Parental knowledge about antibiotic use: results of a cluster-randomized, multicommunity intervention. Pediatrics. 2007;119(4):698-706. [PubMed ID: 17403840]. https://doi.org/10.1542/peds.2006-2600.
-
24.
Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15(4):85. [PubMed ID: 23615206]. https://doi.org/10.2196/jmir.1933.
-
25.
Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin Psychol Sci. 2013.