Abstract
Objectives:
This study aimed to assess the diurnal variation of short term maximal performance and biological markers of hormonal [cortisol (CRT), testosterone (TST), melatonin (MLT)], biochemical [creatine phosphokinase (CPK), blood glucose (GLC), uric acid (UA)] and hematological [white blood cells (WBC), monocytes (MO), neutrophils (NE), lymphocytes (LY), red blood cells (RBC), hemoglobin (HB), hematocrit (HMT)] parameters in male police officers.Methods:
Twenty male police officers performed a running-based anaerobic sprint test (RAST) at two different times of the day (TOD), in the morning (6:00 h - 7:00 h) and evening (19:00 - 20:00) where blood samples were collected from the participants on these two occasions before each exercise session.Results:
Short term maximal performance [Peak power (PP), average power (AP) and minimal power (MP)] was higher in the evening as compared to the morning. It was noted that biological markers of hormonal, biochemical and hematological parameters exhibit diurnal fluctuation. Some of them peak in the morning (MLT, CRT, TST, UA, RBC, HB, and HMT) and others peak in the evening (GLC, CPK, WBC, NE, LY, and MO).Conclusions:
Short term maximal performance, hormonal, biochemical and hematological parameters were strongly affected by the TOD in police officers. Thus, understanding changes in short term maximal exercice and these circulating mediators during different TOD provide a better understanding of the anaerobic metabolism and could help modulate and quantify training load.Keywords
1. Background
The human body, encompassing it physiological and biochemical processes, follows a circadian rhythm, with the suprachiasmatic nucleus regulating the sleep-wake cycle and other bio-rhythms (1). As a result of physiological diurnal variations, psychological and performance parameters also follow this pattern affecting physical exercise performance, as seen in several studies (2-4). Peak values in short-term high intensity exercise was observed during afternoon with amplitudes of ~ 2% - 22% as revealed by Chtourou (5), Peak and and mean power during a Wingate test were found to be significantly higher during afternoon compared to morning in a group of physically active students (2, 6).
Past studies have mainly focused on how the time of day affects short term maximal performance in highly trained athletes, students or sedentary participants but no studies have focused on the diurnal variation of short term maximal performance or the biological parameters of police officers.
Continual short-term high intensity efforts require aerobic and anaerobic pathways (7). The Military Police Physical Training programme is an exercise program with a principle of specificity seeking to enhance the physical standards which are desirable for the demanding activities of this profession (8), wherein anaerobic and aerobic metabolism of the individual play a big role in efficiency of performance (8). Police officers are expected to perform a physically demanding task as part of their potentially hazardous career, whilst upholding their duties to protect the public and prevent crimes. There is always an unexpected potential incident when a police officer could be involved in, with very little warning, when they need to perform to the best of their physical and mental abilities with a good reserve of anaerobic metabolism needed in such circumstances (9, 10).
Short-term physical exercice is very similar to the emergency reaction demands of the job requirements of police officers. However, understanding morning-to-evening variations in short term maximal performance and resting biological parameters could be helpful to a better understanding of their metabolism and hence contribute to better quantifying of training loads and improving physical fitness, ameliorating their rediness to such emergency situations.
2. Objectives
Hence, this study aims to assess the potential effects of diurnal variation in short term maximal performance, hormonal, biochemical and haematological parameters in young male police officers to ascertain the effectiveness of the same.
3. Methods
3.1. Participants
Twenty healthy active men (age: 25.85 ± 2.03 years, height 1.78 ± 0.07 m, body mass: 80.17 ± 6.96 kg, BMI: 25.39 ± 2.17 kg.m-2) were recruited as voluntary participants in this study. They signed an informed consent after a complete description of the protocol was explained. A minimum of 5 years of regular physical exercise and training previously was a requirement prior to participation. Their daily training was including various short-term maximal exercises as per the police training requirements. Participants were nonsmokers and did not consume nutritional supplements, caffeine, drugs, or alcoholic beverages prior to enrolment into the study. They had no history of insomnia and had regular sleeping schedules. Throughout the experimental period, participants were required to maintain their habitual physical activity and to avoid strenuous physical efforts 24 h before each test session.
Participants were familiarised with the running-based anaerobic sprint test (RAST) as part of their daily training. They were used to the exact study protocol during the week preceding the experiment. In addition, sessions were conducted far from the full moon to avoid the effect of circa-lunar variation on the measured parameters (11).
The study was conducted according to the principals outlined in the Declaration of Helsinki and was approved by the ethical committee of Hospital Farhat Hachad, Sousse, Tunisia (code: FH20201026).
3.2. Experimental Protocol
The experimental design consisted of two nights carried out at the sleep laboratory. Participants completed blood test analysis on two separate occasions (in the morning between 6:00 h and 7:00 h and in the evening between 19:00 h and 20:00 h).
Participants had to come to the laboratory the night before the study to avoid the potential effect of light exposure on endogenous melatonin (MLT) in the day’s preceding the experiment. The protocol was to be at the sleep laboratory at 19:30 h on the night before. They consumed a standardized dinner one hour later, followed by ~90 min of informal activity (e.g. reading, watching television, playing videogames or cards, etc.) until 22:00 h when the participants were instructed to go to sleep (all lights and stimulating devices switched off). The different sleep sessions were realized under constant routine conditions (luminosity < 8 lux, temperature 21°C, semi-recumbent posture in bed). Sleep was controlled in this study to avoid the potential effect of sleep disruption on the short term maximal performance the following day.
In the morning testing sessions, participants were awakened at 06:00 h (following 8 hours of bedtime), which corresponded to their daily routine. They, then undertook 30 minutes of rest on comfortable armchairs. After this, fasting blood samples were collected, following which they performed the RAST test.
In the evening testing sessions, participants were awakened at 06:00 h (following 8 hours of bedtime, during the day of the study), which correlated to their daily practice. They then had a standardized breakfast (quantitatively and qualitatively) at 06:30 h. They were intructed to stay awake until 12:00 h continuing to do similar passive activities as in the previous evening. During this time, the subjects were not allowed to consume eatables, but were allowed to drink water as needed. At ~12:00 h, participants ate a standardized iso-caloric lunch, following which they continued with their passive activities untill 18:30 h. Thereafter, they took 30 minutes of rest on comfortable armchairs followed by the evening blood test samples taken for analysis after which they undertook the RAST.
3.3. RAST
The short-term maximal performance was evaluated with the RAST. RAST is composed of 6 × 35-m maximal sprints interspersed by 10-second of passive recovery. Each participant performed a 12 min warm-up (jogging followed by active dynamic stretching), followed by 3 min recovery. The following variables were then calculated: peak power (PP), average power (AP) and minimal power (MP) according to Zagatto et al. (12).
3.4. Blood Testing and Analysis
Venous samples were collected from median cubital vein of the right forearm of each participant, after 5 minutes rest on the blood collection chair [using vacuitainer blood collection system and tubes (BD, USA)].
The intra-assay and inter-assay coefficients of variation were 5.5 and 9.5% for MLT; 4.05 and 6.7% for cortisol (CRT); 4.46 and 8.06% for testosterone (TST), 1.55 and 4.65% for creatine phosphokinase (CPK), 1.76 and 2.8% for uric acid (UA), 0.94 and 1.3% for blood glucose (GLC), 3.5 and 5.4% for white blood cells (WBC), 4.6 and 6.1% for neutrophils (NEU), 3.9 and 8.4% for monocytes (MO), 1.5 and 3.8% for lymphocytes (LY), 2.1 and 6.5% for Red blood cells (RBC), and 1.5 and 2.5% for hemoglobin (Hb), respectively.
To annihilate inter-assay variance, all blood samples were retested in duplicate at the same laboratory, run in the same assay and mean values were used for the study purpose.
3.5. Statistical Analysis
Quantitative data were reported as mean ± SD. The Kolmogorov-Smirnov normality test showed that data were normally distributed, thus parametric tests were used. Data was analysed using a one-way ANOVA with repeated measures. Partial eta-squared (ηp2) was calculated to assess the ANOVA practical significance. Once the ANOVA indicated a significant main effect of the time of the day (TOD), the Bonferroni post-hoc test was used. Furthermore, the effect size (d) was calculated for pairwise comparison according to Cohen (13). The magnitude of d was classified as trivial (< 0.2), small (≥ 0.2 - 0.6), moderate (≥ 0.6 - 1.2), large (≥ 1.2 - 2.0) and very large (≥ 2.0) according to Batterham (14). All statistical analyses were conducted using the statistical package for the social sciences (SPSS, version 18.0, SPSS Inc, Chicago, IL, USA). The significance level was set at P < 0.05.
4. Results
4.1. RAST Results
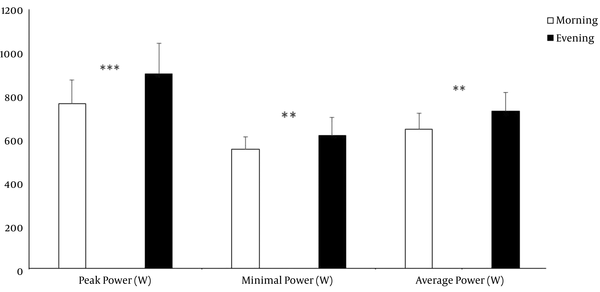
The present findings showed the TOD affected PP, AP and MP (F(1,76) = 14.70; P < 0.001; ηp2 = 0.16), F(1,76) = 8.12; P < 0.01; ηp2 = 0.1), F(1,76) = 11.62; P < 0.001; ηp2 = 0.13). The Post Hoc revealed that PP, AP and MP were greater in the evening compared to the morning (P < 0.001, < 0.01, < 0.01; d = 1.08, = 1, = 0.85) (Figure 1).
Effect of the time of the day on the Running-based Anaerobic Sprint test (RAST). **, ***, Significant difference between morning and evening (P < 0.01, P < 0.001, respectively)
4.2. Hormonal Results
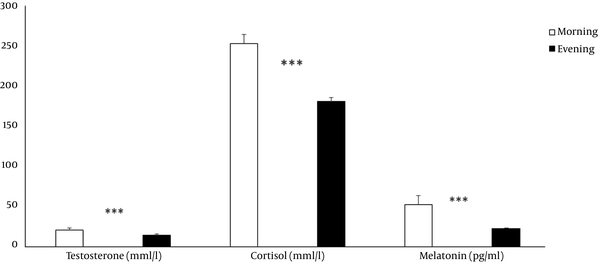
The present findings showed the TOD affected MLT (F(1,76) = 2444.59; P < 0.001; ηp2 = 0.97), CRT (F(1,76) = 93.34; P < 0.001; ηp2 = 0.55) and TST (F(1,76) = 1701.21; P < 0.001; ηp2 = 0.95). The post hoc revealed that MLT, CRT and TST levels were higher in the morning compared to the evening (P < 0.001; d = 10.12, d = 1.21, = 10.47, respectively) (Figure 2).
Effect of the time of the day on hormonal parameters. ***, Significant difference between morning and evening (P < 0.001)
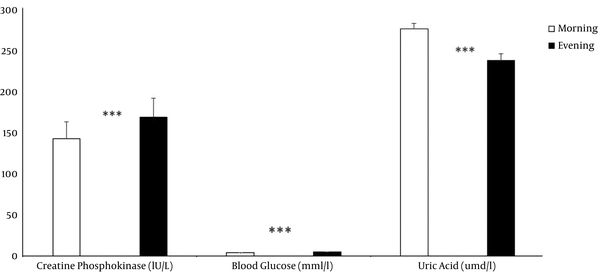
4.3. Biochemical Results
The present findings showed revealed a TOD effect for GLC (F(1,76) = 296.17; P < 0.001; ηp2 = 0.79), UA (F(1,76) = 441.45; P < 0.001; ηp2 = 0.85), and CPK (F(1,76) = 363.95; P < 0.001; ηp2 = 0.82) (Table 1). The post hoc revealed that GLC and CPK were higher in the evening compared to morning (P < 0.001; d = 4.2, = 4.34, respectively). Moreover, UA was higher in the morning compared to the evening P < 0.001; d = 4.35) (Figure 3).
Effect of the time of the day on biochemical parameters. ***, Significant difference between morning and evening (P < 0.001)
| Morning | Evening | |
|---|---|---|
| CPK, IU/L | 151.50 ± 8.07 | 178.00 ± 4.39b |
| GLC, mmol/L | 4.10 ± 0.21 | 4.90 ± 0.23b |
| UA, µmol/L | 275.55 ± 7.29b | 232.70 ± 9.26 |
| WBC, × 103/µL | 6.96 ± 0.54 | 7.64 ± 0.58b |
| NE, × 103/µL | 3.49 ± 0.21 | 4.42 ± 0.14b |
| LY, × 103/µL | 2.26 ± 0.19 | 2.69 ± 0.19b |
| MO, × 103/µL | 0.70 ± 0.12 | 0.78 ± 0.12b |
| RBC, × 106/µL | 5.24 ± 0.25b | 4.68 ± 0.19 |
| HGB, g/dL | 15.62 ± 0.55b | 14.87 ± 0.45 |
| HCT, % | 44.79 ± 0.75b | 43.65 ± 0.46 |
4.4. Hematological Results
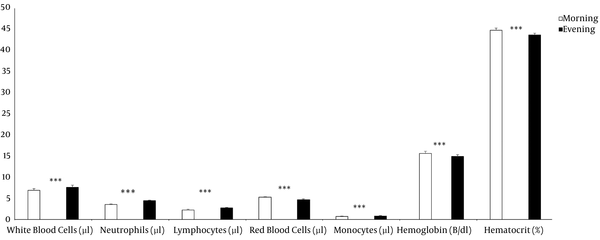
The present findings showed an effect of TOD on WBC, NEU, LY, RBC, MO, HGB, and HCT (F(1,76) = 36.96; P < 0.001; ηp2 = 0.32, F(1,76) = 639.28; P < 0.001; ηp2 = 0.89, F(1,76) = 108.33; P < 0.001; ηp2 = 0.58, F(1,76) = 124.08; P < 0.001; ηp2 = 0.62, F(1,76) = 12.65; P < 0.001; ηp2 = 0.14, F(1,76) = 31.26; P < 0.001; ηp2 = 0.29, F(1,76) = 36.22; P < 0.001; ηp2 = 0.32, respectively) (Table 1). The post hoc revealed that WBC, NEU, LY, and MO were higher in the evening compared to the morning (P < 0.001 for all; d = 1.56, d = 5.4, d = 2.42, d = 0.88, respectively). Further, RBC, HGB, and HCT were higher in the morning compared to the evening during (P < 0.001; d = 1.95, d = 1.03, d = 1.84, respectively) (Figure 4).
Effect of the time of the day on hematological parameters. ***, Significant difference between morning and evening (P < 0.001)
5. Discussion
This study investigated diurnal variations of short-term maximal physical performance as well as biological markers of hormonal, biochemical and hematological parameters in male police officers.
The main findings were that RAST performance (PP, AP and MP) exhibits diurnal variation with a better performance recorded in the evening as compared to the morning. Additionally, hormonal, biochemical and hematological profile exhibits diurnal fluctuation too. Some of them peak in the morning (MLT, CRT, TST, UA, RBC, HB and HMT) whilst others peak in the evening (GLC, CPK, WBC, NE, LY, and MO).
The short term maximal performance of RAST was clinically significant in the evening as compared to the morning (Figure 1), as shown in previous studies too (15-17). Zarrouk et al. (16) also showed that high-intensity short duration performance was much more productive in the afternoon as compared to morning times. There was a 3% - 21% variability in the muscle strength, power and sprint ability amongst the athlete group tested (5). A possible explanation for this could have been attributed to an increase in core temperature in the afternoon with diurnal fluctuation of body temperature too (5, 15, 17). A study done by West et al. (17) showed a 5.1% reduced physical performance in a group of elite athletes with a small morning-to-evening change in core temperature. A significantly better mechanical response to motor neuron stimulation causing improved muscle force and contractility was noted with a diurnal variation, more enhanced in the evening (18). Other factors which could influence RAST could be age, experience of study subjects, their nutritional status, training level and sleeping behaviours (5, 15).
As mentioned previously, this is first study to show the effect of diurnal variation on short term maximal performance in police officers, as the previous studies have focused mainly on elite athletes or sedentary participants.
The present findings showed that the participants’ hormonal, biochemical, and hematological profile exhibits diurnal fluctuations. Some variables peak in the morning (i.e., CRT, TST, UA, RBC, HGB, and HCT) and other peaks in the evening (i.e., MLT, GLC, CPK, WBC, NEU, LY, MO).
Concerning MLT, our findings revealed that this hormone is higher during early morning to the evening. Circulating MLT levels were lower during the day and much higher at night, peaking near the midpoint of the dark interval (19). Throughout the day, MLT secretion is inhibited by light via the inhibition of serotonin N-acetyl transferase activity reflecting very low or undetectable diurnal serum levels (< 10 pg/mL) (20). Serum concentrations of MLT increase significantly at night and become more prominent from 22:00 h. The secretion of MLT persists for about 10 h, with a peak (between 30 and 200 pg/mL) recorded around 2 A.M. (20). A plateau is observed up to 5 h, after which the rate decreases rapidly to regain its basal diurnal level (20).
In our study, the participant’s usual wake time was 5:30 A.M. and the blood test was conducted just 30 minutes to 1 hour later. Thus, the authors postulate that the higher level of MLT in the morning could be an indicator of the beginning of the drop of MLT regaining its basal diurnal level. Similarly, the participant’s usual sleep time was 9 P.M. and the blood test was conducted 1 to 2 hours before sleep. The authors think that the lower level of MLT around the late afternoon could be corresponding to the beginning of the formation of MLT plateau. In this way, comparing the present findings to previous results on the diurnal variation of MLT, its endogenous level should be lower or almost undetected at this time (20). As a result, the higher MLT level in this study could be explained by the participant’s early usual time to bed.
The results also revealed that CRT was higher in the morning as compared to the evening for both conditions (FM and NM), which was in line with previous studies (19). The CRT rhythm could be used as a phase marker of the circadian clock (21). Concerning TST, the study findings showed that TST concentration was higher in the morning compared to the evening. In the same way, previous studies showed that TST levels displayed circadian variation, peaking during sleep and reaching a nadir during late afternoons (22).
Sale et al. (23) linked TST and CRT to physical performance, showing negative effects of raised CRT on neuromuscular functions, in the morning. They used transcranial magnetic stimulation to stimulate the primary motor cortex, to evaluate the diurnal variation on the neuromuscular system in this study. The motor-evoked potentials were lower in the mornings due to increased CRT levels, evaluated by electromyographic recordings.
Circadian rhythm of hormonal parameters was ascertained by Bird and Tarpenning (24), showing an anabolic tendency of hormonal profile, favouring strength and muscle adaptation associated with resistance exercise in their subjects. The TST/CRT ratio was greater in the evening, with a lower pre-exercise CRT level, postulating a diminished catabolic state which could be advantageous for training adjustments. The subjects in this study has at least a years’ weight lifting experience and it is possible that the positive alteration recorded in the hormonal profile in this study could have been affected by the training status of the subjects (25).
Similar to the present findings in this study, previous reports (26-28) have shown that resting levels of CPK were greater in the evening than during morning. The maximal rates of production of CPK are in phase with the circadian rhythm of body temperature, which is a well known fact (26). However, the current results showed that UA levels were higher in the morning than in the evening. As per the authors knowledge, only a small number of studies have investigated the diurnal variation of UA in humans (26, 27). These investigations found that the acrophase of UA occurs during early morning, which confirms the results in this study. Moreover, this study showed that the plasma levels of GLC were greater in the evening than during morning, which is in concurrence with the study conducted by Ammar et al. (28).
Furthermore, regarding the hematological parameters, the current study revealed that WBC and their sub-populations (MO, NEU and LY) were remarkably higher during evening than in the morning. Likewise, previous studies have recognized that the acrophase of these parameters were placed between 18:00 h and 24:00 h in day-active people (26, 27). These diurnal disparities have been shown to be associated with the circadian rhythm of core temperature (26, 27).
However, to the author’s knowledge, the present analysis is the first study to investigate the diurnal variations of short term maximal performances and the hormonal, biochemical and hematological profile in male police officers.
A main limitation of the present study was that short term maximal performance and hormonal, biochemical and hematological parameters were assessed only on two-measurement points per day, namely morning and evening. It is probable that such a large gap in measurements could miss the peak and nadir of performance during the time period. Hence, this study was unable to delineate the thorough extent of diurnal variation in short term maximal performance and hormonal, biochemical and hematological parameters in police officers. Thus, further research needs to be conducted to assess these parameters during different TOD to study the circadian rhythmicity of the above mentioned parameters. Another limitation of this study was that post-short term exercice biological responses was not assessed, which could probably have given a better explanation for the anaerobic metabolism after RAST in the study participants.
The authors also recommend future studies to use specific “police test protocol” rather than test protocols related to sport performance to have more distinct results.
5.1. Conclusions
The results reveal that, in police officers, diurnal variation exert a major effect on their physical performance and their biological rhythms. Although enhanced performance is most frequently seen in the early evenings, taking into consideration an individuals’ specific time-of-day training, it is suggested to play an important role in improving their physical performance. Hence, for police officers, the time-of-day on short term maximal repetitive exercise should be contemplated as well as other biological makers of hormonal, biochemical and hematological parameters, as shown in this study. The authors suggest further research in this field to evaluate accomplishment during repeated high-intensity bouts using a specific police test protocol and correlate if it delivers similar results as this study.
Acknowledgements
References
-
1.
Teo W, Newton MJ, McGuigan MR. Circadian rhythms in exercise performance: implications for hormonal and muscular adaptation. J Sports Sci Med. 2011;10(4):600-6. [PubMed ID: 24149547]. [PubMed Central ID: PMC3761508].
-
2.
Chtourou H, Hammouda O, Chaouachi A, Chamari K, Souissi N. The effect of time-of-day and Ramadan fasting on anaerobic performances. Int J Sports Med. 2012;33(2):142-7. [PubMed ID: 22318530]. https://doi.org/10.1055/s-0031-1286251.
-
3.
Chtourou H, Ammar A, Nikolaidis PT, Abdel Karim O, Souissi N, Chamari K, et al. Post-resistance training detraining: time-of-day effects on training and testing outcomes. Biol Rhythm Res. 2015;46(6):897-907. https://doi.org/10.1080/09291016.2015.1063204.
-
4.
Pullinger SA, Oksa J, Clark LF, Guyatt JWF, Newlove A, Burniston JG, et al. Diurnal variation in repeated sprint performance cannot be offset when rectal and muscle temperatures are at optimal levels (38.5 degrees C). Chronobiol Int. 2018;35(8):1054-65. [PubMed ID: 29566344]. https://doi.org/10.1080/07420528.2018.1454938.
-
5.
Chtourou H, Souissi N. The effect of training at a specific time of day: a review. J Strength Cond Res. 2012;26(7):1984-2005. [PubMed ID: 22531613]. https://doi.org/10.1519/JSC.0b013e31825770a7.
-
6.
Chtourou H, Zarrouk N, Chaouachi A, Dogui M, Behm DG, Chamari K, et al. Diurnal variation in Wingate-test performance and associated electromyographic parameters. Chronobiol Int. 2011;28(8):706-13. [PubMed ID: 21793694]. https://doi.org/10.3109/07420528.2011.596295.
-
7.
Chtourou H, Engel FA, Fakhfakh H, Fakhfakh H, Hammouda O, Ammar A, et al. Diurnal Variation of Short-Term Repetitive Maximal Performance and Psychological Variables in Elite Judo Athletes. Front Physiol. 2018;9:1499. [PubMed ID: 30416454]. [PubMed Central ID: PMC6212582]. https://doi.org/10.3389/fphys.2018.01499.
-
8.
da Silveira CL, de Souza TS, Batista GR, de Araujo AT, da Silva JC, de Sousa Mdo S, et al. Is long term creatine and glutamine supplementation effective in enhancing physical performance of military police officers? J Hum Kinet. 2014;43:131-8. [PubMed ID: 25713653]. [PubMed Central ID: PMC4332172]. https://doi.org/10.2478/hukin-2014-0098.
-
9.
Vanhees L, Lefevre J, Philippaerts R, Martens M, Huygens W, Troosters T, et al. How to assess physical activity? How to assess physical fitness? Eur J Cardiovasc Prev Rehabil. 2005;12(2):102-14. [PubMed ID: 15785295]. https://doi.org/10.1097/01.hjr.0000161551.73095.9c.
-
10.
Lentz L, Randall JR, Guptill CA, Gross DP, Senthilselvan A, Voaklander D. The Association Between Fitness Test Scores and Musculoskeletal Injury in Police Officers. Int J Environ Res Public Health. 2019;16(23). [PubMed ID: 31771132]. [PubMed Central ID: PMC6926534]. https://doi.org/10.3390/ijerph16234667.
-
11.
Dergaa I, Fessi MS, Chaabane M, Souissi N, Hammouda O. The effects of lunar cycle on the diurnal variations of short-term maximal performance, mood state, and perceived exertion. Chronobiol Int. 2019;36(9):1249-57. [PubMed ID: 31368366]. https://doi.org/10.1080/07420528.2019.1637346.
-
12.
Zagatto AM, Beck WR, Gobatto CA. Validity of the running anaerobic sprint test for assessing anaerobic power and predicting short-distance performances. J Strength Cond Res. 2009;23(6):1820-7. [PubMed ID: 19675478]. https://doi.org/10.1519/JSC.0b013e3181b3df32.
-
13.
Cohen J. Quantitative methods in psychology: A power primer. Psychol Bull. 1992;112:1155-9.
-
14.
Batterham AM. Comment on probabilities of clinical or practical significance. Sportscience. 2002;6.
-
15.
Mhenni T, Michalsik LB, Mejri MA, Yousfi N, Chaouachi A, Souissi N, et al. Morning-evening difference of team-handball-related short-term maximal physical performances in female team handball players. J Sports Sci. 2017;35(9):912-20. [PubMed ID: 27352917]. https://doi.org/10.1080/02640414.2016.1201212.
-
16.
Zarrouk N, Chtourou H, Rebai H, Hammouda O, Souissi N, Dogui M, et al. Time of day effects on repeated sprint ability. Int J Sports Med. 2012;33(12):975-80. [PubMed ID: 22782387]. https://doi.org/10.1055/s-0032-1312626.
-
17.
West DJ, Cook CJ, Beaven MC, Kilduff LP. The influence of the time of day on core temperature and lower body power output in elite rugby union sevens players. J Strength Cond Res. 2014;28(6):1524-8. [PubMed ID: 24149752]. https://doi.org/10.1519/JSC.0000000000000301.
-
18.
Guette M, Gondin J, Martin A. Time-of-day effect on the torque and neuromuscular properties of dominant and non-dominant quadriceps femoris. Chronobiol Int. 2005;22(3):541-58. [PubMed ID: 16076653]. https://doi.org/10.1081/CBI-200062407.
-
19.
Czeisler CA, Klerman EB. Circadian and sleep-dependent regulation of hormone release in humans. Recent Prog Horm Res. 1999;54:97-130. discussion 130-2. [PubMed ID: 10548874].
-
20.
Benloucif S, Burgess HJ, Klerman EB, Lewy AJ, Middleton B, Murphy PJ, et al. Measuring melatonin in humans. J Clin Sleep Med. 2008;4(1):66-9. [PubMed ID: 18350967]. [PubMed Central ID: PMC2276833].
-
21.
Van Cauter E, Refetoff S. Multifactorial control of the 24-hour secretory profiles of pituitary hormones. J Endocrinol Invest. 1985;8(4):381-91. [PubMed ID: 2999212]. https://doi.org/10.1007/BF03348519.
-
22.
Wittert G. The relationship between sleep disorders and testosterone in men. Asian J Androl. 2014;16(2):262-5. [PubMed ID: 24435056]. [PubMed Central ID: PMC3955336]. https://doi.org/10.4103/1008-682X.122586.
-
23.
Sale MV, Ridding MC, Nordstrom MA. Cortisol inhibits neuroplasticity induction in human motor cortex. J Neurosci. 2008;28(33):8285-93. [PubMed ID: 18701691]. [PubMed Central ID: PMC6670557]. https://doi.org/10.1523/JNEUROSCI.1963-08.2008.
-
24.
Bird SP, Tarpenning KM. Influence of circadian time structure on acute hormonal responses to a single bout of heavy-resistance exercise in weight-trained men. Chronobiol Int. 2004;21(1):131-46. [PubMed ID: 15129828]. https://doi.org/10.1081/cbi-120027987.
-
25.
Lusa Cadore E, Lhullier FL, Arias Brentano M, Marczwski Da Silva E, Bueno Ambrosini M, Spinelli R, et al. Salivary hormonal responses to resistance exercise in trained and untrained middle-aged men. J Sports Med Phys Fitness. 2009;49(3):301-7. [PubMed ID: 19861937].
-
26.
Hammouda O, Chtourou H, Chahed H, Ferchichi S, Kallel C, Miled A, et al. Diurnal variations of plasma homocysteine, total antioxidant status, and biological markers of muscle injury during repeated sprint: effect on performance and muscle fatigue--a pilot study. Chronobiol Int. 2011;28(10):958-67. [PubMed ID: 22080741]. https://doi.org/10.3109/07420528.2011.613683.
-
27.
Hammouda O, Chahed H, Chtourou H, Ferchichi S, Miled A, Souissi N. Morning-to-evening difference of biomarkers of muscle injury and antioxidant status in young trained soccer players. Biol Rhythm Res. 2012;43(4):431-8. https://doi.org/10.1080/09291016.2011.599638.
-
28.
Ammar A, Chtourou H, Turki M, Hammouda O, Chaari A, Boudaya M, et al. Acute and delayed responses of steroidal hormones, blood lactate and biomarkers of muscle damage after a resistance training session: time-of-day effects. J Sports Med Phys Fitness. 2018;58(7-8):980-9. [PubMed ID: 28222580]. https://doi.org/10.23736/S0022-4707.17.07048-7.
