Abstract
Objectives:
The study objective was to determine the way in which patients encounter pain, and to distinguish the clinical parameters impacting pain by transrectal ultrasonography (TRU) of the prostate.Patients and Methods:
Medical records for men receiving prostate TRU from November 2015 to April 2016 were acquired from the database. Patients underwent a detail review of medical history as well as physical evaluation. All the relevant variables were associated to visual analog scale (VAS) by using multivariate regression analysis.Results:
Independent factors for TRU associated pain were identified using multivariate regression analysis. The analysis demonstrated that sagittal length of the prostate was the continuous variable impacting pain level. Patients who received explanation for the process of the test in detail promptly before the examination and had prior TRU experience were found to be in negative association with the pain score; while, hemorrhoids (external), prior anal surgery, and stool artifact were in positive association with the pain score.Conclusion:
Despite the fact that TRU of the prostate is uncomfortable for patients, after identification of pain affecting factors, healthcare providers could help reduce the patients’ pain through the procedure, thereby providing better quality exams.Keywords
Prostate Trans Rectal Ultrasonography Ultrasound Visual Analog Scale
1. Background
The initial clinically relevant prostate pictures provided through trans rectal ultrasonography (TRU) were depicted by Watanabe et al. in 1967 (1). As the technology of ultrasound has turned out to be greatly refined throughout the years, utilization of TRU to assess prostatic illness has expanded. In the mid-80s, the 7 MHz ultrasound test, that plainly portrays the prostate design, turned into a standard instrument for diagnosis (2). TRU could be utilized for detection of prostate anomalies including prostate cancer, prostatitis, benign prostatic hyperplasia (BPH), and prostatic calculi (3). Nevertheless, TRU of the prostate is painful (4), and there were claims from a few patients at our setting that they encountered extreme pain while getting this intrusive technique. Despite the fact that the level of and variables affecting pain amid TRU-guided biopsy were explored in the literature (5-7), in view of our investigation, there is a dearth of studies that concentrated on pain encountered by the patients undergoing TRU of the prostate.
2. Objectives
The objectives of the present study were to determine the way in which patients encounter the pain, and to distinguish the clinical parameters impacting the pain amid a TRU test.
3. Patients and Methods
This single center prospective study was performed in tertiary hospital, China from November 2015 to April 2016.
The study got the approval from the ethics committee and patient confidentiality was strictly maintained. Medical records for men receiving prostate TRU from November 2015 to April 2016 were acquired from the database. Patients underwent a detail review of medical history as well as physical evaluation. The recorded variables were age, prostate specific antigen level, [body mass index (BMI) obtained by dividing weight in kilograms by square of height in meters], prior anal operative history, and TRU experience. At the point when routine computerized rectal examination was done, careful inspection of the anus and any appearance of external hemorrhoids was noted. Exclusion criteria included patients having dementia, disorders that interfere with the verbal communication, prostatitis, neurological disorders that have potential impact assessment of pain, as well as those who encountered transurethral prostate resection. An aggregate of 468 patients were enlisted in the present study.
The patients were categorized into two groups via randomization as per medical-chart number (Group 1 [odd number]; Group 2 [even number]). The patients in Group 1 got the TRU test as the standard procedure of the setting. In contradiction, Group 2 patients got the test process explanation in detail promptly prior to the examination start. Additionally, a monitor was put alongside them, letting the patients watch the ongoing pictures amid the whole test. TRU was conducted on patients utilizing an ultrasound machine (Prosound Alpha 6 [Hitachi, Tokyo]) with a 7.5MHz biplane trans rectal probe. The volume of the prostate was calculated utilizing ellipse formula (sagittal length × height × width × 0.52). Interference of picture quality with that of stool storage in the rectum was noted. Quickly taking after the test, the patients finished a visual analog scale (VAS) survey, assessing the pain encountered amid the TRU on a 0 to 10 scale. Rounding technique was utilized to get a whole number.
The distribution was inspected utilizing the Kolmogorov Smirnov test. comparison of continuous as well as categorical variables was performed by Mann-Whitney U-test or Chi square tests. Linear regression was conducted for analysis and identification of independent variables impacting the pain was encountered amid the test. Analysis of all collected data was done using SPSS version 16.0 (Chicago, SPSS Inc). P value ≤ 0.05 was regarded as statistically significant.
4. Results
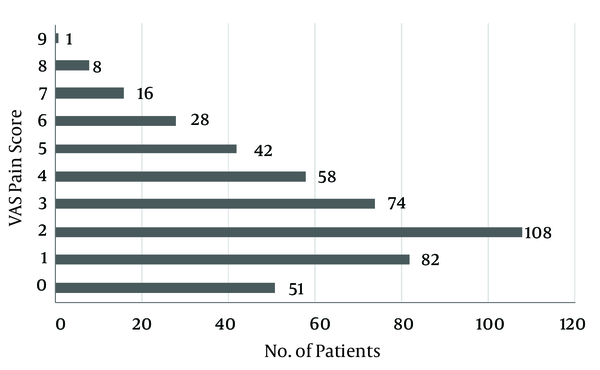
The clinical/demographic characteristics of patients are outlined in Table 1. The patients’ median age (years), body mass index (kg/m2), and prostate volume (mL), were 62 (range: 42 - 86), 24.62 (17.1 - 46.98), and 33.1 (9.8 - 161.04), respectively. The mean pain score was noted as 2.79 (standard deviation: 2.14; range of 0 - 9). The visual analog scale pain score distribution is depicted in Figure 1. No pain (pain score [VAS] = 0) was recorded in 51 (10.9%) patients, mild pain (pain score = 1 to 3) was recorded in 264 (56.41%) patients, whereas moderate pain (pain score = 4 to 5) was recorded in 100 (21.37%) patients. Fifty-three patients (11.32%) experienced severe pain (pain score = 6 to 10) amid test. The Kolmogorov Smirnov test demonstrated normality in result distribution.
| Characteristics (N = 468) | Median (Range) | Pain Score < 4 | Pain Score > 3 | P Value |
|---|---|---|---|---|
| Age (years) | 62 (42 - 86) | 64.88 ± 10.86 | 63.22 ± 11.86 | 0.0182 |
| Body mass index (kg/m2) | 24.62 (17.1 - 46.98) | 24.84 ± 3.92 | 25.14 ± 3.82 | 0.5362 |
| Prostate volume (mL) | 33.1 (9.8 - 161.04) | 36.91 ± 21.29 | 42.92 ± 25.39 | 0.0372 |
| Prostate specific antigen (ng/mL) | 4.98 (0.1 - 397.8) | 3.18 ± 2.21 | 4.78 ± 3.94 | 0.4042 |
| Prostate sagittal length (cm) | 4.48 (2.39 - 7.48) | 4.74 ± 0.82 | 4.62 ± 0.92 | 0.0322 |
Visual analog scale - pain score distribution
At the point when patients were divided further into two categories: pain score < 4 and pain score > 3, as depicted in Table 1, it was observed that patients with pain scores > 3 were significantly younger in age (63.22 versus 64.88, P = 0.0182), and they had a significantly bigger prostate volume (42.92 g versus 36.91 g, P = 0.0372), and a significantly large prostate sagittal length (4.74 cm vs 4.48 cm, P = 0.0322). The information additionally uncovered that a lower rate of patients with pain scores > 3 had prior TRU experience (14.38% versus 24.13%, P = 0.0482) and they were categorized randomly into Group 2 (35.29% versus 59.05%, P < 0.0001) in comparison to patients with pain scores < 4. In contradiction, a high percentage of patients with pain scores > 3 experienced hemorrhoids (external) (58.82% versus 27.30%, P < 0.0001), prior anal surgery (32.03% versus 7.30%, P < 0.0001), and stool artifact (21.57% versus 10.79%, P = 0.0032), as depicted in Table 2.
Qualitative Variable Comparison
| Characteristics (N = 468) | Pain Score < 4 (%) | Pain Score > 3 (%) | P Value |
|---|---|---|---|
| Prior TRU experience | 24.13 | 14.38 | 0.0482 |
| Group 2 | 59.05 | 35.29 | < 0.0001 |
| Prostate calcification | 23.49 | 37.25 | 0.0822 |
| Hemorrhoids (external) | 27.30 | 58.82 | < 0.0001 |
| Prior anal surgery | 7.30 | 32.03 | < 0.0001 |
| Stool artifact | 10.79 | 21.57 | 0.0032 |
Patients in Group 2 showed lower pain scores than those in Group 1 (2.52 versus 3.11, P = 0.003). At the end of the day, the patients who got the test process explanation in detail promptly prior to the examination start and were permitted to watch ongoing images had lesser pain in contrast to patients who did not.
The results of the variables for TRU associated pain using multivariate regression analysis are presented in Table 3. The analysis demonstrated that prostate sagittal length is the continuous variable impacting the pain level. Group 2 categorization and prior TRU experience was found to be in negative association with the pain score, while hemorrhoids (external), prior anal surgery, and stool artifact were in positive association with the pain score.
Multivariate Regression Analysis for Trans Rectal Ultrasonography (TRU) Associated Pain
| Variables | Regression Coefficient (β) | Standard Error (β) | P Value |
|---|---|---|---|
| Age (years) | -0.02371 | 0.0082 | 0.0771 |
| Body mass index (kg/m2) | -1.003622 | 0.0409 | 0.8357 |
| Prostate volume (mL) | -0.00232 | 0.0030 | 0.4621 |
| Prostate specific antigen (ng/mL) | 0.00003821 | < 0.001 | 0.617 |
| Prostate sagittal length (cm) | 0.005437 | 0.0011 | 0.0061 |
| Prior TRU experience (with none) | -0.3244 | 0.1834 | 0.0399 |
| Group 2 (with Group1) | -0.4583 | 0.2640 | 0.0065 |
| Prostate calcification (with none) | 0.6538 | 0.1720 | 0.1472 |
| Hemorrhoids external (with none) | 1.352 | 0.2116 | < 0.0001 |
| Prior anal surgery (with none) | 1.647 | 0.3126 | < 0.0001 |
| Stool artifact (with none) | 0.6254 | 0.2270 | 0.0038 |
5. Discussion
VAS is a straightforward evaluation device composed of a 10 cm line with “0 toward one side and “10” on another side. Patients grade their level of pain by setting a mark on line that relates to their present level. It is utilized as baseline pain assessment and to assess the effectiveness of the therapy (8). VAS is extensively utilized in numerous pain research areas since it is straightforward, takes < 1 minutes for completion, and it is highly reliable and valid (9). Hence, we utilized VAS in the present study. Assessing the pain level using VAS and thereby investigating the factors impacting pain amid TRU guided biopsy have been examined in the literature (5-7). Although we have conducted this research, there is a dearth of studies that have concentrated on the level of pain encountered by patients getting prostate TRU. Despite the fact that the test is viewed as a simple exam by urologists and it needs no local anesthesia, a few patients declare to have encountered severe pain through the test. Subsequently, we concentrated on deciding the pain score distribution in patients and distinguishing the factors impacting pain. The results demonstrated normal distribution of the pain scores encountered by patients and the mean pain score of just 2.79 indicating that a large portion of patients endured pain well and needed no anesthesia amid the test.
It was observed that the patients with pain scores > 3 were significantly younger in age than patients with pain scores < 4 (63.22 versus 64.88, P = 0.0182). Albeit multivariate regression-analysis demonstrated that age was an insignificant factor for pain (P = 0.0771). Philip et al. (10) and Rodriguez et al. (11) outlined that older patients had more pain tolerance amid TRU-guided biopsy of the prostate due to the comparatively lesser anal-resting-tone. The sphincter of internal anus gives about 60% - 70% of the anal-resting-tone, while the sphincter of external anus is in charge for 20% - 30%. The remainder 10% - 15% is ascribed to anal cushion development, called hemorrhoids (12-15). Younger patients have comparatively greater anal-resting-tone and lesser anorectal consistence amid insertion as well as withdrawal of the probe (10, 11). Hence, younger patients encounter more pain through the test. Prostate setup additionally plays a vital role in agony amid TRU. Results from the study demonstrated that prostate sagittal length, instead of prostate volume influenced the level of agony. Patients with more extended prostate sagittal length had greater pain since while prostate volume measurement, the ultrasonography probe should be embedded further in the rectum, bringing about more inconvenience.
Patients with external hemorrhoids represented about 37.6% of the whole study population. Hemorrhoids are divided into external hemorrhoids (distal to the dentate line), internal hemorrhoids (proximal to the dentate line), and mixed hemorrhoids (proximal/distal). External hemorrhoids are highly sensitive to pain, irritation, and itchiness when compared to internal ones (16). Amid TRU test, patients’ external hemorrhoids are aggravated and excruciating. In our examination, a greater pain score was recorded in patients with external hemorrhoids, which was an independent variable affecting pain. Additionally, patients with prior anal surgery were noted to have encountered greater pain amid TRU test. Obstructed scar tissue of the anus, asymptomatic stenosis, fibrosis or symptomatic strictures might happen after anal surgery. The rate of post anal stenosis is not very low and happens in approximately 4% - 5% of patients undergoing hemorrhoidectomy (17). A past study demonstrated that fistulectomy may likewise incite anal fibrosis (18). However, no patient mentioned experiencing the previously mentioned complications of surgery, we noted that prior anal surgery diminished the consistence of sphincter of anus and therefore, brought about more agony amid insertion as well as withdrawal of the probe. We suggest using the digital finger for incorporation with sufficient lubricant in order to wash the dry anal-canal, bit by bit expanding the sphincter of anus to forestall spasms. Insertion of probe can be performed gradually and delicately after the resting-anal-tone diminishes. Utilizing this strategy empowers decreasing the pain encountered amid TRU test by patients with external hemorrhoids/prior anal surgery. It is also additionally uncovered that patients encountered more pain in the presence of stool artifact, potentially in light of the fact that the analyst needed to acquire a higher quality picture by moving and altering the position of the ultrasound probe in the rectum. In this way, we recommend that patients with chronic constipation get enema prior to the test.
In a study by Czarnecki et al., it was specified that pain depends on the patient’s perception, and that it might be affected by interrelated components such as the patient’s psychological/emotional states, prior pain experience, anxiety levels, comprehension of the the technique, medical condition, and ecological factors (19). This might clarify why patients with prior TRU experience encountered lesser pain through the method. Besides, test process explanation in detail promptly prior to the examination start and permit to watch ongoing images decreased patient tension resulting in lesser pain. Tarhan et al. additionally demonstrated that video training about the technique of TRU biopsy could lessen patient tension (20). Hence, we emphasize that explanation in detail and the capacity to watch ongoing images of the test could lead to significant reduction in pain of anxious patients.
Certain inherent limitations required to be appraised during interpretation of the results of the current study. To begin with, a portion of the patients who got the examination conceivably had prostate tumor. We did not further talk about whether prostate cancer would influence the level of pain encountered by patients. In spite of the fact that our study affirmed that prior anal surgery was one of the independent variables impacting TRU associated pain, a portion of the given history essentially depended on self-report as opposed to medical chart review accuracy. This single-center study had a restricted number of patients. Therefore, generalization of the results should be made with care. Analysis of external hemorrhoids was done by the investigation of a urologist as opposed to an anorectal expert. Therefore, the high rate of external hemorrhoids among the patients was doubtful.
5.1. In Conclusion
Despite the fact that a TRU test is uncomfortable for patients, we observed that a large portion of patients had pain tolerance and needed no anesthesia amid the test. Be that as it may, 21.37% of the patients described moderate pain; whereas, 11.32% described severe pain. The analysis demonstrated influencing factors of TRU associated pain: prostate sagittal length, prior TRU experience, hemorrhoids (external), prior anal surgery, and stool artifact. Besides, test explanation in detail and capacity to watch ongoing images of the test could lead to significant reduction in pain of anxious patients.
Acknowledgements
References
-
1.
Watanabe H, Igari D, Tanahasi Y, Harada K, Saito M. Development and application of new equipment for transrectal ultrasonography. J Clin Ultrasound. 1974;2(2):91-8. [PubMed ID: 4136630].
-
2.
Alkan I, Turkeri L, Biren T, Cevik I, Akdas A. Volume determinations by transrectal ultrasonography in patients with benign prostatic hyperplasia: correlation with removed prostate weight. Int Urol Nephrol. 1996;28(4):517-23. [PubMed ID: 9119637].
-
3.
Terris MK, Stamey TA. Determination of prostate volume by transrectal ultrasound. J Urol. 1991;145(5):984-7. [PubMed ID: 2016815].
-
4.
Van PC, Decaestecker K, Hoebeke P. Correlation between prostate volume measured by transrectal and suprapubic ultrasound: can we do without TRUS? Global congress on Prostate Cancer, Marseille. France. 2013.
-
5.
Seymour H, Perry MJ, Lee-Elliot C, Dundas D, Patel U. Pain after transrectal ultrasonography-guided prostate biopsy: the advantages of periprostatic local anaesthesia. BJU Int. 2001;88(6):540-4. [PubMed ID: 11678747].
-
6.
von Knobloch R, Weber J, Varga Z, Feiber H, Heidenreich A, Hofmann R. Bilateral fine-needle administered local anaesthetic nerve block for pain control during TRUS-guided multi-core prostate biopsy: a prospective randomised trial. Eur Urol. 2002;41(5):508-14. discussion 514. [PubMed ID: 12074792].
-
7.
Irani J, Fournier F, Bon D, Gremmo E, Dore B, Aubert J. Patient tolerance of transrectal ultrasound-guided biopsy of the prostate. Br J Urol. 1997;79(4):608-10. [PubMed ID: 9126093].
-
8.
Huskisson EC. Measurement of pain. Lancet. 1974;2(7889):1127-31. [PubMed ID: 4139420].
-
9.
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S240-52. [PubMed ID: 22588748]. https://doi.org/10.1002/acr.20543.
-
10.
Philip J, McCabe JE, Roy SD, Samsudin A, Campbell IM, Javle P. Site of local anaesthesia in transrectal ultrasonography-guided 12-core prostate biopsy: does it make a difference? BJU Int. 2006;97(2):263-5. [PubMed ID: 16430625]. https://doi.org/10.1111/j.1464-410X.2006.05957.x.
-
11.
Rodriguez A, Kyriakou G, Leray E, Lobel B, Guille F. Prospective study comparing two methods of anaesthesia for prostate biopsies: apex periprostatic nerve block versus intrarectal lidocaine gel: review of the literature. Eur Urol. 2003;44(2):195-200. [PubMed ID: 12875938].
-
12.
Bennett RC, Duthie HL. The functional importance of the internal sphincter. Br J Surg. 1964;51:355-7.
-
13.
Lestar B, Penninckx F, Kerremans R. The composition of anal basal pressure. An in vivo and in vitro study in man. Int J Colorectal Dis. 1989;4(2):118-22. [PubMed ID: 2746132].
-
14.
Frenckner B, Euler CV. Influence of pudendal block on the function of the anal sphincters. Gut. 1975;16(6):482-9. [PubMed ID: 1150119].
-
15.
Gibbons CP, Bannister JJ, Trowbridge EA, Read NW. Role of anal cushions in maintaining continence. The Lancet. 1986;327(8486):886-8. https://doi.org/10.1016/s0140-6736(86)90990-6.
-
16.
Jacobs D. Clinical practice. Hemorrhoids. N Engl J Med. 2014;371(10):944-51. [PubMed ID: 25184866]. https://doi.org/10.1056/NEJMcp1204188.
-
17.
Sayfan J, Becker A, Koltun L. Sutureless closed hemorrhoidectomy: a new technique. Ann Surg. 2001;234(1):21-4. [PubMed ID: 11420479].
-
18.
Theerapol A, So BY, Ngoi SS. Routine use of setons for the treatment of anal fistulae. Singapore Med J. 2002;43(6):305-7. [PubMed ID: 12380728].
-
19.
Czarnecki ML, Turner HN, Collins PM, Doellman D, Wrona S, Reynolds J. Procedural pain management: a position statement with clinical practice recommendations. Pain Manag Nurs. 2011;12(2):95-111. [PubMed ID: 21620311]. https://doi.org/10.1016/j.pmn.2011.02.003.
-
20.
Tarhan H, Cakmak O, Unal E, Akarken I, Un S, Ekin RG, et al. The effect of video-based education on patient anxiety in men undergoing transrectal prostate biopsy. Can Urol Assoc J. 2014;8(11-12):894-900. [PubMed ID: 25553162]. https://doi.org/10.5489/cuaj.2208.
