Abstract
Background:
The Body Image Acceptance and Action Questionnaire (BI-AAQ) assesses cognitive flexibility and acceptance of body image.Objectives:
This study was done to assess the validity and reliability of the Persian version of BI-AAQ, as an instrument to measure body image flexibility, in patients with somatic symptom and related disorders.Methods:
This descriptive psychometric study was done in 2017 on 357 patients with somatic symptom and related disorders selected through a convenient sampling method from Kashan University of Medical Sciences clinics. They responded to the BI-AAQ, Depression, Anxiety, and Stress Scale (DASS), Acceptance and Action Questionnaire-II (AAQ-II), and Freiburg Mindfulness Inventory (FMI). The reliability of the BI-AAQ was calculated using Cronbach’s alpha coefficient. To assess its validity, the exploratory and confirmatory factor analyses were used. The gathered data were analyzed via SPSS-22 and Amos-22 software.Results:
This version retained a one-factor structure, similar to the original version of the questionnaire, which explained 42.55% of the variance. It had high internal consistency (0.84), split-half method (0.77), and correlates with AAQ (0.45), mindfulness (0.39) and correlates contrastingly with stress (0.11), anxiety (0.36) and depression (0.43).Conclusions:
According to the results of the current research, the BI-AAQ is a reliable instrument with valid psychometric properties to measure the body image acceptance of individuals in Iranian patients with somatic symptom and related disorders.Keywords
Acceptance Body Image Acceptance and Action Questionnaire Psychometric Properties Somatic Symptom and Related Disorders
1. Background
Body image can be defined as a person’s people’s perception of their physical self (1). It has three aspects: (1) the perceptual aspect, which refers to the person’s perception of his physical appearance and includes an evaluation of the weight, size, and shape; (2) the subjective (cognitive and affective) aspect, which includes aspects, such as satisfaction or concern about appearance; and (3) the behavioral aspect (the avoidance of conditions that result in exposure and eventually cause anxiety and distress) (2). Various studies have investigated the association between body image and social functions, revealing the relationship between this factor and these functions, and life quality (2). Research results have also implied that the perceptual difference between physical appearance and ideal body image causes significant distress. It can also result in radical, destructive behavior, such as inordinate dieting, physical problems, or repeated manipulation of the appearance (1).
Cognitive-behavioral therapy (CBT) stresses the distorted and irrational body image analyses and suggests correcting them through cognitive restructuring. It is also argued that negative affections result from these analyses. On the other hand, newer and more detailed views on body image have been articulated with the birth of the third generation of behavioral therapies and evolution of the acceptance and commitment therapy (ACT) model (3).
ACT is an example of the third generation of behavioral therapies, and it explicitly advocates the alteration of the functions of thoughts and emotions instead of changing their forms, contents, or frequencies (3). ACT, which is based on the relational framework theory, has its roots in the functional contextualism philosophy. It consists of six core processes leading to psychological flexibility. These six processes are acceptance, defusion, self as context, contact with the present moment, values, and committed action (3). In this model, experiential avoidance is a construct with a significant role in psychopathology and serves to avoid painful experiences.
Many patients with somatic symptom and related disorders display high levels of experiential avoidance. These individuals often describe their inner experiences (including thoughts, affects, bodily sensations, impulses, and memories) as intolerable events and take actions to avoid or reduce the intensity of these experiences (3).
In the ACT, experiential avoidance is considered as an important destructive factor. Modifying this factor can bring peace to the person by reducing the distressing factors. However, it can result in behavioral decline and reduced awareness through negative reinforcement (4). In this method, body image disturbance is associated with cognitive flexibility, and the strict behavioral and cognitive patterns are considered problems. On the other hand, experiential avoidance is accepted by embracing and facing somatic feelings and senses (4). The goal of ACT is to create flexibility to move along the path of values.
The Acceptance and Action Questionnaire-II (AAQ-II) was developed to assess psychological flexibility, and it has been widely used in various studies (5). However, this questionnaire is not extensively used in studies on somatic symptom and related disorders. Sandoz et al. developed a modified version of this questionnaire called BI-AAQ (5).
This questionnaire assesses the avoided negative affections or thoughts about one’s body, which interfere with the person’s life and values. It was originally developed and normalized for a group of nonclinical university students. Sandoz studied a 12-item scale on 182 participants and eventually reported that one item was loaded higher than 0.60 (6). This scale has displayed an extremely good internal consistency (0.92) and has satisfactory convergent validity in predicting the eating disorders. It has been translated into various languages and has been especially applied in assessing somatic disorders (7). The different translations of this scale have displayed high levels of reliability and validity (8). In a study on women with eating disorders, low scores of the BI-AAQ were significantly associated with symptoms of this disorder in the pre- and post-treatment phases (9).
2. Objectives
The main objective of the present research was to examine the validity and reliability of a Persian version of the BI-AAQ in a clinical population suffering at least one of the somatic symptom and related disorders.
3. Methods
3.1. Population and Participants
The study population included all the patients who visited one of the clinics of Kashan University of Medical Sciences and were diagnosed with one of the somatic symptoms and related disorders by a psychiatrist or an internist, according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). Polit and Beck (10) and Garson (11) recommended 5 to 10 patients per item for the exploratory factor analysis (EFA). Garson (11) recommended sample size of 200 people for the confirmatory factor analysis (CFA). Therefore, considering the number of the items (12 items) and the likelihood of attrition, 150 patients with somatic symptoms and related disorders were selected for the EFA and 220 patients for the CFA. As a result, 370 participants were selected, and finally, 357 participants (144 cases of the first step and 213 patients of the second step) completed the questionnaires (illness anxiety disorder = 33, somatic symptom disorder = 72, psychological factors affecting other medical conditions = 232, and conversion disorder = 20) and were included in the analyses in the first and second studies.
3.2. Procedure
3.2.1. Step 1
To use this scale in this research, it was translated into Persian with the permission of the authors, and three expert psychologists were consulted about the accuracy of the translation. Afterward, two translators were provided with the approved version (a psychologist with a mastery of the Persian and English languages and an English expert familiar with psychological texts, who had not seen the original version, to translate it into English (back translation)). Then, the latter was compared with the original scale, and the discrepancies were resolved.
3.2.2. Step 2
The translated form was tested on ten patients with somatic symptom and related disorders to ensure an accurate understanding of the items.
3.2.3. Step 3
Afterward, a briefing session was held to discuss the diagnosis and diversity of the somatic symptom and related disorders after obtaining a permit from the university and making arrangements with some physicians, psychologists, and psychiatrists. In this session, three masters of clinical psychology were introduced, and arrangements were made to complete the questionnaires. These masters met with the specialists to complete the questionnaires, and all of the patients were interviewed.
3.2.4. Step 4
Participants were divided into two groups. The first group was used for EFA, and the other group was used for CFA. The normality of data was examined by the Shapiro-Wilk test. EFA was conducted using the Kaiser-Meyer-Olkin (KMO) and the Bartlett tests. Then, CFA was used to confirm the exploration model. To calculate the reliability of this scale, Cronbach’s alpha and split-half method were used. The results were analyzed with SPSS version 22.0 and AMOS-22 software.
3.3. Measures
3.3.1. Body Image-Acceptance and Action Questionnaire (BI-AAQ)
This questionnaire was developed to assess the body image flexibility (6). It is defined as the potential for experiencing perceptions, physical feelings, affections, thoughts, and beliefs about one’s body image without attempting to change their intensity and frequencies while pursuing one’s values despite such beliefs (6). The final version of this scale consists of 12 items ranked from 1 to 7 based on the Likert scale. The minimum and maximum scores are 12 and 84, respectively (12). The reliability and validity of the BI-AAQ were reported acceptable after testing it on a sample of university students in Iran (13).
3.3.2. Depression, Anxiety, and Stress Scale (DASS)
DASS was developed in 1995 by Lovibond and Lovibond (14). This scale is available in two versions. The short-form version consists of 21 items that assess the depression, anxiety, and stress constructs by 7 different statements. The long-form is composed of 42 items and 14 statements to assess psychological health. The validity of its short-form was assessed in Iran by Darchini-Maragheh et al. Internal consistency was reported 0.77, 0.79, and 0.78 for depression, anxiety, and stress, respectively (15).
3.3.3. Acceptance and Action Questionnaire II (AAQ-II)
This questionnaire measures psychological flexibility, especially in terms of experiential avoidance and the tendency to engage in actions despite unwanted thoughts and effects (5). It consists of 7 items ranked based on the Likert scale. The reliability of this scale was reported 0.81 by Bond et al., and its internal consistency was reported 0.84 (5). Izadi et al. also reported an internal consistency (α = 0.86) and test-retest reliability (r = 0.72) for this scale (13).
3.3.4. The Freiburg Mindfulness Inventory (FMI)
FMI is a short form with 14 items, which measures several important aspects of mindfulness (7, 16, 17). Each item is scored on a four-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). This inventory was standardized by Ghasemi Jobaneh et al. in Iran, and its validity and reliability have been confirmed. They reported an internal consistency (α = 0.92) and test-retest reliability (r = 0.83) for this scale (18).
Psychiatric interviews were done using DSM-5 criteria to diagnose somatic symptom and related disorders (19).
4. Results
4.1. Descriptive Analysis
Table 1 presents the demographic information of the study patients (n = 357; 210 female and 147 male) with somatic symptom and related disorders in Kashan city. The average age of the samples was 23.39 ± 6.7 years, and most of the participants had a Bachelor’s degree (Table 1).
The Demographic Information of the Study Samples
| Sample | Gender, Frequency (%) | Education | Age, Mean ± SD | |||
|---|---|---|---|---|---|---|
| Female | Male | High School Diploma or Lower | Bachelor’s Degree | Master’s Degree and Ph.D. | ||
| Exploratory factor analysis | 88 (61.1) | 56 (38.9) | 21 (14.6) | 100 (69.4) | 23 (16) | 24.59 ± 6.16 |
| Confirmatory factor analysis | 122 (57.3) | 91 (42.7) | 18 (8.5) | 168 (78.9) | 27 (12.7) | 23.63 ± 5.93 |
| Total | 210 (58.8) | 147 (41.2) | 39 (10.9) | 268 (57.1) | 50 (24) | 23.39 ± 6.7 |
Table 2 shows the mean and SD of BI-AAQ, DASS, FMI, AAQ in two groups, and total participants. Also, the mean and SD of BI-AAQ according to diagnosis in two groups and total participants has been reported in Table 3.
The Mean and Standard Deviation of the BI-AAQ, DASS, FMI, AAQ
| Sample | BI-AAQ, Mean ± SD | DASS, Mean ± SD | FMI, Mean ± SD | AAQ, Mean ± SD | ||
|---|---|---|---|---|---|---|
| Depression | Anxiety | Stress | ||||
| Exploratory factor analysis | 35.92 ± 14.51 | 13.67 ± 3.75 | 13.66 ± 3.75 | 16.31 ± 4.18 | 86.01 ± 15.45 | 24.59 ± 6.16 |
| Confirmatory factor analysis | 38.2 ± 13.72 | 14.58 ± 4.73 | 13.94 ± 4.04 | 16.35 ± 4.32 | 82.32 ± 14.78 | 23.63 ± 5.93 |
| Total | 37.28 ± 4.26 | 14.21 ± 4.58 | 13.83 ± 3.92 | 16.33 ± 4.26 | 83.8 ± 15.14 | 37.9 ± 9.08 |
The Mean and Standard Deviation of the BI-AAQ According to Diagnosis
| Group/Diagnosis | N | Mean | SD |
|---|---|---|---|
| Exploratory factor analysis | |||
| Somatic symptom disorder | 55 | 33.96 | 14.84 |
| Illness anxiety | 12 | 35.08 | 13.39 |
| Conversion disorder | 8 | 34.62 | 11.73 |
| Psychological factors affecting | 16 | 36.75 | 16.15 |
| Factitious disorder | 6 | 34.83 | 16.94 |
| Other unspecified somatic symptom disorders | 47 | 38.54 | 14.42 |
| Total | 144 | 35.91 | 14.56 |
| Confirmatory factor analysis | |||
| Somatic symptom disorder | 68 | 36.16 | 13.28 |
| Illness anxiety | 85 | 38.34 | 13.71 |
| Conversion disorder | 5 | 43.40 | 11.05 |
| Psychological factors affecting | 4 | 47.00 | 11.34 |
| Factitious disorder | 6 | 46.16 | 13.60 |
| Other unspecified Somatic symptom disorders | 45 | 38.60 | 11.66 |
| Total | 213 | 38.20 | 13.13 |
| Total | |||
| Somatic symptom disorder | 123 | 35.17 | 13.99 |
| Illness anxiety | 97 | 37.93 | 13.65 |
| Conversion disorder | 13 | 38.0 | 11.86 |
| Psychological factors affecting | 20 | 38.0 | 15.62 |
| Factitious disorder | 12 | 40.50 | 15.79 |
| Other unspecified somatic symptom disorders | 92 | 38.57 | 13.05 |
| Total | 356 | 37.28 | 13.74 |
4.2. Construct Validity
4.2.1. Exploratory Factor Analysis
In the exploratory and confirmatory factor analyses, there was no significant difference between the two samples in terms of age (t = 1.46, P = 0.14), gender (χ2 = 0.52, P = 0.47), and education (χ2 = 4.68, P = 0.32). There was also no difference between the scores of BI-AAQ (t = 1.21, P = 0.22) of the two groups. First, an EFA was carried out to assess the construct validity of this scale. To this end, the correlation between the items was assessed, revealing a correlation higher than 0.3 between some of the items and satisfaction of the requirement for the factor analysis. In the EFA, the numerical KMO was 0.87, and the χ2 resulting from the Bartlett test was 649.45, which was significant at P < 0.001, showing the adequacy of the selected sample and variables for the analysis. One factor with an eigenvalue of 4.75 was extracted by performing a factor analysis of the principal components with varimax rotation using eigenvalues and a scree slope. The factor explained 42.55% of the total variance (Table 4).
The Factor Loading of BI-AAQ Items
| Item | Factor Loading |
|---|---|
| 1. Worrying about my weight makes it difficult for me to live a life that I value. | 0.59 |
| 2. I care too much about my weight and body shape. | 0.39 |
| 3. I shut down when I feel bad about my body shape or weight. | 0.58 |
| 4. My thoughts and feelings about my body weight and shape must change before I can take important steps in my life. | 0.60 |
| 5. Worrying about my body takes up too much of my time. | 0.66 |
| 6. If I start to feel fat, I try to think about something else. | 0.45 |
| 7. Before I can make any serious plans, I have to feel better about my body. | 0.54 |
| 8. I will have better control over my life if I can control my negative thoughts about my body. | 0.44 |
| 9. To control my life, I need to control my weight. | 0.75 |
| 10. Feeling fat causes problems in my life. | 0.61 |
| 11. When I start thinking about the size and shape of my body, it’s hard to do anything else. | 0.66 |
| 12. My relationships would be better if my body weight and/or shape did not bother me. | 0.58 |
| Eigenvalue | 4.75 |
| % Variance | 42.55 |
4.2.2. Confirmatory Factor Analysis
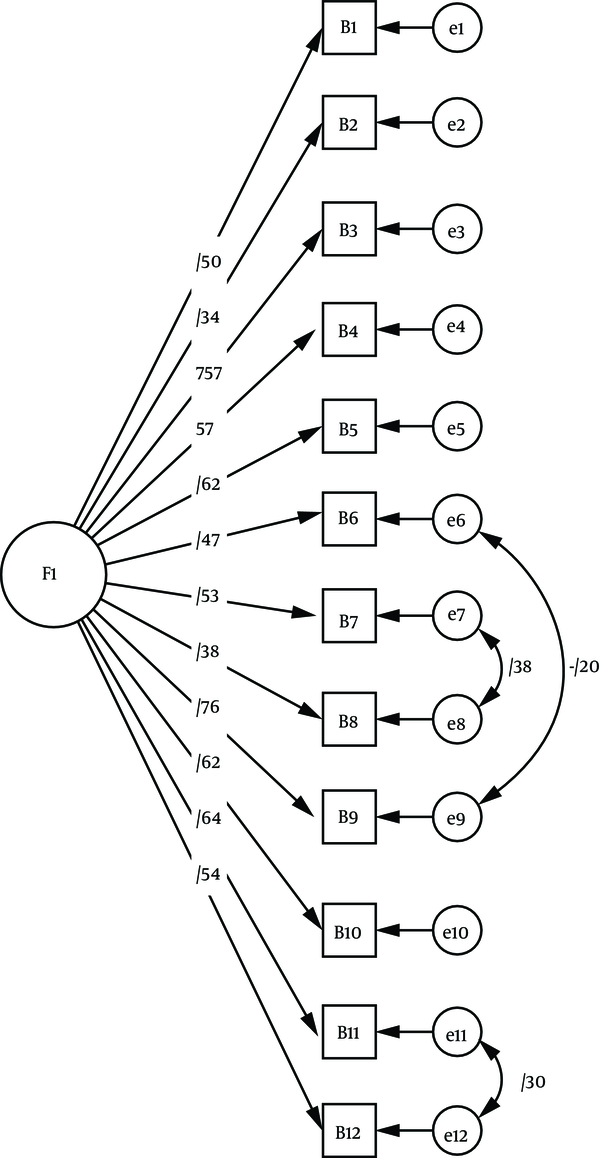
AMOS-22 was used to evaluate the one-factor model of this scale in the CFA. The results indicated that all of the goodness of fit index, adjusted goodness of fit index, comparative fit index, Tucker-Lewis index (larger than 0.90), and root mean square error of approximation (smaller than 0.05) indices were in the acceptable range (Table 5). Consequently, it could be stated that the one-factor model extracted from the EFA had a good fit (Figure 1). Figure 1 shows the results of the structural equation modeling analysis of the one-factor model BI-AAQ with standard coefficients.
Results of the Confirmatory Factor Analysis of the One-Factor Model of BI-AAQ
| Goodness of Fit Indexes Model | χ2/Df | GFI | AGFI | TLI | CFI | RMSEA (90% CI) |
|---|---|---|---|---|---|---|
| One-factor model | 1.44 | 0.96 | 0.93 | 0.96 | 0.97 | 0.039 (0.01 - 0.05) |
Results of the structural equation modeling analysis of one-factor model BI-AAQ
4.3. Convergent and Divergent Validity
To assess the convergent validity of this scale, the Pearson’s correlation between this scale and the total score of AAQ and FMI was calculated, and for divergent validity, the correlation between this scale and DASS-21 was determined. The correlation between the total score of the BI-AAQ and AAQ, and FMI was 0.39 and 0.39, respectively (P < 0.001). This confirms the convergent validity of this scale. On the other hand, the divergent validity of this scale was calculated by assessing its correlation with the stress (-0.11), anxiety (-0.36), and depression (-0.43) Subscales.
4.4. Reliability
Analysis of the reliability of this scale resulted in a Cronbach’s alpha coefficient of 0.84, and a reliability coefficient of r = 0.77 was calculated using the split-half method (P < 0.001).
5. Discussion
Due to the lack of a scale for assessing body image flexibility in patients with somatic symptom and related disorders in Iran, this research was carried out, and psychometric properties of the BI-AAQ were studied (14). This scale was developed to assess the ability to accept and experience perceptions, thoughts, beliefs, and physical feelings without attempting to change their intensity, frequencies, or forms. Hence, the relationships among stress, anxiety, depression, psychological flexibility, and body image flexibility were studied, and their convergent and divergent validities were assessed. Also, the relationship between each item and body image flexibility was taken into account based on the model developed by Sandoz et al. (6) as regards the one-factor model of body image flexibility, and the model was fitted. In sum, the values of the indices matched their interpretive values, reflecting the adequacy and satisfactory validity of the scale. The factorial analysis showed a one-dimensional factor structure, similar to the original one (6). Therefore, the results confirmed the validity and reliability of this scale.
The method used by the authors of this scale was employed in the psychometric analysis of BI-AAQ. As stated, the 12-item one-factor structure referred to the theoretical description of this scale was observed, which explained 42.55% of its total variance. Our results comply with the results reported by the authors of this scale (6, 7, 14, 16), who proved the existence of one main factor in the scale.
Also, the reliability of this scale was assessed using Cronbach’s alpha internal consistency and split-half methods. The results of the internal consistency method revealed the relatively high reliability of this scale (0.84) in patients with somatic symptom and related disorders. Its reliability using the split-half method was r = 0.77. These results comply with the findings reported in a study on Iranian university students (13) and the research by Sandoz et al. (6) and Ferreira et al. (7), who reported Cronbach’s alpha coefficients of 0.92 and 0.95, respectively. In general, the results of this research indicated that the 12-item version of the BI-AAQ had satisfactory reliability in the Iranian population and can be used confidently for patients with somatic symptom and related disorders.
The divergent and convergent validities were employed to assess the validity of this scale. In the convergent validity phase, this scale showed a significant correlation with the total score of AAQ-II (5) and the FMI (17).
From a pathological point of view, the correlation with AAQ-II, which shows psychological flexibility, indicates the level of psychological flexibility and a lack of experiential avoidance. This finding is in line with the findings reported by Izadi et al. (16), Sandoz et al. (6), and Ferreira et al. (7). Our findings also suggested that body image flexibility is associated with body satisfaction, self-care, self-compassion (18), and philanthropy (20, 21). Therefore, it can be concluded that acceptance of body image has a positive relationship with the other mental health dimensions (7).
Moreover, the DASS-21 scale was used to assess the divergent validity of this scale, and the results showed the negative relationship between the total score of the BI-AAQ and anxiety and depression. In other words, with an increase in body image flexibility, anxiety, and depression decrease. Similar findings were reported by other researchers (12). Also, this scale has a negative relationship with other general dimensions of psychopathology.
These findings can be added to those from the Steven Hayes’ model of ACT, in which he reports the negative association between psychological symptoms and acceptance, and the latter’s relationship with life quality and general health dimensions (22). Therefore, BI-AAQ can be used as a predictor of mental health and psychopathology.
Since the prevalence of somatic symptom and related disorders is relatively considerable, and these disorders account for a large portion of the referrals to clinical psychologists (23), it is necessary to accurately examine its psychological dimensions. This examination calls for various scales that can be used to diagnose and treat such disorders. Somatic symptom and related disorders can affect a wide range of people and the patients suffer several somatic symptoms (23). Numerous studies have examined body image flexibility and proved this construct’s effectiveness in assessing disorders associated with the body (7, 12). BI-AAQ can also be applicable in identifying high-risk individuals and preventing somatic symptom and related disorders (6). We found that it is possible to use the Persian version of this scale for patients suffering from somatic symptom and related disorders.
This study had several limitations. Firstly, the scale studied in this research has been examined for all somatic symptom disorders. Therefore, it should be used in a more limited and specialized group. Although the sample size was large, this questionnaire was surveyed only in one city of Iran. However, it can be stated that the BI-AAQ, which was designed based on the theoretical model of ACT, is a transdiagnostic scale and can be used for different disorders. Hence, it is recommended to use this scale in the preliminary examinations and assessment of the treatment process. It enables the therapists to estimate body acceptance, body image flexibility, body awareness, mindfulness, and psychological distress to a great extent.
5.1. Conclusion
The analysis of the psychometric properties of BI-AAQ showed good values. Accordingly, this scale is an appropriate tool to measure the rate of the acceptance of body image in Iranian people with somatic symptom and related disorders.
Acknowledgements
References
-
1.
Thompson J. Assessing body image disturbance: Measures, methodology, and implementation. Body image, eating disorders, and obesity: An integrative guide for assessment and treatment. 2001. p. 49-81. https://doi.org/10.1037/10502-003.
-
2.
Tantleff-Dunn S, Lindner DM. Body image and social functioning. In: Cash TF, Smolak L, editors. Body image: A handbook of science, practice, and prevention. 2nd ed. New York: Guilford Press; 2011. p. 263-70.
-
3.
Hayes SC, Barnes-Holmes D, Wilson KG. Contextual Behavioral Science: Creating a science more adequate to the challenge of the human condition. Journal of Contextual Behavioral Science. 2012;1(1-2):1-16. https://doi.org/10.1016/j.jcbs.2012.09.004.
-
4.
Hayes SC, Pistorello J, Levin ME. Acceptance and Commitment Therapy as a Unified Model of Behavior Change. The Counseling Psychologist. 2012;40(7):976-1002. https://doi.org/10.1177/0011000012460836.
-
5.
Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011;42(4):676-88. [PubMed ID: 22035996]. https://doi.org/10.1016/j.beth.2011.03.007.
-
6.
Sandoz EK, Wilson KG, Merwin RM, Kate Kellum K. Assessment of body image flexibility: The Body Image-Acceptance and Action Questionnaire. Journal of Contextual Behavioral Science. 2013;2(1-2):39-48. https://doi.org/10.1016/j.jcbs.2013.03.002.
-
7.
Ferreira C, Pinto-Gouveia J, Duarte C. The validation of the Body Image Acceptance and Action Questionnaire: Exploring the moderator effect of acceptance on disordered eating. International Journal of Psychology and Psychological Therapy. 2011;11(3):327.
-
8.
Moore M, Masuda A, Hill ML, Goodnight BL. Body image flexibility moderates the association between disordered eating cognition and disordered eating behavior in a non-clinical sample of women: a cross-sectional investigation. Eat Behav. 2014;15(4):664-9. [PubMed ID: 25289446]. https://doi.org/10.1016/j.eatbeh.2014.08.021.
-
9.
Wendell JW, Masuda A, Le JK. The role of body image flexibility in the relationship between disordered eating cognitions and disordered eating symptoms among non-clinical college students. Eat Behav. 2012;13(3):240-5. [PubMed ID: 22664403]. https://doi.org/10.1016/j.eatbeh.2012.03.006.
-
10.
Polit DF, Beck CT. Nursing research: Principles and methods. Lippincott Williams & Wilkins; 2004.
-
11.
Garson GD. Testing of assumptions. Online monograph; 2007. Available from: http://www.Chass.ncsu.edu/garson/pa 765/assumpt.htm.
-
12.
Basarkod G, Sahdra B, Ciarrochi J. Body Image-Acceptance and Action Questionnaire-5: An Abbreviation Using Genetic Algorithms. Behav Ther. 2018;49(3):388-402. [PubMed ID: 29704968]. https://doi.org/10.1016/j.beth.2017.09.006.
-
13.
Izaadi A, Karimi J, Rahmani M. Psychometric Analysis of Persian Version of Body Image flexibility Questionnaire (BI-AAQ) among University students. Hayat. 2013;19(3).
-
14.
Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335-43. https://doi.org/10.1016/0005-7967(94)00075-u.
-
15.
Darchini-Maragheh E, Salehi M, Payandeh A, Behdani F, Ghasemzadeh Kolagar H. Evaluation of the correlations between depression, anxiety, and stress as DASS-21 subscales and high-risk behaviors in the adolescents in Torghabeh and Shandiz Towns, Iran. Journal of Patient Safety & Quality Improvement. 2017;5(3):584-90.
-
16.
Walach H, Buchheld N, Buttenmüller V, Kleinknecht N, Schmidt S. Measuring mindfulness—the Freiburg Mindfulness Inventory (FMI). Personality and Individual Differences. 2006;40(8):1543-55. https://doi.org/10.1016/j.paid.2005.11.025.
-
17.
Neff KD. The Development and Validation of a Scale to Measure Self-Compassion. Self and Identity. 2003;2(3):223-50. https://doi.org/10.1080/15298860309027.
-
18.
Ghasemi Jobaneh R, Arab Zadeh M, Jalili Nikoo S, Mohammad Alipoor Z, Mohsenzadeh F. Survey the validity and reliability of the persian version of short form of freiburg mindfulness inventory. Journal of Rafsanjan University of Medical Sciences. 2015;14(2):137-50.
-
19.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub; 2013. https://doi.org/10.1176/appi.books.9780890425596.
-
20.
Webb JB. Body image flexibility contributes to explaining the link between body dissatisfaction and body appreciation in White college-bound females. Journal of Contextual Behavioral Science. 2015;4(3):176-83. https://doi.org/10.1016/j.jcbs.2015.06.001.
-
21.
Bluett EJ, Lee EB, Simone M, Lockhart G, Twohig MP, Lensegrav-Benson T, et al. The role of body image psychological flexibility on the treatment of eating disorders in a residential facility. Eat Behav. 2016;23:150-5. [PubMed ID: 27776279]. https://doi.org/10.1016/j.eatbeh.2016.10.002.
-
22.
Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1-25. [PubMed ID: 16300724]. https://doi.org/10.1016/j.brat.2005.06.006.
-
23.
Shabbeh Z, Feizi A, Afshar H, Hassanzade Kashtali A, Adibi P. Identifying the profiles of somatic symptom and related disorders in an iranian adult population and their relation to psychological problems. Journal of Mazandaran University of Medical Sciences. 2016;26(137):82-94.