Abstract
Background:
There is little data about the surgical outcomes of different procedures in children.Objectives:
We aimed to compare the difference in three-year surgical outcomes between laparoscopic sleeve gastrectomy laparoscopic sleeve gastrectomy (LSG) and one-anastomosis gastric bypass one-anastomosis gastric bypass (OAGB) in children undergoing these procedures.Methods:
A total of 96 children aged ≤ 19 years were listed for bariatric surgery to be included in this prospective study. Demographic characteristics, such as age and gender, and anthropometric indices, including height, weight, body mass index, waist circumference, and hip circumference, as well as postoperative complications, were recorded. The participants underwent LSG and OAGB by the same surgical team. The variables were compared between the groups at baseline and 1, 3, 6, 12, 24, and 36 months after surgery.Results:
At follow-up, the OAGB group had a higher waist circumference after 1 and 3 month(s) (P = 0.011 and 0.005, respectively) and higher hip circumference 3 months after surgery (P = 0.035). Time significantly affected the trend of changes in weight, body mass index, waist circumference, and hip circumference (P < 0.001). There were no cases of postoperative complications.Conclusions:
Our experience showed that LSG had better outcomes after three months, while LSG and OAGB had favorable outcomes on the weight and body mass index (BMI) of children with morbid obesity until three years after surgery.1. Background
Obesity is a worldwide growing health problem (1). with an increased risk of mortality and morbidity (2). Morbid obesity, defined as a body mass index (BMI) ≥ 40 kg/m2, is reported in approximately 1.5 - 4% of children and adolescents (3-5), with an increasing trend in recent decades (6). Morbid obesity, as a life-threatening condition, requires emergent treatment and surgical treatment. In this regard, bariatric surgery can be considered the best option for treating patients who fail to lose enough weight through non-surgical treatments (7, 8).
Bariatric or metabolic surgery is performed by various procedures worldwide, including Roux-en-Y gastric bypass, sleeve gastrectomy sleeve gastrectomy (SG), adjustable gastric banding adjustable gastric banding (AGB), and biliopancreatic diversion with duodenal switch biliopancreatic diversion with duodenal switch (BPD/DS) (9), favorably performed laparoscopically (10). Laparoscopic mini-gastric bypass laparoscopic mini gastric bypass (LMGB), also known as a one-anastomosis gastric bypass (OAGB), is a relatively new procedure, suggested as an effective and safe method of bariatric surgery (11) with favorable surgical outcomes (12). Studies have compared the efficacy of different surgical procedures on various postsurgical outcomes (13-15), while there are few investigations on the efficacy of diverse bariatric procedures in the pediatric population (16, 17). Most studies on morbid obese children have reported favorable outcomes for different bariatric techniques, including gastric banding, AGB, RYGB, SG, and laparoscopic RYGB (18-20). However, (laparoscopic) OAGB has scarcely been addressed.
Iran is a country with a high prevalence of obesity, estimated at 22% of adults and 6 - 12% of the pediatric population aged < 18 years (21, 22). However, different aspects of morbid obesity, such as the efficacy of distinct treatment protocols, are not well defined among the Iranian population, especially children. In our center, the approved center of excellence for metabolic and bariatric surgery by the international federation of surgery for obesity and metabolic disorders international Federation of surgery for obesity and metabolic disorders (IFSO), we actively manage obese and patients with morbid obesity, referring from variable parts of the country by different methods based on patients’ conditions. We accurately record patients' information in a web-based database at different follow-ups. There are insufficient data about morbid obesity treatment among the pediatric population in our country, as well as a lack of studies comparing the effect of laparoscopic SG (LSG) with OAGB in the pediatric population on patients' weight loss and health status.
2. Objectives
This study compared the three-year surgical outcomes between LSG and OAGB in children undergoing these procedures.
3. Methods
3.1. Participants
The study population of this retrospective study included children aged ≤ 19 years scheduled for bariatric surgeryduring 2011 - 2019 from National Obesity Surgery Database, Iran. The study protocol was approved by the Ethics Committee of the affiliated institution (code: IR.IUMS.REC 1396.30618). Before the enrollment of patients into the study, the researchers explained the research objectives to the children’s parents, informed them about the study steps and protocols, and asked them to read and sign the written informed consent for the participation of their child in the study. The inclusion criteria were the age of ≤ 19 years old, referring to the obesity clinic and private clinics during 2011 - 2019, and having an indication for bariatric surgery. Indications of bariatric surgery included BMI ≥ 40 kg/m2, BMI of 35 - 40 kg/m2 in addition to an obesity-related complication or failure of treatments other than surgery after two years, with an acceptable risk of surgery. All eligible patients were enrolled in the study by the census method.
The demographic characteristics of participants, including age and gender, were recorded, and their anthropometric indices, namely height, weight, waist circumference waist circumference (WC), and hip circumference (HC), were measured by the clinic’s physician and were recorded in the study checklist. The participants underwent two types of surgery, LSG, and OAGB, based on medical indications, such as nutritional habits and the presence of diseases, including gastroesophageal reflux. The surgical procedures were performed by one surgical team. OAGB was performed according to Rutledge’s method presented in 2001 (23). Accordingly, a long and narrow lesser curvature pouch was cut distal to the crow's foot and was continued vertically as a tube to the left side of the Hiss angle, and was finally anastomosed side to side with an omega-shaped jejunal loop at about 180 - 220 cm from the ligament of Treitz.
All participants were scheduled to be followed for three years and were visited after 1, 3, 6, 12, 24, and 36 months. Postsurgical complications, including postoperative bleeding, deep vein thrombosis deep vein thrombosis (DVT), intra-abdominal abscess, obstruction, pulmonary emboli (PE), wound dehiscence, and wound infection, were investigated during the follow-up visits and were recorded. Exclusion criteria are any patient who developed substance abuse or alcoholism, became pregnant during the follow-up period, had long durations of hospitalization (> 5 days) due to surgical complications or hypoalbuminemia, and required pre-surgery, as well as patients who had no weight loss after surgery due to reduced physical activity (such as traumatic patients).
3.2. Statistical Analysis
Statistical analysis was performed using the SPSS version 21 (IBM, USA). Analysis of data distribution was assessed by the Kolmogorov-Smirnov test. In order to show whether the variance of data in the two groups was equal or not, Levene’stest was used. Mean and standard deviation were calculated for normal variables, and median with IQR described the non-normal variables. For normally distributed data, the independent samples t-test and paired samples t-test were used; for non-normal variables, the Mann-Whitey U test and Wilcoxon (nonparametric independent and two related sample comparisons) were applied to compare variables. Repeated measures analysis of variance (ANOVA) with Greenhouse-Geisser correction of within-subjects effects was utilized to assess the differences between and within groups for weight loss and BMI at follow-up periods. P < 0.05 was accepted as statistical significance.
4. Results
A total of 96 patients were included in the analysis, of whom 58 (60.4%) were female and 38 (39.6%) were male. LSG was performed for 32 patients, and OAGB was performed for 64 people. The gender distribution of the groups was not different, with 22 females and ten males in the SG group and 36 females and 28 males in the OAGB group (P = 0.274). The mean age of the study, SG and OAGB groups was 17.21 ± 2.75, 16.65 ± 2.78, and 17.5 ± 2.71 years, respectively. The groups were not significantly different in terms of age (P = 0.159).There were no cases of postoperative complications in any of the groups.
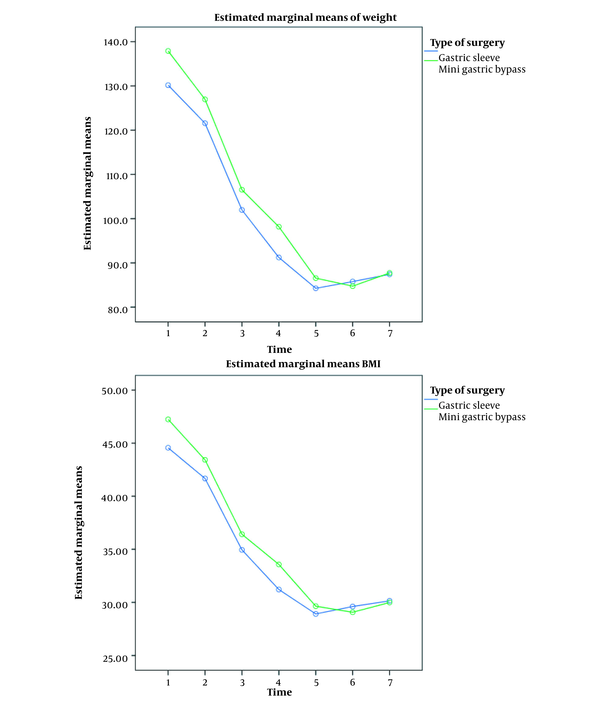
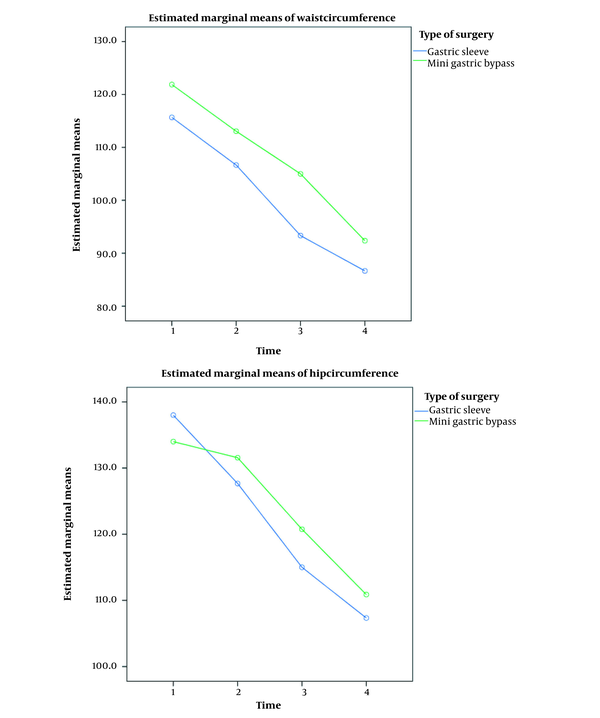
Mean and standard deviation (SD) of the weight, height, BMI, WC, and HC of patients in different time points in the two surgical groups are shown in Table 1. As indicated, the baseline weight in the OAGB group was higher than in the SG group (P = 0.04), while the other baseline characteristics, including BMI, were similar between the groups. According to the results of the independent samples t-test, the WC of the groups was different after 1 and 3 month(s) (P = 0.011 and 0.005, respectively), and HC was different 3 months after surgery (P = 0.035).The changes in weight and BMI are shown in Figure 1, and that of WC and HC are shown in Figure 2. Assessment of the effect of time using repeated measures ANOVA showed the significant effect of time on patients' weight and BMI considering seven time intervals (Figure 1) (P < 0.001). Due to a lot of loss to follow-up patients, studying the effect of time on WC and HC was only possible after 1, 3, and 6 months and the results of comparing the four intervals (these three in addition to baseline values) showed the significant effect of time on WC and HC (P < 0.001) as shown in Figure 2. In all cases, neither early complications (e.g., leakage, bleeding, abscess, dyspepsia, and wound infection) nor serious late complications in subsequent follow-ups (e.g., ulcer, stenosis, hypoalbuminemia, vomiting, anemia, reflux, internal hernia, gastroesophageal reflux disease (GERD), malnutrition, and cholelithiasis) were observed. Only the cases of anemia and vitamin D deficiency were found which were treated.
Mean Height, Weight, Body Mass Index, Waist Circumference, and Hip Circumference of Participants at Different Time Points in the Two Study Groups
| Variables and Time Points | Total | Sleeve Gastrectomy | One-Anastomosisgastric Bypass | P-Value a | |||
|---|---|---|---|---|---|---|---|
| N | Mean ± SD | N | Mean ± SD | N | Mean ± SD | ||
| Height (m) | 96 | 166.77 ± 8.46 | 32 | 165.08 ± 9.87 | 64 | 167.62 ± 7.6 | 0.167 |
| Weight (kg) | |||||||
| Before surgery | 96 | 136.14 ± 26.24 | 32 | 128.39 ± 24.8 | 64 | 140.02 ± 26.27 | 0.04 |
| 1 month after surgery | 92 | 126.18 ± 25.19 | 29 | 119.42 ± 24.06 | 63 | 129.29 ± 25.27 | 0.081 |
| 3 months after surgery | 81 | 106.52 ± 22.16 | 23 | 100.55 ± 15.59 | 58 | 108.89 ± 23.98 | 0.128 |
| 6 months after surgery | 76 | 96.17 ± 20.78 | 21 | 92.32 ± 14.63 | 55 | 97.64 ± 22.63 | 0.322 |
| 12 months after surgery | 62 | 85.00 ± 20.13 | 15 | 84.26 ± 12.59 | 47 | 85.24 ± 22.11 | 0.872 |
| 24 months after surgery | 44 | 80.48 ± 14.92 | 9 | 86.40 ± 17.18 | 35 | 78.96 ± 141.16 | 0.186 |
| 36 months after surgery | 27 | 87.64 ± 17.98 | 6 | 87.41 ± 25.2 | 21 | 87.71 ± 16.18 | 0.972 |
| Body mass index | |||||||
| Before surgery | 96 | 48.83 ± 8.01 | 32 | 46.98 ± 6.81 | 64 | 45.98 ± 7.14 | 0.111 |
| 1 month after surgery | 92 | 45.18 ± 7.57 | 29 | 43.65 ± 6.81 | 63 | 45.88 ± 7.85 | 0.19 |
| 3 months after surgery | 81 | 38.16 ± 7.23 | 23 | 37.03 ± 5.83 | 58 | 38.61 ± 7.72 | 0.377 |
| 6 months after surgery | 76 | 34.39 ± 6.85 | 21 | 33.97 ± 5.94 | 55 | 34.55 ± 7.21 | 0.743 |
| 12 months after surgery | 62 | 30.4 ± 6.71 | 15 | 31.01 ± 5.22 | 47 | 30.20 ± 7.16 | 0.687 |
| 24 months after surgery | 44 | 28.39 ± 4.84 | 9 | 30.44 ± 6.54 | 35 | 27.86 ± 4.26 | 0.157 |
| 36 months after surgery | 27 | 30.02 ± 8.94 | 6 | 30.14 ± 8.94 | 21 | 29.99 ± 4.53 | 0.953 |
| Waist circumference (cm) | |||||||
| Before surgery | 60 | 122.68 ± 28.36 | 19 | 113.84 ± 32.24 | 41 | 126.78 ± 25.78 | 0.101 |
| 1 month after surgery | 52 | 118.37 ± 13.71 | 19 | 112.07 ± 13.82 | 33 | 122.00 ± 12.45 | 0.011 |
| 3 months after surgery | 52 | 108.49 ± 14.39 | 16 | 100.28 ± 7.95 | 36 | 112.13 ± 15.17 | 0.005 |
| 6 months after surgery | 36 | 96.17 ± 20.78 | 11 | 94.27 ± 11.78 | 25 | 98.64 ± 8.36 | 0.879 |
| 12 months after surgery | 15 | 87.26 ± 9.39 | 4 | 87.00 ± 11.91 | 11 | 87.36 ± 8.99 | 0.95 |
| 24 months after surgery | 10 | 88.7 ± 14.82 | 3 | 85.33 ± 19.21 | 7 | 90.14 ± 14.08 | 0.665 |
| 36 months after surgery | 7 | 93 ± 10.59 | 0 | 0 | 7 | 93 ± 10.59 | – |
| Hip circumference (cm) | |||||||
| Before surgery | 60 | 135.55 ± 29.26 | 19 | 129.26 ± 32.81 | 41 | 138.46 ± 27.4 | 0.261 |
| 1 month after surgery | 52 | 156.22 ± 15.4 | 19 | 190.15 ± 25.35 | 33 | 136.68 ± 24.48 | 0.232 |
| 3 months after surgery | 52 | 125.42 ± 13.7 | 16 | 119.46 ± 8.53 | 36 | 128.06 ± 14.8 | 0.035 |
| 6 months after surgery | 36 | 113.45 ± 10.63 | 11 | 116.94 ± 10.43 | 25 | 112.32 ± 10.73 | 0.34 |
| 12 months after surgery | 15 | 104.86 ± 9.16 | 4 | 109.75 ± 9.21 | 11 | 103.09 ± 8.89 | 0.226 |
| 24 months after surgery | 10 | 107.1 ± 10.94 | 3 | 10.7.00 ± 16.0 | 7 | 107.14 ± 9.71 | 0.986 |
| 36 months after surgery | 7 | 112.57 ± 11.71 | 0 | 0 | 7 | 112.57 ± 11.71 | – |
Changes in the patients’ weight and body mass index in the two study groups
Changes in the patients’ waist and hip circumferences in the two study groups
5. Discussion
In this study, we investigated the effects of LSG and OAGB on 96 children aged ≤ 19 years with a mean age of 17.21 years and compared the weight, BMI, WC, and HC of the participants between the groups at baseline and 1, 3, 6, 12, 24, and 36 months after surgery. Our study showed that both groups had a significant decrease in all these variables at all the follow-up visits, with the significant effect of time on weight, BMI, WC, and HC. Comparison between the groups revealed similar weight and BMI at all intervals, while the OAGB group had a higher WC after 1 and 3 month(s) and higher HC after 3 months. These results confirmed the favorable impact of LSG and OAGB on the weight loss of the pediatric population.
Several studies have addressed morbid obesity management in children due to the increasing prevalence of morbid obesity in this population and its negative influence on their growth and future adulthood diseases (4). In the first report of LSG in children, this technique was suggested as a safe and effective stand-alone surgical option for managing morbid obese children (24).Other researchers confirmed favorable short-term results for LSG on the weight loss of children and adolescents (< 19 years) (25). In addition, the comparison of results with a matched group undergoing non-surgical weight management suggested significant weight loss, improved growth, and the resolution of comorbidities without a significant rise in the mortality or morbidity rate by LSG in children aged < 14 years (26). These results support the findings of the present study, suggesting that the LSG group lost weight for three years after surgery. In our study, the mean weight and BMI of patients at baseline were128.4 kg and 46.98 kg/m2, respectively, while in the study by Boza et al., the presurgical values (98 kg and 38.5 kg/m2, respectively) (25) were higher than that of our study. Despite the higher baseline weight and BMI, we observed a significant decline in patients' weight and BMI with a decreasing trend in the mean weight until 12 months after surgery and BMI until 3 years postop in the group undergoing LSG. These results confirm the efficacy of LSG on the weight loss of children with morbid obesity aged ≤ 19 years without any postoperative complications among 32 cases.
The other group in the current research underwent OAGB. Patients in this group had a mean weight of 140 kg and a mean BMI of 45.98 kg/m2 before surgery, both of which showed a decreasing trend until 24 months after surgery but increased a bit after that. One-anastomosis gastric bypass is a relatively new technique, introduced in 2001 for adults with morbid obesity (23), and most studies have investigated its efficacy and safety only in the adult population (11, 27). In a 10-year follow-up study by Lee et al., comparing the results of laparoscopic RYGB with OAGB showed lower mean BMI in the OAGB group with a shorter duration of surgery, which suggested OAGB as a safe and efficient alternative (28). The results of the latter study are in line with that of the present study, indicating significant weight loss in the group undergoing OAGB, while we have included patients aged ≤ 19 years. Following the successful weight lossin one case aged 12 years undergoing OAGB after 5 years (29), Carbajo et al. reported the results of a 5-year follow-up of children aged 13 - 19 years (mean: 17.8 years) undergoing OAGB at the European IFSO excellence center and showed that the mean BMI of participants declined from the pre-operative value of 42.2 kg/m2 to 25.9 kg/m2 after 5 years (30). These findings are consistent with our results, suggesting OAGB as a valid alternative in children and adolescents with favorable long-term results. Among 64 patients undergoing OAGB, there were no cases of postoperative complications. These results confirm the safety and efficacy of OAGB in children. In other studies on 1000 (31) and 1200 cases (32) undergoing OAGB, the researchers reported short-term complications in about 1 - 2.7% of patients. However, these studies have addressed surgical outcomes in the adult population. One-anastomosis gastric bypass complications must be further investigated in children and adolescents in large populations.
In our study, the comparison of the outcomes of LSG and OAGB groups showed that both groups had similar weight and BMI after surgery, while the OAGB group had a higher WC after 1 and 3 month(s) and higher HC after 3 months, which could be due to the higher mean baseline weight of children in the OAGB group. As WC and HC of the groups were not different at other intervals, there was no difference between the mean weight or BMI of the groups, and both groups had a decreasing trend in weight, BMI, WC, and HC, with a significant effect of time. We can conclude that both LSG and OAGB resulted in substantial weight loss in the studied population with similar impacts. We could not find any other studies comparing these two methods in children. Other investigations have reported other bariatric techniques, including gastric banding and AGB (18), RYGB and SG (19), and laparoscopic RYGB, SG, and AGB (20) and have revealed favorable outcomes. Therefore, further studies are required to compare the effect of OAGB with other bariatric procedures to indicate the best treatment choice for children with morbid obesity.
5.1. Limitations
We compared the efficacy of OAGB with LSG for the first time in children and adolescents, extracting valid data from the IFSO excellence center. The present study had some limitations. First, the number of patients meeting the inclusion criteria was low, which limited the sample size of our study. Furthermore, for the same reason, we had to include all eligible patients by the census method (convenient sampling method) and could not randomize patients for the study. Moreover, the type of surgery was selected based on the surgeon's opinion, and we could not randomize patients into the groups or match patients in the groups for the baseline characteristics. This type of patient enrollment can increase the chance of bias in the results.
5.2. Conclusions
In conclusion, the results of the present study demonstrated that children aged ≤ 19 years could successfully undergo OAGB with a significant reduction in weight, BMI, and other anthropometric variables, such as WC and HC, until three years after surgery which were comparable to LSG. Therefore, OAGB is suggested as an efficient weight loss procedure for children and adolescents. Although there were no short- or long-term complications in our study, the small sample size in each group necessitates larger studies on larger populations to determine the complication rates of OAGB in children and adolescents compared to LSG or other bariatric techniques.
Acknowledgements
References
-
1.
Hruby A, Hu FB. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics. 2015;33(7):673-89. [PubMed ID: 25471927]. [PubMed Central ID: PMC4859313]. https://doi.org/10.1007/s40273-014-0243-x.
-
2.
Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161. [PubMed ID: 28480197]. [PubMed Central ID: PMC5401682]. https://doi.org/10.21037/atm.2017.03.107.
-
3.
van Dommelen P, Schonbeck Y, van Buuren S, HiraSing RA. Trends in a life threatening condition: morbid obesity in dutch, Turkish and Moroccan children in The Netherlands. PLoS One. 2014;9(4). e94299. [PubMed ID: 24732729]. [PubMed Central ID: PMC3986047]. https://doi.org/10.1371/journal.pone.0094299.
-
4.
Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9(5):322-9. [PubMed ID: 19560993]. [PubMed Central ID: PMC2746875]. https://doi.org/10.1016/j.acap.2009.04.005.
-
5.
Farrant B, Utter J, Ameratunga S, Clark T, Fleming T, Denny S. Prevalence of severe obesity among New Zealand adolescents and associations with health risk behaviors and emotional well-being. J Pediatr. 2013;163(1):143-9. [PubMed ID: 23357187]. https://doi.org/10.1016/j.jpeds.2012.12.043.
-
6.
Pan L, Blanck HM, Sherry B, Dalenius K, Grummer-Strawn LM. Trends in the prevalence of extreme obesity among US preschool-aged children living in low-income families, 1998-2010. JAMA. 2012;308(24):2563-5. [PubMed ID: 23268509]. [PubMed Central ID: PMC4597777]. https://doi.org/10.1001/jama.2012.108099.
-
7.
Wolfe BM, Kvach E, Eckel RH. Treatment of Obesity: Weight Loss and Bariatric Surgery. Circ Res. 2016;118(11):1844-55. [PubMed ID: 27230645]. [PubMed Central ID: PMC4888907]. https://doi.org/10.1161/CIRCRESAHA.116.307591.
-
8.
Kagan J, Balliro J, Carr-Locke D, Dann M, Guterman L, Ikramuddin S, inventors. Apparatus and methods for treatment of morbid obesity. USA. 2015.
-
9.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427-36. [PubMed ID: 23338049]. https://doi.org/10.1007/s11695-012-0864-0.
-
10.
Sundbom M. Laparoscopic revolution in bariatric surgery. World J Gastroenterol. 2014;20(41):15135-43. [PubMed ID: 25386062]. [PubMed Central ID: PMC4223247]. https://doi.org/10.3748/wjg.v20.i41.15135.
-
11.
Georgiadou D, Sergentanis TN, Nixon A, Diamantis T, Tsigris C, Psaltopoulou T. Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Relat Dis. 2014;10(5):984-91. [PubMed ID: 24913595]. https://doi.org/10.1016/j.soard.2014.02.009.
-
12.
Abed O, Kabir A, Jesmi F, Janani L, Alibeigi P, Abdolhosseini M, et al. Laparoscopic Roux-en-Y versus One Anastomosis Gastric Bypass on Remission of Diabetes in Morbid Obesity. J Minim Invasive Surg Sci. 2017;6(3). e55991. https://doi.org/10.5812/minsurgery.55991.
-
13.
Jammu GS, Sharma R. A 7-Year Clinical Audit of 1107 Cases Comparing Sleeve Gastrectomy, Roux-En-Y Gastric Bypass, and Mini-Gastric Bypass, to Determine an Effective and Safe Bariatric and Metabolic Procedure. Obes Surg. 2016;26(5):926-32. [PubMed ID: 26337694]. https://doi.org/10.1007/s11695-015-1869-2.
-
14.
Wang FG, Yu ZP, Yan WM, Yan M, Song MM. Comparison of safety and effectiveness between laparoscopic mini-gastric bypass and laparoscopic sleeve gastrectomy: A meta-analysis and systematic review. Medicine (Baltimore). 2017;96(50). e8924. [PubMed ID: 29390281]. [PubMed Central ID: PMC5815693]. https://doi.org/10.1097/MD.0000000000008924.
-
15.
Pazouki A, Mokhber S, Riazi S, Alibeigi P, Abdolhosseini M, Jesmi F. Assessment of Surgical Complications in Morbid Obese Patients, The Candidates for 2 Methods of Laparoscopic Bariatric Surgery (Laparoscopic Gastric Bypass, Laparoscopic Sleeve Gastrectomy). J Minim Invasive Surg Sci. 2015;4(4):100-10. https://doi.org/10.17795/minsurgery-19040.
-
16.
Black JA, White B, Viner RM, Simmons RK. Bariatric surgery for obese children and adolescents: a systematic review and meta-analysis. Obes Rev. 2013;14(8):634-44. [PubMed ID: 23577666]. https://doi.org/10.1111/obr.12037.
-
17.
Inge TH, Zeller MH, Jenkins TM, Helmrath M, Brandt ML, Michalsky MP, et al. Perioperative outcomes of adolescents undergoing bariatric surgery: the Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study. JAMA Pediatr. 2014;168(1):47-53. [PubMed ID: 24189578]. [PubMed Central ID: PMC4060250]. https://doi.org/10.1001/jamapediatrics.2013.4296.
-
18.
De La Cruz-Munoz N, Lopez-Mitnik G, Arheart KL, Miller TL, Lipshultz SE, Messiah SE. Effectiveness of bariatric surgery in reducing weight and body mass index among Hispanic adolescents. Obes Surg. 2013;23(2):150-6. [PubMed ID: 22918552]. [PubMed Central ID: PMC3538108]. https://doi.org/10.1007/s11695-012-0730-0.
-
19.
Inge TH, Courcoulas AP, Jenkins TM, Michalsky MP, Helmrath MA, Brandt ML, et al. Weight Loss and Health Status 3 Years after Bariatric Surgery in Adolescents. N Engl J Med. 2016;374(2):113-23. [PubMed ID: 26544725]. [PubMed Central ID: PMC4810437]. https://doi.org/10.1056/NEJMoa1506699.
-
20.
Paulus GF, de Vaan LE, Verdam FJ, Bouvy ND, Ambergen TA, van Heurn LW. Bariatric surgery in morbidly obese adolescents: a systematic review and meta-analysis. Obes Surg. 2015;25(5):860-78. [PubMed ID: 25697125]. [PubMed Central ID: PMC4428750]. https://doi.org/10.1007/s11695-015-1581-2.
-
21.
Rahmani A, Sayehmiri K, Asadollahi K, Sarokhani D, Islami F, Sarokhani M. Investigation of the Prevalence of Obesity in Iran: a Systematic Review and Meta-Analysis Study. Acta Med Iran. 2015;53(10):596-607. [PubMed ID: 26615371].
-
22.
Jafari-Adli S, Jouyandeh Z, Qorbani M, Soroush A, Larijani B, Hasani-Ranjbar S. Prevalence of obesity and overweight in adults and children in Iran; a systematic review. J Diabetes Metab Disord. 2014;13(1):121. [PubMed ID: 25610814]. [PubMed Central ID: PMC4301060]. https://doi.org/10.1186/s40200-014-0121-2.
-
23.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11(3):276-80. [PubMed ID: 11433900]. https://doi.org/10.1381/096089201321336584.
-
24.
Till H, Bluher S, Hirsch W, Kiess W. Efficacy of laparoscopic sleeve gastrectomy (LSG) as a stand-alone technique for children with morbid obesity. Obes Surg. 2008;18(8):1047-9. [PubMed ID: 18459015]. https://doi.org/10.1007/s11695-008-9543-6.
-
25.
Boza C, Viscido G, Salinas J, Crovari F, Funke R, Perez G. Laparoscopic sleeve gastrectomy in obese adolescents: results in 51 patients. Surg Obes Relat Dis. 2012;8(2):133-7. discussion 137-9. [PubMed ID: 22433934]. https://doi.org/10.1016/j.soard.2011.11.021.
-
26.
Alqahtani A, Elahmedi M, Qahtani AR. Laparoscopic Sleeve Gastrectomy in Children Younger Than 14 Years: Refuting the Concerns. Ann Surg. 2016;263(2):312-9. [PubMed ID: 26496081]. https://doi.org/10.1097/SLA.0000000000001278.
-
27.
Mahawar KK, Jennings N, Brown J, Gupta A, Balupuri S, Small PK. "Mini" gastric bypass: systematic review of a controversial procedure. Obes Surg. 2013;23(11):1890-8. [PubMed ID: 23934271]. https://doi.org/10.1007/s11695-013-1026-8.
-
28.
Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SC, Chen JC. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22(12):1827-34. [PubMed ID: 23011462]. https://doi.org/10.1007/s11695-012-0726-9.
-
29.
Carbajo Caballero MA, Vázquez-Pelcastre R, Aparicio-Ponce R, Luque de Leon E, Jimenez JM, Ortiz-Solorzano J, et al. 12-year old adolescent with super morbid obesity, treated with laparoscopic one anastomosis gastric bypass (LOAGB/BAGUA): A case report after 5-year follow-up. Nutr Hosp. 2015;31(5):2327-32. [PubMed ID: 25929410]. https://doi.org/10.3305/nh.2015.31.5.8884.
-
30.
Carbajo MA, Gonzalez-Ramirez G, Jimenez JM, Luque-de-Leon E, Ortiz-de-Solorzano J, Castro MJ, et al. A 5-Year Follow-up in Children and Adolescents Undergoing One-Anastomosis Gastric Bypass (OAGB) at a European IFSO Excellence Center (EAC-BS). Obes Surg. 2019;29(9):2739-44. [PubMed ID: 31049849]. https://doi.org/10.1007/s11695-019-03908-2.
-
31.
Noun R, Skaff J, Riachi E, Daher R, Antoun NA, Nasr M. One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg. 2012;22(5):697-703. [PubMed ID: 22411569]. https://doi.org/10.1007/s11695-012-0618-z.
-
32.
Carbajo MA, Luque-de-Leon E, Jimenez JM, Ortiz-de-Solorzano J, Perez-Miranda M, Castro-Alija MJ. Laparoscopic One-Anastomosis Gastric Bypass: Technique, Results, and Long-Term Follow-Up in 1200 Patients. Obes Surg. 2017;27(5):1153-67. [PubMed ID: 27783366]. [PubMed Central ID: PMC5403902]. https://doi.org/10.1007/s11695-016-2428-1.