Abstract
Context:
Cancer diagnosis and its therapeutic methods can lead to considerable psychological problems and decrease the levels of hope in patients. Due to the considerably important multidimensional effects of hope on the life of patients with cancer, this study aimed to assess the effect of psycho-socio-spiritual strategies on the hope level of patients with cancer.Evidence Acquisition:
In this narrative review, electronic databases were searched including Google Scholar, Scientific Information Database, Magiran, PubMed, ScienceDirect, Web of Science (ISI), Ovid, and Scopus. Those articles published between 1978 and 2020 were retrieved and assessed through the abstract and full-text appraisal. Finally, 74 articles were included in this study.Results:
Psycho-socio-spiritual strategies for affecting the hope level of patients with cancer were classified as follows: (1) psychological interventions (psychotherapy, counseling, coping skills training, stress management training, crisis management, individual or group supporting therapy, hope therapy, and psychoeducational interventions); (2) social interventions (social and family support intervention); and (3) spiritual interventions (logotherapy, religion therapy, and praying).Conclusions:
Due to the chronic nature of cancer disease, in addition to the important role of pharmacological treatment such as chemotherapy and radiotherapy, considering non-pharmacological approaches such as hope-fostering interventions for these patients is essential and can lead to a better quality of life.Keywords
1. Context
Cancer is one of the major burdens of disease worldwide (1-3). The psychological aspects of cancer diagnosis and its physical complications can negatively affect all dimensions of the patients’ and their families' lives (1, 4). They are exposed to psychological problems such as anxiety, depression, hopelessness, social isolation, fear of death, sense of confusion, loss of control, and increased feelings of vulnerability (5-7). These symptoms have significantly negative effects on the beginning and exacerbation of cancer (8). Literature shows that most published articles about the level of hope among individuals have been conducted on patients suffering from cancer, which is due to the considerable negative effects of cancer on patient's hope and life expectancy, compared to other chronic diseases (9).
Hope is defined as a complicated multi-dimensional, vibrant, and important factor in the patient’s effective compliance, perceived control, and survival during the disease (10-13). In another definition, hope is identified as one of the most essential elements in the life of patients with cancer and is considered a fostering coping strategy that includes positive thoughts toward the future, providing the ability for problem-solving, motivation to determine goals, and the desire to increase cooperation in therapeutic programs and psychological adjustment to the illness (10, 12, 14-19). Based on the results of a study, the prevalence of anxiety and depression among newly diagnosed cancer patients was 39.6 and 25.0%, respectively (20). It is supposed that the presence of hope can improve physical and psychological well-being, easy acceptance of the disease, anger level, and other negative psychological symptoms (12, 15, 21). The hope level of patients with cancer seems to be related to a variety of factors consisting of physical (pain severity and energy levels) and psychological (anxiety, depression, and other) symptoms (13, 15, 21, 22). Also, the time since diagnosis, illness stage, and knowledge of diagnosis and treatment were associated with hope in patients (12). Patients need a variety of coping resources to expose to challenging issues during the illness stages such as psychological interventions and social support, providing a sense of meaning in life (2).
Due to the considerably important multidimensional effects of hope on the life of patients with cancer, the recognition of effective strategies for improving the hope level appears to be very noticeable and this study aimed to assess the effectiveness of psycho-socio-spiritual strategies on the hope level of patients with cancer.
2. Evidence Acquisition
This narrative review was performed in five main steps: Identification of the research question, comprehensive literature searches to retrieve articles, study selection, ethical considerations, and data extraction (23).
2.1. Identification of the Research Question
The research question was defined as: What are the effective psycho-socio-spiritual strategies on the hope level of patients with cancer?
2.2. Comprehensive Literature Searches to Find Relevant Articles
Two researchers (MA and FE) independently searched the following databases to find relevant studies: (1) Google Scholar, (2) Scientific Information Databases (SID), (3) Magiran, (4) ScienceDirect, (5) PubMed, (6) Web of Science (ISI), (6) Ovid, and (7) Scopus. The following keywords found through the MeSH strategy were used to find articles published between 1978 and 2020: ["hope" OR "life expectancy"] AND ["strategies" OR "effective strategies" OR "copying styles" OR "psychological strategies" OR "psychological intervention" OR "mental health intervention" OR "psychotherapy" OR "psycho-spiritual therapy" OR "spiritual therapy" OR "hope therapy" OR "meaning therapy" OR "social support therapy" OR "family support] AND ["cancer" OR "neoplasm" OR "oncology"].
2.3. Study Selection
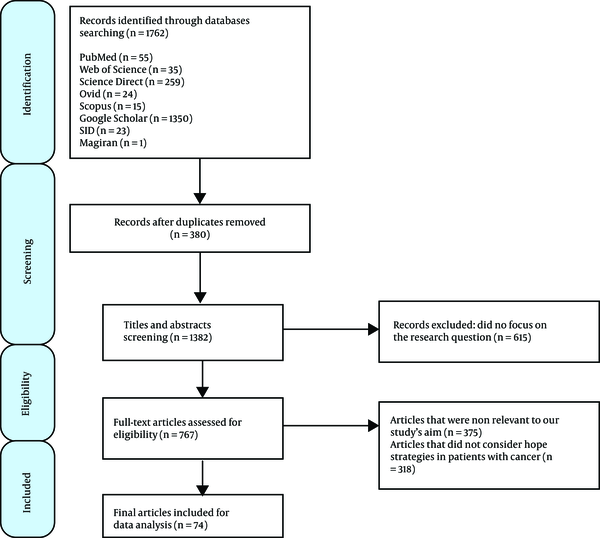
The initial comprehensive literature searches led to the retrieval of 1,762 articles. Two researchers (MA and FE) conducted the title and abstract screening independently and selected the relevant articles according to the inclusion criteria such as being published in the scientific and valid journals in Persian or English languages and referring to effective psycho-socio-spiritual strategies to increase the hope level in cancer patients. After removing repeated articles (n = 380), 1,382 articles remained in this step. In the abstract screening step, 615 articles were excluded due to not focusing on the study's research question. Also, in full-text assessment, articles that did not refer to effective strategies (n = 318) or had irrelevant objectives (n = 375) were excluded from this study. Finally, 74 documents were included in this study (Figure 1).
The search flow diagram based on PRISMA guidelines
2.4. Ethical Considerations
In this study, researchers attempted to follow the ethical considerations and general standards regarding publication with respect to plagiarism, misconduct, data fabrication, double publication, or submission.
2.5. Data Extraction
The full texts of the included articles were studied carefully, and the relevant and required data were extracted and used for writing the findings of this study.
3. Results
The results are classified into three main categories such as psychological interventions, social and family support interventions and spiritual strategies. The characteristics of the included studies are listed in Table 1.
Characteristics of Included Studies Regarding Strategies for Hope in Patients with Cancer
| Authors | Year of Study | Type of Study | Country | Patients Number | Type of Intervention | Results of Studies |
|---|---|---|---|---|---|---|
| Wood, P. E. (24) | 1978 | Pilot study | California, Irvine | 15 | Group counseling | Closed-ended group counseling that does not include family members and is homogeneous for the stage of the disease is most useful. |
| Mickley, J. R. (25) | 1992 | Cross-sectional | San Antonio, Texas | 175 | - | Hope was positively associated with psychological well-being. |
| Helgeson, V. S. (6) | 1996 | Review | Pennsylvania, USA | Electronic search | Peer discussion groups compared to educational groups | Peer discussion groups to provide emotional support were less effective than educational groups to provide informational support. |
| Rustoen, T. (26) | 1998 | Review | Norway | Electronic search | An intervention program based on Nowotny’s definition of hope including eight sessions of belief in oneself and yourself ability, emotional reactions, relations with others, active involvement, spiritual beliefs and belief in the future | The patients' hope was considerably increased in this study. |
| Rustoen, T. (27) | 1998 | Clinical trial | Norway | 96 | learning to live with cancer program | The level of hope was significantly increased in the intervention group (hope therapy group). |
| Herth, K. (10) | 2000 | Clinical trial | Minnesota, USA | 115 | Hope therapy | Treatment groups had significantly higher levels of hope compared to the control group. |
| Leydon, G. M. (28) | 2000 | Qualitative | London | 17 | Depth interviews with patients regarding information needs and information-seeking behavior. | Cancer patients' attitudes to cancer and their strategies for coping with their illness were so that they wished information and tried to obtain it. |
| Antoni, M. H. (29) | 2001 | Clinical trial | Miami, Florida | 100 | Group cognitive-behavioral stress management intervention. | Only the prevalence of moderate depression decreased. The intervention also had positive effects on the patients’ lives and generalized optimism. |
| Stanton, A. L. (30) | 2002 | Cohort | Lawrence, USA | 70 | Situation-specific coping strategies | Coping through turning to religion would be more effective for less hopeful women and mixed support emerged for the approach-oriented coping strategies. |
| Klemm, P. (31) | 2003 | Review | USA | Electronic search | Online cancer support groups | This intervention increased patients seeking treatment. In issues such as negative psychological problems, women used online cancer support groups. |
| Weaver, A. J. (32) | 2004 | Review | New York, USA | Electronic search | Religion/spirituality intervention | In patients using spiritual and religious beliefs, coping with their illness was more successful and they accepted their disease and tried to deal with it positively. |
| Pour Ghaznain, T. (33) | 2005 | Cross-sectional | Iran, Mashhad | 100 | - | Patients that prayed and were in contact with physicians and nurses had no physical problems and financial distress. |
| Hendricks-Ferguson, V. (34) | 2006 | Cross-sectional | USA | 78 | - | The progressive stage of disease or gender may influence the adolescents' hope level, spiritual and religious well-being, and successful cope during cancer. |
| Taleghani, F. (35) | 2006 | Qualitative | Iran, Tehran | 19 | Interviews using a content analysis method about coping in cancer | Coping with the disease was associated with the use of a religious approach, thinking about illness, positively accepting the fact of the disease, and seeking and finding support from the family and others. |
| Vellone, E. (12) | 2006 | Cross-sectional | Italy | 80 | - | Factors such as anxiety, depression, and boredom during hospitalization were associated with unhopefulness. |
| Duggleby, W. D. (17) | 2007 | Clinical trial | Saskatchewan, Canada | 60 | Living with hope program, consisting of viewing an international award-winning video on hope and a choice of one of three hope activities to work on over one week | Patients in the intervention group had statistically significantly higher hope levels and increased quality-of-life scores than patients in the control group. |
| Abdi, N. (36) | 2007 | Controlled randomized trial | Iran, Sanandaj | 50 | Depth discussion, face-to-face method, and problem-based learning | There was no significant difference between the case and control groups before hope promotion intervention. |
| Moryl, N. (37) | 2008 | Case report | California, USA | 1 | Managing an acute pain crisis | The palliative care team helped the patients address their goals of care and achieve their psychological, social, and existential needs. |
| Elsayem, A. (38) | 2004 | Cross-sectional | Houston, Texas | 320 | Palliative care | The mean reimbursement rate for all palliative care changes was approximately 57%, and the mean daily changes in the palliative care in the patient service were 38% lower than the mean daily changes for the rest of the hospital. |
| Mattioli, J. L. (39) | 2008 | Qualitative | USA | 14 | Semi-structured interviews regarding the personal meaning of hope and social support | Receiving support from the family, friends, and healthcare providers was associated with better dealing with the disease and treatment. |
| Sanatani, M. (16) | 2008 | Cohort | Canada | 50 | 29 curative-intent; 21 palliative care | There were no differences in hope level between patients in the two intervention groups. |
| Holt, C. L. (40) | 2009 | Qualitative | Birmingham, England | 23 | 1 - 1.5 hour interviews regarding religiosity in coping | Hope was considered a predictor mediator between religiosity and three coping styles. Themes such as control over illness, emotional response to disease, the importance of social support, the role of God and praying as healers for them, and the importance of faith for recovery were extracted. |
| Hasson-Ohayon, I. (41) | 2009 | Cross-sectional | Israel | 233 | - | - |
| Kang, K. (42) | 2009 | Clinical trial | Korea | 29 | Effect of logotherapy on suffering, finding meaning, and spiritual well-being | Logotherapy was associated with improving the meaning of life and decreased suffering from cancer diagnosis among patients. |
| Hosseinian, E. (43) | 2010 | Clinical trial | Iran, Ahvaz | 40 | Group logotherapy | There were significant differences in life expectancy increase between the logotherapy group and control group. |
| Rustoen, T. (44) | 2011 | Cohort | Norway | 195 | Hope intervention | More than 95% of the patients reported that this intervention was useful for them. |
| Fallah, R. (45) | 2011 | Case-control | Iran, Tehran | 60 | Integrating spirituality into a group psychotherapy program | The spiritual intervention led to promoting hope and life satisfaction among patients. |
| Moradian, S. (46) | 2012 | Qualitative | Iran, Mashhad | 30 | Interviews about Iranian cancer patients' needs from patients' perspective | The negative effect of cancer on a patient's daily life was more than the suffering due to physical symptoms and its treatment. Some issues including financial distress regarding treatment costs and the possibility of being unable to work due to the disease were the most concerns of patients with cancer. |
| Carey, M. (47) | 2012 | Systematic review | Australia | Electronic search | - | Most interventional studies showed the limited effects on cancer patients’ unmet needs. |
| Rahnama, M. (48) | 2012 | Qualitative | Iran, Tehran | 11 | Semi-structured interviews regarding patients’ perception of spirituality | God as the spiritual truth, morality as a spiritual sign, and spiritual resources as the source of hope were the main themes extracted from interviews. |
| Kavradim, S. T. (49) | 2013 | Cross-sectional | Turkey | 240 | - | Factors such as family income, level of knowledge of the disease, feeling of healing, and interpretation of higher family support were associated with higher hope levels and factors such as anxiety or concern and fear were independently related to the disturbed hope level. |
| Duggleby, W. (13) | 2013 | Cross-sectional | Canada | 310 | - | The age of above 65 was associated with higher levels of hope among patients. Also, the male gender was effective in the patient’s hope level. |
| Jafari, N. (50) | 2013 | Controlled clinical trial | Iran, Isfahan | 65 | Spiritual therapy | Participation in the spiritual therapy program was associated with increased spiritual well-being and quality of life among patients. |
| Farhadi, M. (1) | 2014 | Clinical trial | Iran, Hamedan | 42 | Group meaning-centered hope therapy | Participation of patients and their families in this intervention was associated with increased quality of life. |
| Felder, B. E. (14) | 2004 | Cross-sectional | Philadelphia, USA | 183 | - | The level of hope among patients was significantly high and positively related to coping in patients regardless of their demographic characteristics such as gender, age, marital status, education, or site of malignancy. |
| Lotfi, K. F. (51) | 2014 | Clinical trial | Iran, Tehran | 30 | Hope therapy | This intervention reduced distress in women with breast cancer. |
| Soroush, M. (52) | 2015 | Qualitative study | Iran, Tehran | 20 | Semi-structured interviews regarding psychological features and hope | Some patients showed positive psychological characteristics such as extraversion, sociability, sincerity, altruism, resilience, and optimism, and some negative features such as anxiety, loneliness, depression, sadness, anger, and frustration manifest. Overall, the majority of patients were hopeful about the future. |
| Tamadon, A. (8) | 2015 | Clinical trial | Iran, Shiraz | 30 | Hope therapy on improving the resilience of patients | Hope therapy was an appropriate strategy for increasing resilience among patients with blood cancer. |
| Fathollahzade, A. (53) | 2015 | Cross-sectional | Iran, Tabriz | 262 | - | Iranian patients with cancer had moderate to high levels of financial distress regarding treatment costs. |
| Gassmann, C. (54) | 2016 | Qualitative | Switzerland | 6 | Open interviews in patients undergoing oral chemotherapy | In this study, the samples showed the physical and emotional reluctance towards oral chemotherapy due to its toxic side effects. |
| Yousefi, E. (55) | 2016 | Clinical trial | Iran, Qeshm | 30 | Hope therapy training | Hope therapy was an appropriate mediator of increasing resilience among women with cancer. |
| Mahdian, Z. (56) | 2016 | Cross-sectional | Iran, Mazandaran | 198 | - | The direct and indirect effects of spiritual well-being on hope were positive and significant |
| Li, P. (57) | 2018 | Meta-analysis | China | - | Nursing intervention on cancer patient's hope | The nursing intervention had a positive and satisfactory effect on the level of hope in patients with cancer. |
| Pourfaraj, M. (58) | 2018 | Cross-sectional | Iran | 40 | Positive psychotherapy | Positive psychotherapy increased the happiness and hope level among cancer patients compared to the control group. |
| Fischer, I. C. (59) | 2018 | Cross-sectional | USA | 84 | Being hopeful and optimistic may be associated with various dimensions of psychological distress in patients living with advanced stages of cancer. | |
| Ozen, B. (60) | 2019 | Cross-sectional | Turkey | 106 | - | Patients with cancer had relatively higher hope levels. The patients’ thoughts about death affected their hope level through direct and indirect paths. |
| Bastian, T. D. (61) | 2020 | Qualitative phenomenologic descriptive | USA | 52 | - | Survival informed other survivors regarding their lived experiences during their disease. which was characterized by themes such as listen to your body, advocate for yourself, embrace your culture and spirituality, and share your story with others. |
3.1. Psychological Strategies
Factors such as cancer diagnosis, its treatment, and concerns for survival can increase the psychological distress among patients; so, they might have a negative effect on their adaptation to the disease (44, 59). There are many psychological strategies to improve the level of hope among patients with cancer (1, 44, 60) including psychotherapy, counseling, coping skills training, stress management training, crisis management, individual or group supporting therapy, and hope therapy (6, 26, 29, 31, 37). These interventions can be performed by psychiatrists or other healthcare providers such as nurses, family physicians, and psychologists (57). These interventions aim to reduce stress, increase hope for the recovery and expansion of the relationships and social activities, and improve the mental health of the patients (52).
3.1.1. Psychotherapy
A psychotherapy intervention can lead to the improvement of patient’s quality of life through the promotion of the hope level among them (1, 58). Literature regarding the efficacy of psychotherapy in patients with cancer shows that group psychotherapy influences the patient's quantity of life such as years of survival, pain level reduction, reduction of the possibility of mood disorders, and improvement of social activities (1, 45). Based on the published studies, holding individual and group counseling sessions with different parts such as stress and crisis management for these patients is associated with appropriate and satisfactory therapeutic results (24, 62, 63).
3.1.2. Coping Styles Improvement
Interventions on coping styles are used in patients with a high or low level of hope to guide them to cope effectively with cancer diagnosis and acceptance (10, 17, 54). Coping styles such as confronting and evasive coping styles are the most effective ones and are used in patients with cancer. Confronting coping styles are used for the improvement of constructive problem-solving, and evasive coping styles are applied in avoidance behaviors (14, 17).
Other coping styles referred to in different studies regarding cancer consist of active approaches toward stressors, such as seeking social support, problem-solving-based coping styles, positive attitudes and thinking, positive reinterpretation, active acceptance, and passive or avoidant coping styles, which may be applied for appropriate adjustment with the disease in women with low hope level (30, 32, 35, 36). A comparative study revealed that participants in the coping skills training group showed better psychological adjustment than patients in the non-therapeutic group (26).
Coping skills training includes behavioral and psychological techniques for the patients. Behavioral techniques may include relaxation training, activity planning, determining goals, and information seeking (14, 26, 30). Mental techniques may consist of recovering the feelings, experiencing a social sense with others, acknowledging a sense of altruism with giving, and receiving support (26).
3.1.3. Hope Therapy
Hope therapy is a special strategy that applies the positive psychology approach without emphasizing disabilities and it can decrease psychological distress (51). Psychologically, hope therapy is viewed as a strong therapeutic strategy that helps the patient's mental health by strengthening resilience in the patients (8, 49). Issues that are assessed in hope therapy sessions include problem-solving-based learning and the patient's active participation in the discussion topics such as positive self-speaking, hopeful imagination, following a healthy and useful diet, regular daily sports, and effective connection with supportive networks (9). Cognitive-behavioral therapy and solution-focused therapy are used by healthcare providers in this strategy. This strategy aims to provide educational and theoretical services and hope promotion programs such as helping patients to formulate their specific goals, consider some hypothetical gates for reaching them, motivating to follow them and overcome problems and barriers (8, 17, 55, 64).
3.1.4. Psychoeducational Interventions
Psychoeducational interventions are strategies provided by nurses and other healthcare providers in clinics or hospitals (12, 27). The knowledge of healthcare providers regarding effective strategies on increasing hope is significantly important in the therapeutic trend (8, 10, 16). The purpose of the nursing interventions is to help patients cope with illness and its suffering and find the meaning of life in this specific situation (40). Nurses’ behaviors have an important role in inspiring and provoking hope in different ways (27). The most important roles of the nurses include active listening, providing emotional support for patients, demonstrating caring behaviors, giving knowledge and information about the therapeutic options and recovery, promoting the awareness of life, identifying the cause of life, providing comfort, and helping patients to set superior goals (2, 12, 14, 25, 40, 47, 65). Also, nurses can regulate the process of rehabilitation and help the patient adapt to the disease and its divergence (27).
3.2. Social and Family Support Intervention
3.2.1. Family Support
Most studies showed that family and close friends' support was the strongest predictor of hope in patients with cancer and had a positive impact on the level of hope (6, 13, 16, 18, 21, 40, 56). Studies revealed that having sympathetic and careful caregivers at home or during the therapeutic processes and sessions was considerably associated with a higher level of hope in patients with cancer (66, 67). Based on the results of the studies, cancer patients often have financial distress regarding the high costs of cancer diagnosis and treatment (53). Financial distress in these patients may result from two main issues such as temporary or permanent loss of occupation and long-term costs of cancer treatment (46). Therefore, these concerns and distresses may be associated with the negative outcomes in the patient’s decision-making for following or continuing therapeutic sessions. Notably, providing a supportive economic environment such as considering therapeutic insurance for special treatments such as chemotherapy, radiotherapy, and cancer medications that patients receive without financial concern is associated with higher hope levels and better therapeutic outcomes (38).
3.2.2. Social Support
The role of social support as an important key predictor of hope in patients with cancer has been referred to extensively in most published studies regarding cancer (18, 25, 39, 56, 67, 68). Overall, the social support resource will assist patients to share their thoughts, experiences, and concerns about their illness and receive sympathetic reactions from others (18, 69). According to the results of studies, there are two main types of supportive social support including emotional and instrumental support.
Emotional support includes verbal and non-verbal communication consisting of listening, focusing, and comforting. Emotional support can help the patients to promote their sense of self-esteem and reduce the sense of insufficiency by understanding their values and roles in their personal lives (6). Instrumental support includes providing goods material such as transportation and appropriate therapeutic methods (6, 18, 65).
According to the results of a study, hospice care is offered when life expectancy is six or fewer months. Hospice and palliative care is a special strategy that is considered for patients in the end-stage of the illness and their caregivers are to develop a personal relationship (11). Hospice care can be delivered by an interdisciplinary team, such as physicians, nurses, home health aides, clergy, and trained caregivers. In addition to focusing on the disease and treatment, this strategy emphasizes the quality of life of patients and their families (11, 70). During the caring period, patients should be assisted to have a high-quality life through seeking the meaning of their lives (28).
3.2.3. Support Group Therapy
Support group therapy is mentioned as one of the most effective strategies for improving the sense of life expectancy in patients with cancer (8). These group therapies are mostly constructed of informal and non-structured sessions aiming at assisting patients to express their health concerns, needs, and fears regarding their health status freely (27). Support groups in patients based on their initial focus can be classified into two main categories. The first category is the insight-oriented support group, assessing affective concerns. The second category emphasizes training and behavior and its aim is to promote cognitive awareness and coping skills (27).
3.3. Spiritual Strategies
Spiritual interventions are mentioned as an effective non-pharmacological strategy in curing many chronic illnesses and coping with severe pain of diseases (45, 50, 61). Also, several studies showed that having spiritual beliefs is significantly associated with higher hope and psychological well-being in patients with cancer (12, 41, 45). Spirituality might include aspects of religious faith to the meaning of life and internal peace (41). Spirituality can also reduce negative psychological problems such as anxiety, depression, and anger by filling the gap between something individuals have and something they want to achieve and also can assist patients to facilitate the acceptance of their disease and increase their life satisfaction (45).
Studies show that religious and spiritual strategies have been applied by many psychologists and psychiatrists in the management process of patients with cancer (25, 45). Asking the patients regarding God and the role of religious belief in their lives can be an important step to initial assessment and management in spiritual therapy (25). Different methods can be used in the spiritual therapy process.
3.3.1. Logotherapy
Logotherapy is a specific treatment that consists of a spiritual approach for the root of the problem that helps the patients to encourage themselves for their responsibilities, such as achieving the sense of freedom of psychological distress and overcome existential emptiness and enhance the meaning and goal of their lives (42, 43). Logotherapy invites humans towards the effort, hope, and activity by taking into account the transience of human existence rather than pessimism and isolation (71). Based on the results of a study that assessed the effectiveness of short-term group logotherapy in life expectancy and resilience of women with breast cancer, group logotherapy could assist women with breast cancer to find meaning in their lives, receive support from groups, and adapt themselves to the disease. Also, logotherapy could be useful in patient’s attitudes towards the challenges and problems during the disease process and could increase their strength and resilience (72).
3.3.2. Religion Therapy
One aspect of spirituality that is studied in most of the studies regarding hope is religion and its role in patient’s hope. Religion is mentioned as an important and key predictor of compatible adjustment and positive coping with chronic diseases, such as cancer (12, 19, 41, 44). Religion is a complex concept that has a deep effect on cancer patients (11, 25). Also, religious identity was associated with fewer psychological symptoms such as anxiety and spiritual well-being and beliefs (41).
Religious resources such as God, imams, and the prophet play fundamental roles in long-term coping with an illness such as maintaining self-esteem, higher psychological well-being, and appropriate and compatible comfort and hope, as well as promoting the sense of meaning and goals in life (32, 40, 48, 69). The prevalence of religious coping depends on some factors such as the type of stressors, sample characteristics, type and stage of illness, the status of remission condition, and therapeutic options. A literature review showed that for patients in the terminal stage of the disease, the importance of religious and spiritual well-being may be more than that of physical health (32, 73).
3.3.3. Praying
Among patients, prayer was found to be helpful, effective, and associated with hope and positive psychological outcomes (33, 34, 40). Prayer was considered a significantly important factor in positive coping with and healing from cancer (26, 40). Also, it is believed that prayer decreases negative emotions such as anger, depression, and fear such that a study found that praying alone or with others was the most common coping strategy in patients with cancer (32). In the patient’s idea, God was seen as a provider of comprehensive insights or cognition and a great sense of comfort and strength to the patients.
4. Discussion
The present study aimed to determine the effect of psycho-socio-spiritual strategies on the hope level of patients with cancer. Hope is a significant concept for patients with cancer to find the meaning of life and adapt to the illness. A good reaction to cancer depends on some factors such as patients’ and their families’ psychological structure, social environment, social support systems, and their relationships with healthcare providers (21). Studies regarding hope in patients with cancer mentioned that hope-inspiring strategies and symptoms management are important in the therapeutic process (74).
Patients with a higher hope level can cope with the disease more successfully through positive acceptance, a normal way of living, and a hopeful belief in the future (19). Also, a high level of hope is associated with low levels of uncertainty, low psychological status, and greater use of positive coping skills (12). There is a mutual relationship between hopeful thoughts and cancer disease. First, hopeful patients more emphasize life and disease reality and are more active and successful in resolving the problems. During the treatment, hopeful patients show more resilience in tolerating long-term and severe treatments and complications of chemotherapy or radiotherapy and are more likely to participate in treatment stages (2, 4).
The most important sources of hope in patients with cancer are spiritual resources such as God, the prophet, imams, family members, friends, and healthcare workers such as physicians and nurses (2, 12). The literature about optimism and hopefulness indicated that optimistic patients in comparison with pessimistic individuals are less likely to show poor physical health, depression, disappointment, and suicide commitment when faced with major stressful life events (4). According to the results of studies, the most common strategies used in patients with cancer were religion and prayer, living with a supportive family, creating relationships with others such as cancer patients, appropriate perceived control and positive thoughts, improving continuous accomplishment, and anticipating survival (19, 30, 73). The strategies used to increase hope were based on four main aspects such as experimental process, spiritual process, rational thinking process, and relationship with physicians (44).
4.1. Limitations
We did not include unpublished studies or grey literature in this study. Also, as the authors were unfamiliar with other languages except for Persian and English, only studies published in these languages were included in this study. Given the mentioned limitations, we suggest that high-quality clinical trials be conducted regarding the effective strategies for hope in these patients.
As cancer patients need to receive counseling regarding hope based strategies, this study results proposed that the presence of a midwife with counseling in midwifery specialty in the oncology ward is an useful action.
5. Conclusion
The results showed that different strategies are used to improve the hope level in patients with cancer. Due to the chronic nature of cancer disease, in addition to pharmacological treatment such as chemotherapy or radiotherapy, considering non-pharmacological approaches such as hope fostering interventions for these patients is essential and can lead to a better quality of life. For improving the ability of hospital personnel regarding hope strategies, it seems helpful to consider periodic training and holding counseling programs for oncology ward nurses regarding psychotherapy styles and crisis management. Also, it is recommended that clergymen or priests and patients’ families settle in the oncology ward.
Acknowledgements
References
-
1.
Farhadi M, Reisi-Dehkordi N, Kalantari M, Zargham-Boroujeni A. Efficacy of group meaning centered hope therapy of cancer patients and their families on patients' quality of life. Iran J Nurs Midwifery Res. 2014;19(3):290-4. [PubMed ID: 24949069]. [PubMed Central ID: PMC4061631].
-
2.
Afrooz R, Rahmani A, Zamanzadeh V, Abdullahzadeh F, Azadi A, Faghany S, et al. The nature of hope among Iranian cancer patients. Asian Pac J Cancer Prev. 2014;15(21):9307-12. [PubMed ID: 25422217]. https://doi.org/10.7314/apjcp.2014.15.21.9307.
-
3.
Moosazadeh M, Hamzehgardeshi Z, Elyasi F, Janbabai G, Rezaei M. [The effect of therapeutic-supportive interventions on body image in women with breast cancer: A systematic review]. J of Health in the Field. 2017;5(1):32-42. Persian.
-
4.
Soraki N, Abolghasemi S. Relationship between happiness and health with a life expectancy of cancer patients. J Curr Res in Sci. 2016;1(2):403.
-
5.
Mohammadi Ziyarati A, Damghani Mirmahalleh M, Asadi J. The effectiveness of mindfulness training on life expectancy in women with breast cancer in Gorgan. Int J humanit. 2016:1247-55.
-
6.
Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Health Psychol. 1996;15(2):135-48. [PubMed ID: 8681922]. https://doi.org/10.1037//0278-6133.15.2.135.
-
7.
Azizi M, Elyasi F, Fariborzifar A. Psychosocial/spiritual interventions for mental health in patients with cancer: A review. Med J Ahwaz Jundishapur Univ Med Sci. 2013;4(1):41-51.
-
8.
Tamadon A. [Evaluate the effectiveness of hope therapy on improving resilience of patients whit blood cancer]. Journal Ump Social Sciences and Technology Management. 2015;3(3):358-62. Persian.
-
9.
Shekarabi-Ahari G, Younesi J, Borjali A, Ansari-Damavandi S. The effectiveness of group hope therapy on hope and depression of mothers with children suffering from cancer in tehran. Iran J Cancer Prev. 2012;5(4):183-8. [PubMed ID: 25352968]. [PubMed Central ID: PMC4209570].
-
10.
Herth K. Enhancing hope in people with a first recurrence of cancer. J Adv Nurs. 2000;32(6):1431-41. [PubMed ID: 11136411]. https://doi.org/10.1046/j.1365-2648.2000.01619.x.
-
11.
Brown C. Hope and quality of life in hospice patients with cancer [master's degree]. Florida, USA: University of South Florida; 2005.
-
12.
Vellone E, Rega ML, Galletti C, Cohen MZ. Hope and related variables in Italian cancer patients. Cancer Nurs. 2006;29(5):356-66. [PubMed ID: 17006108]. https://doi.org/10.1097/00002820-200609000-00002.
-
13.
Duggleby W, Ghosh S, Cooper D, Dwernychuk L. Hope in newly diagnosed cancer patients. J Pain Symptom Manage. 2013;46(5):661-70. [PubMed ID: 23535324]. https://doi.org/10.1016/j.jpainsymman.2012.12.004.
-
14.
Felder BE. Hope and coping in patients with cancer diagnoses. Cancer Nurs. 2004;27(4):320-4. [PubMed ID: 15292728]. https://doi.org/10.1097/00002820-200407000-00009.
-
15.
Abdullah-Zadeh F, Agahosseini S, Asvadi-Kermani I, Rahmani A. Hope in Iranian cancer patients. Iran J Nurs Midwifery Res. 2011;16(4):288-91. [PubMed ID: 23450037]. [PubMed Central ID: PMC3583098].
-
16.
Sanatani M, Schreier G, Stitt L. Level and direction of hope in cancer patients: an exploratory longitudinal study. Support Care Cancer. 2008;16(5):493-9. [PubMed ID: 17891421]. https://doi.org/10.1007/s00520-007-0336-6.
-
17.
Duggleby WD, Degner L, Williams A, Wright K, Cooper D, Popkin D, et al. Living with hope: Initial evaluation of a psychosocial hope intervention for older palliative home care patients. J Pain Symptom Manage. 2007;33(3):247-57. [PubMed ID: 17349494]. https://doi.org/10.1016/j.jpainsymman.2006.09.013.
-
18.
Butt CM. Supporting hope in midlife cancer survivors: Intervention workshop [dissertation]. Massachusetts, USA: Boston College; 2012.
-
19.
Chi GC. The role of hope in patients with cancer. Oncol Nurs Forum. 2007;34(2):415-24. [PubMed ID: 17573305]. https://doi.org/10.1188/07.ONF.415-424.
-
20.
Peh CX, Liu J, Bishop GD, Chan HY, Chua SM, Kua EH, et al. Emotion regulation and emotional distress: The mediating role of hope on reappraisal and anxiety/depression in newly diagnosed cancer patients. Psychooncology. 2017;26(8):1191-7. [PubMed ID: 27723939]. https://doi.org/10.1002/pon.4297.
-
21.
Sheikholeslami F, Nia N, Vardanjani T, Rabiei L, Esmaeili Vardanjani SA, Salehzadeh A, et al. Hope and religious beliefs in Iranian cancer patients. Life Sci. 2012;9(2):1300-3.
-
22.
Hamzehgardeshi Z, Moosazadeh M, Elyasi F, Janbabai G, Rezaei M, Yeganeh Z, et al. Effect of midwifery-based counseling support program on body image of breast cancer women survivors. Asian Pac J Cancer Prev. 2017;18(5):1293-9. [PubMed ID: 28610417]. [PubMed Central ID: PMC5555538]. https://doi.org/10.22034/APJCP.2017.18.5.1293.
-
23.
Cowley S, Whittaker K, Grigulis A, Malone M, Donetto S, Wood H, et al. Why health visiting? A review of the literature about key health visitor interventions, processes and outcomes for children and families. London, UK: National Nursing Research Unit, King’s College London; 2013.
-
24.
Wood PE, Milligan M, Christ D, Liff D. Group counseling for cancer patients in a community hospital. Psychosomatics. 1978;19(9):555-61. [PubMed ID: 704782]. https://doi.org/10.1016/S0033-3182(78)70932-1.
-
25.
Mickley JR, Soeken K, Belcher A. Spiritual well-being, religiousness and hope among women with breast cancer. Image J Nurs Sch. 1992;24(4):267-72. [PubMed ID: 1452180]. https://doi.org/10.1111/j.1547-5069.1992.tb00732.x.
-
26.
Rustoen T, Hanestad BR. Nursing intervention to increase hope in cancer patients. J Clin Nurs. 1998;7(1):19-27. [PubMed ID: 9510704]. https://doi.org/10.1046/j.1365-2702.1998.00126.x.
-
27.
Rustoen T, Wiklund I, Hanestad BR, Moum T. Nursing intervention to increase hope and quality of life in newly diagnosed cancer patients. Cancer Nurs. 1998;21(4):235-45. [PubMed ID: 9691504]. https://doi.org/10.1097/00002820-199808000-00003.
-
28.
Leydon GM, Boulton M, Moynihan C, Jones A, Mossman J, Boudioni M, et al. Cancer patients' information needs and information seeking behaviour: In depth interview study. BMJ. 2000;320(7239):909-13. [PubMed ID: 10742000]. [PubMed Central ID: PMC27332]. https://doi.org/10.1136/bmj.320.7239.909.
-
29.
Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001;20(1):20-32. [PubMed ID: 11199062]. https://doi.org/10.1037//0278-6133.20.1.20.
-
30.
Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psychooncology. 2002;11(2):93-102. [PubMed ID: 11921325]. https://doi.org/10.1002/pon.574.
-
31.
Klemm P, Bunnell D, Cullen M, Soneji R, Gibbons P, Holecek A. Online cancer support groups: A review of the research literature. Comput Inform Nurs. 2003;21(3):136-42. [PubMed ID: 12792194]. https://doi.org/10.1097/00024665-200305000-00010.
-
32.
Weaver AJ, Flannelly KJ. The role of religion/spirituality for cancer patients and their caregivers. South Med J. 2004;97(12):1210-4. [PubMed ID: 15646759]. https://doi.org/10.1097/01.SMJ.0000146492.27650.1C.
-
33.
Pour Ghaznain T, Ghafari F. Study of the relationship between hopefulness and self-esteem in renal transplant recipients at imam reza hospital, Mashhad, Iran, 2002-03. SSU Journals. 2005;13(1):57-61.
-
34.
Hendricks-Ferguson V. Relationships of age and gender to hope and spiritual well-being among adolescents with cancer. J Pediatr Oncol Nurs. 2006;23(4):189-99. [PubMed ID: 16766684]. https://doi.org/10.1177/1043454206289757.
-
35.
Taleghani F, Yekta ZP, Nasrabadi AN. Coping with breast cancer in newly diagnosed Iranian women. J Adv Nurs. 2006;54(3):265-73. [PubMed ID: 16629910]. https://doi.org/10.1111/j.1365-2648.2006.03808_1.x.
-
36.
Abdi N, Taghdisi MH, Naghdi S. [Promoting interventions on cancer patients. A case study in Sanandaj, Iran, in 2007]. Armaghan Danesh. 2009;14(3 (55)):13-21. Persian.
-
37.
Moryl N, Coyle N, Foley KM. Managing an acute pain crisis in a patient with advanced cancer: "This is as much of a crisis as a code". JAMA. 2008;299(12):1457-67. [PubMed ID: 18364488]. https://doi.org/10.1001/jama.299.12.1457.
-
38.
Elsayem A, Swint K, Fisch MJ, Palmer JL, Reddy S, Walker P, et al. Palliative care inpatient service in a comprehensive cancer center: Clinical and financial outcomes. J Clin Oncol. 2004;22(10):2008-14. [PubMed ID: 15143094]. https://doi.org/10.1200/JCO.2004.11.003.
-
39.
Mattioli JL, Repinski R, Chappy SL. The meaning of hope and social support in patients receiving chemotherapy. Oncol Nurs Forum. 2008;35(5):822-9. [PubMed ID: 18765329]. https://doi.org/10.1188/08.ONF.822-829.
-
40.
Holt CL, Caplan L, Schulz E, Blake V, Southward P, Buckner A, et al. Role of religion in cancer coping among African Americans: A qualitative examination. J Psychosoc Oncol. 2009;27(2):248-73. [PubMed ID: 19337932]. [PubMed Central ID: PMC3646589]. https://doi.org/10.1080/07347330902776028.
-
41.
Hasson-Ohayon I, Braun M, Galinsky D, Baider L. Religiosity and hope: a path for women coping with a diagnosis of breast cancer. Psychosomatics. 2009;50(5):525-33. [PubMed ID: 19855039]. https://doi.org/10.1176/appi.psy.50.5.525.
-
42.
Kang KA, Im JI, Kim HS, Kim SJ, Song MK, Sim S. The effect of logotherapy on the suffering, finding meaning, and spiritual well-being of adolescents with terminal cancer. J Korean Acad Child Health Nurs. 2009;15(2):136. https://doi.org/10.4094/jkachn.2009.15.2.136.
-
43.
Hosseinian E, Soudani M, Mehrabizadeh HM. [Efficacy of group logotherapy on cancer patients'life expectation]. Int J Behav Dev. 2010;3(4). Persian.
-
44.
Rustoen T, Cooper BA, Miaskowski C. A longitudinal study of the effects of a hope intervention on levels of hope and psychological distress in a community-based sample of oncology patients. Eur J Oncol Nurs. 2011;15(4):351-7. [PubMed ID: 20870459]. https://doi.org/10.1016/j.ejon.2010.09.001.
-
45.
Fallah R, Golzari M, Dastani M, Akbari ME. Integrating spirituality into a group psychotherapy program for women surviving from breast cancer. Iran J Cancer Prev. 2011;4(3):141-7. [PubMed ID: 26328054]. [PubMed Central ID: PMC4551298].
-
46.
Moradian S, Aledavood SA, Tabatabaee A. Iranian cancer patients and their perspectives: A qualitative study. Eur J Cancer Care. 2012;21(3):377-83. [PubMed ID: 21955041]. https://doi.org/10.1111/j.1365-2354.2011.01293.x.
-
47.
Carey M, Lambert S, Smits R, Paul C, Sanson-Fisher R, Clinton-McHarg T. The unfulfilled promise: A systematic review of interventions to reduce the unmet supportive care needs of cancer patients. Support Care Cancer. 2012;20(2):207-19. [PubMed ID: 22089430]. [PubMed Central ID: PMC3244607]. https://doi.org/10.1007/s00520-011-1327-1.
-
48.
Rahnama M, Khoshknab MF, Maddah SS, Ahmadi F. Iranian cancer patients' perception of spirituality: A qualitative content analysis study. BMC Nurs. 2012;11:19. [PubMed ID: 23043231]. [PubMed Central ID: PMC3500707]. https://doi.org/10.1186/1472-6955-11-19.
-
49.
Kavradim ST, Ozer ZC, Bozcuk H. Hope in people with cancer: A multivariate analysis from Turkey. J Adv Nurs. 2013;69(5):1183-96. [PubMed ID: 22891939]. https://doi.org/10.1111/j.1365-2648.2012.06110.x.
-
50.
Jafari N, Farajzadegan Z, Zamani A, Bahrami F, Emami H, Loghmani A, et al. Spiritual therapy to improve the spiritual well-being of Iranian women with breast cancer: A randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:353262. [PubMed ID: 24023572]. [PubMed Central ID: PMC3759260]. https://doi.org/10.1155/2013/353262.
-
51.
Lotfi Kashani F, Vaziri S, Zine El Abidine SN, Zine El Abidine SN. [Effectiveness of group hope therapy on decreasing psychological distress among women with breast cancer]. J Appl Psychol. 2014;7(4 (28)):45-58. Persian.
-
52.
Soroush M, Hejazi E, Shoakazemi M, Gheranpayeh L. [Body image psychological characteristics and hope in women with breast cancer]. Iran J Breast Dis. 2015;7(4):52-63. Persian.
-
53.
Fathollahzade A, Rahmani A, Dadashzadeh A, Gahramanian A, Esfahani A, Javanganji L, et al. Financial distress and its predicting factors among iranian cancer patients. Asian Pac J Cancer Prev. 2015;16(4):1621-5. [PubMed ID: 25743842]. https://doi.org/10.7314/apjcp.2015.16.4.1621.
-
54.
Gassmann C, Kolbe N, Brenner A. Experiences and coping strategies of oncology patients undergoing oral chemotherapy: First steps of a grounded theory study. Eur J Oncol Nurs. 2016;23:106-14. [PubMed ID: 27456382]. https://doi.org/10.1016/j.ejon.2016.06.001.
-
55.
Yousefi E, Nazemnezhad S, Islami M, SalarHoseini H, Dourandish M. The effectiveness of hope therapy on increasing the resilience of women with cancer. Acad J Psychol Stud. 2016;5(3):261-8.
-
56.
Mahdian Z, Ghaffari M. The mediating role of psychological resilience, and social support on the relationship between spiritual well-being and hope in cancer patients. Fundamentals of Mental Health. 2016;18(3):130-8.
-
57.
Li P, Guo YJ, Tang Q, Yang L. Effectiveness of nursing intervention for increasing hope in patients with cancer: A meta-analysis. Rev Lat Am Enfermagem. 2018;26. e2937. [PubMed ID: 30110091]. [PubMed Central ID: PMC6091366]. https://doi.org/10.1590/1518-8345.1920.2937.
-
58.
Pourfaraj M, Rezazadeh H. [Effectiveness of positive therapy on happiness and hope in cancer patients]. Counseling Culture and Psycotherapy. 2018;9(33):119-36. Persian.
-
59.
Fischer IC, Cripe LD, Rand KL. Predicting symptoms of anxiety and depression in patients living with advanced cancer: the differential roles of hope and optimism. Support Care Cancer. 2018;26(10):3471-7. [PubMed ID: 29681016]. https://doi.org/10.1007/s00520-018-4215-0.
-
60.
Ozen B, Ceyhan O, Buyukcelik A. Hope and perspective on death in patients with cancer. Death Stud. 2020;44(7):412-8. [PubMed ID: 31204898]. https://doi.org/10.1080/07481187.2019.1626942.
-
61.
Bastian TD, Burhansstipanov L. Sharing wisdom, sharing hope: Strategies used by native American cancer survivors to restore quality of life. JCO Glob Oncol. 2020;6:161-6. [PubMed ID: 32031445]. [PubMed Central ID: PMC6998019]. https://doi.org/10.1200/JGO.19.00215.
-
62.
Snyder CR. Handbook of hope: Theory, measures, and applications. Massachusetts, USA: Academic press; 2000.
-
63.
Myers RE. Decision counseling in cancer prevention and control. Health Psychol. 2005;24(4S):S71-7. [PubMed ID: 16045422]. https://doi.org/10.1037/0278-6133.24.4.S71.
-
64.
Feldman DB, Snyder CR. Hope and the meaningful life: Theoretical and empirical associations between goal–directed thinking and life meaning. J Soc Clin Psychol. 2005;24(3):401-21. https://doi.org/10.1521/jscp.24.3.401.65616.
-
65.
Reinke LF, Shannon SE, Engelberg RA, Young JP, Curtis JR. Supporting hope and prognostic information: Nurses' perspectives on their role when patients have life-limiting prognoses. J Pain Symptom Manage. 2010;39(6):982-92. [PubMed ID: 20538182]. [PubMed Central ID: PMC2884140]. https://doi.org/10.1016/j.jpainsymman.2009.11.315.
-
66.
Glajchen M. The emerging role and needs of family caregivers in cancer care. J Support Oncol. 2004;2(2):145-55. [PubMed ID: 15328817].
-
67.
Klemm P, Wheeler E. Cancer caregivers online: Hope, emotional roller coaster, and physical/emotional/psychological responses. Comput Inform Nurs. 2005;23(1):38-45. [PubMed ID: 15681993]. https://doi.org/10.1097/00024665-200501000-00008.
-
68.
Azizi M, Elyasi F. Effective strategies for increasing the hope in patients with cancer: A review. J Cell Immunother. 2017;3(1):14-5. https://doi.org/10.1016/j.jocit.2017.04.021.
-
69.
Baljani E, Khashabi J, Amanpour E, Azimi N. [Relationship between spiritual well-being, religion, and hope among patients with cancer]. Hayat. 2011;17(3):27-37. Persian.
-
70.
Herth K. Fostering hope in terminally-ill people. J Adv Nurs. 1990;15(11):1250-9. [PubMed ID: 2269747]. https://doi.org/10.1111/j.1365-2648.1990.tb01740.x.
-
71.
Aghajani MJ, Akbari B, Khalatbari J, Sadighi A. [Effectiveness of group logo therapy on feeling loneliness and psychological hardiness of the girls suffering from love trauma syndrome]. Armaghane Danesh. 2018;23(5):559-76. Persian.
-
72.
Nader M, Ghanbari N, Tajabadi pour S, Gholipour S, Esmaeilzadeh N. Effectiveness of short-term group logo-therapy on life expectancy and resilience of women with breast cancer. Arch Breast Cancer Res. 2019;6(4):168-73. https://doi.org/10.32768/abc.201964168-173.
-
73.
Stefanek M, McDonald PG, Hess SA. Religion, spirituality and cancer: Current status and methodological challenges. Psychooncology. 2005;14(6):450-63. [PubMed ID: 15376283]. https://doi.org/10.1002/pon.861.
-
74.
Boucher JE. Telephone intervention: Hope for cancer patients [dissertation]. Massachusetts, USA: University of Massachusetts Amherst; 2003.