Abstract
Background:
Insole orthotics are prescribed to correct human body position during both the standing position and the motion of gait. Also, they are being applied for people who have forefoot abduction and arch deformation. However, a little is known about the relationship between forefoot and arch orthotic correction and the alternation in foot biomechanics.Objectives:
This study was aimed to determine the effect of non-prescription insole orthotics in walking gait parameters.Methods:
It was a quasi- experimental with pre-test, post-test design study. Twelve volunteer participants (41 ± 17 y), 10 men and two women, participated in this study. Three-dimensional (3D) cameras were used to do motion capture through those markers placed on lower body segments. Seven segments such as: Hip, left and right thigh, left and right shank, left and right foot were used for labelling in this study, which was measured with Vicon T-Series cameras at 250 Hz. The participants did walk in three different phases: Barefoot, running shoe, running shoe with a non-prescription orthotic inside. t-test was used to analyse the data.Results:
The paired t-test results indicated that there is significant difference in cadence, step length and stride length for running shoe, and non-prescription orthotics compare to those of barefoot (P ≤ 0.05). Additionally, it was found that, non-prescription orthotics resulted in higher step length and stride length, and less cadence (P ≤ 0.05). On the other hand, But, no significant changes were found for non-prescription orthotics (P ≥ 0.05).Conclusions:
It was concluded that cadence, step length and stride length were improved in running shoe compared to non-prescription orthotics group. But there were not any significant differences between running shoe and non-prescription orthotics.Keywords
1. Background
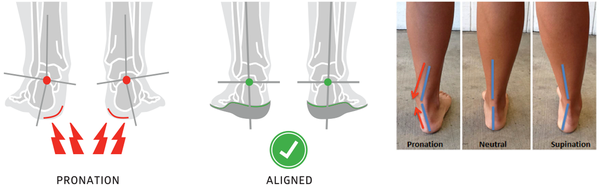
Pronation is the combination of dorsiflexion, abduction, and eversion (1). Through walking, pronation plays an important role in shock observation, and surface adaptation especially during stance phase. During walking, if pronation occurs 25% more than stance phase of walking then it can be said that there is an over-pronation (2). In other words, if pronation occurs at inappropriate time during walking or stance phase and lasts for a long time, overpronation arises (3). Excessive pronation relates to the way of walking and gaiting. It occurs when the foot arches become flattened more than usual excessive pronation or over-pronation can be as a result of repetitive inappropriate movements which have been habits in life, and influences all the muscles strength and length (3). Over-pronation usually followed by numerous lower body injuries like shin split (3), hip and pelvic dysfunction, knee pain and etc. (4). Therefore, all the human movement, posture and performance like walking can be affected by this abnormality (5). To diagnose over-pronation, Dahle et al. suggested a foot type classification scheme. It drew on both the visual observation and measurement of the feet (6). According to this scheme, over-pronation exists if calcaneal eversion, medial talonavicular bulge, and low longitudinal arch angle exceeds 3°, you can see sample in Figure 1. It has been resulted from this study that, over-pronation may not appear in the first step, especially in feet which have forefoot varus asymmetry or deformation, but later in stance phase.
Over-pronation visual recognition
The first “orthotics” dates back at least 2,000 years with underfoot shoe cushioning (7). Primary orthotics were rigid and ordeal to wear and could easily distort the shoe. Hence, it was not until 1910, Dr. William Scholl introduced first light and soft orthotics which were coined to support the arch. Finally, in 1920s, after having many changes in terms of material and shape, orthotic new models started being produced largely by most of the shoe companies (7).
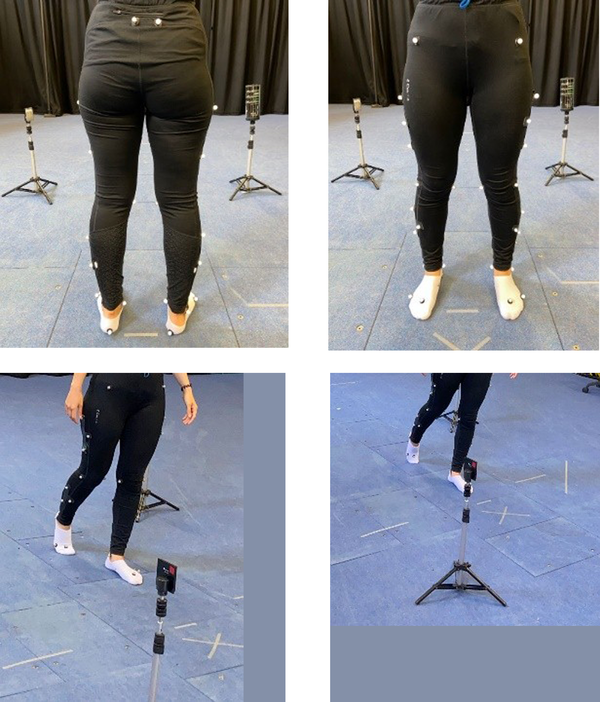
In fact, orthotics designed to prevent and treat lower body musculoskeletal injuries (8, 9). Nowadays, there are two different types of orthotics in the market. Moulded (prescription) and non-moulded (non-prescription). The prescription one would be produced after a personal visit and built according to the person foot shape, body weight, and foot deformity. In other words, analysing the foot is important and all the posture abnormalities and foot dysfunctions, foot shape and length should be recognized as the orthotics are being shaped and produced accordingly. Non-prescription orthotics are being produced by companies in a vast numbers and people can find them in markets with no prescription needed. Non-prescription (Figure 2) which was the one used in this study, is less time consuming to produce and less expensive. They are being offered to customers as a device that can help correct their overpronation. However, due to bulk production, they may be hard to fix in shoe, say, might be wider or narrow than shoe and do not provide enough support (10, 11) and less effective because they are not being produced according to patients’ anatomical differences. Basically, orthotics is being built from fibreboard and ethyl vinyl acetate (EVA), polypropylene, polyethylene, acrylic, fiberglass, carbon fibre composites and other types of cork, foams and laminates. The thickness and materials are being chosen according to patients’ weight and foot type and length. Orthotics are meant to reduce the effect of abnormal pronation on lower body by influencing foot function (12). More to the point, this acts by tilting the calcaneus in both the frontal and sagittal planes and restricts eversion, dorsiflexion, accordingly (13). As a result of applying insole orthotics, the highest point of the arch hits at the same time with the bottom of the heel which provides more arch support during walking (10).
Used non-prescription orthotics in this study

During walking, the kinematic alternation position of the foot may result in more efficient biomechanical correlation, especially at both the subtalar and midtarsal joints. It is likely to have less stress on lower body tissues by having a reduction of pronation beside changing in the timing of pronation during stance phase of gait. In this regard, the orthotics become important to help with over-pronation.
Statistically, efficacy of insole orthotics shows ambivalent results, where some trials reveal improvement and changes, and some trials do not (14). There are few studies which looked at the effect on prescription orthotics in walking in terms of gait velocity, and walking joint moment. Also, there are some other which looked at angular changes in lower body segments. For example, Genova and Gross looked at the effect on prescription orthotics on calcaneal eversion during standing and walking treadmill in people with overpronation (15). In this study, they asked participants start using prescription orthotics three weeks before data collection, which was the good point in this study (15). Because, it would provide more stable and reliable results in terms of familiarisation period. After three weeks, they performed the test by walking on the treadmill, results came out that prescription orthotics can reduce the eversion of calcaneal by 2.2°. Indeed, comparing the results, they found difference between standing position in bare foot and running shoe with and without orthotics. However, all participants in this study had a dramatic amount of calcaneal eversion equal to 10° which is a large amount, and the result might not apply for people with smaller amount. There have been very few articles regarding the effect of non-prescription orthotics in walking gait in people with over-pronation.
2. Objectives
This study was done to find a better understanding regarding any changes by applying non-prescription insole orthotics in walking gait among people with overpronation in terms of cadence, step length, stride length, ankle angle at heel strike, knee angle at toe-off, ankle angle at heel strike, and hip angle at hell strike plane to see if the non-prescription can make any significant differences. It was hypothesized that there would be changes in the all above factors in walking gait after applying non-prescription orthotics.
3. Methods
This was a quasi-experimental with pre-test, post-test design study to improve our understanding of the effect of non-prescription orthotics on kinematic factors during walking in people with over-pronation. Twelve volunteer participants men and women with mean average age of 41 ± 17 took part in this study. They all were recognised with overpronation, and had arch index which were recognised by visual observation. They all reported no lower extremity of hypertension, coronary disease, respiratory, or balance, metabolic, or neurological disorders. Data collection was done in University of Chichester, Biomechanics Lab 1. To start, all the camera got calibrated and the origin was set. And, light gates (Fusion Sport Smart Speed TM System) were placed at two meters distance from each other in middle of the lab. Having participants in the lab, before starting process for data collection, we provided them with an information sheet. All ahead process was explained to them and tried to make sure they are happy to go through the data collection. When they provided informed consent, they got retro-reflective markers (Vicon Motion Systems Ltd, Oxford, UK & B&L Engineering, Los Angeles, UK) placed on their lower limbs as was required by kinematic model (find the markers and light gate in Figure 3). Ten high speed Vicon infrared cameras (MX T-Series (T40-S) Camera) were sited on a rig around the ceiling of the Biomechanics Lab filming participants walking at 250 Hz. We could check walking speed by the light gates placed in the middle of the lab. All data collection for three different phases lasted maximum 1.5 hours.
Reflective markers on participant’ lower body segments, and light gates
All collected trials were labelled by using Vicon Nexus software version 2.11.0 (Vicon Motion Systems Ltd, Oxford, UK), and marker trajectory gaps were filled with either a quantic spline, or pattern-fill technique. Then, static and motion files C3d were transferred to Visual 3D software (C-Motion Technologies, USA) where the biomechanical model was built. The three-dimensional (3D) coordinates of the markers on the seven segments were smoothed using a lowpass filter with a cut off frequency of 10 Hz. All joint angles for ankle angle at toe-off and heel strike and midstance, knee angle at toe-off, and hip angle at heel strike during the gait cycle were calculated and expressed relative to the joint angles measured in the barefoot trials. Inversion and eversion rotation were defined about the longitudinal axis of the foot, and plantar flexion and dorsiflexion about transverse axis.
3.1. Procedure
Markers were places on the segments, participants then had the chance to have some familiarisation. Walking through the path that had been designed in order to familiarise with walking among light gates. Recording their starting position, subjects stepped their right foot forward first and walked through the light gates by their selected speed. First three trials were recorded to calculate average walking speed, and added lower and upper boundary which was ± 5%. When the boundaries were defined, only trials would be accepted which not exceeded or fallen below of those numbers. After barefoot walking, running shoe, and running shoe with orthotic inside trials were completed in the same way. Participants walked with their own running shoes.
It was important to have their natural walking pattern and speed, as could lead us to more ecologically valid results. Hence, participants had all they walking at their self-selected pace. Five good trials, those were performed in the time boundaries, were collected of each phase: Bare foot, running shoe, and running shoe with non-prescription orthotics inside. The reason for recording 5 good trials was to have stability in our data. In other words, stability in the trials will influence the stability of the mean value of the group, and validity of the data (16). Furthermore, the minimum 4 trials have been announced for making stability in data in walking. Following previous studies (17), we recorded 5 trials, as well. Sometimes during data collection, it took more times to keep the trials’ speed within the time boundaries for each participant. Hence, they could take a rest if they needed. When they had finished the trials, a survey was completed with the participants. The main purpose of this survey was to know about the participants opinion and feelings towards non-prescription orthotics. This can be the crucial point here, as not many studies have asked participants’ opinion and will be important to find if patients will continue to use orthotics afterwards. In this survey, the questions were regarding to their age, height and weight which needed for data interpretation and building biomechanical model. And, if they have ever used orthotics, because then they would share their experiences and opinion of orthotics efficiency, do they feel any pain during walking to make an understanding about the participants’ foot condition, did they feel any changes after applying orthotics, if yes what changes, and did they feel any balance improvement during walking with orthotics as it is believed that applying insole orthotics can improve balance during walking (Thompson Health Services, n.d.). All answers were recorded by writing down on paper. Overall, 216 trials were collected from participants from motion analysis. All these trials were collected in Nexus software version 2.11.0 (Vicon Motion Systems Ltd, Oxford, UK), and labelled according to UoC Lower Limb Model. It was tried to fill all the gaps in the data and save a C3d format of the final labelled trial. Transferring both the static and motion C3d file into Visual 3D software (C-Motion Technologies, USA) where the biomechanical model was built for each participant. At this time, we could use the information about their height and weight that was gained from the survey. A pipeline was built according to the factors we wanted to analyse. A low pass filter was created by cut off frequency of 10 HZ to provide a smoother form of signals. Four events were defined to run in the data, heel strike and toe off for both the left foot and right foot. Joint angles in all the X and Z axis at toe-off and heel strike and midstance phase were applied in pipeline. Following other studies, we looked at the right foot and used the data of right side of the body. Mean data were extract from all the eight analysing factors (cadence, step length, stride length, ankle sagittal plane angle at initial contact, knee sagittal plane angle at toe-off and hip sagittal plane angle at heel strike, ankle angle and midstance at X axis, and ankle angle at midstance in Z axis) for the right foot. The mean extraction could give us a more reliable data of the trials. Then, variables were run in the Excel to get a single mean value in five trials for three different phases, and both the mean and standard division (SD) were calculated. Because mean data extracted from 3D used to get a single mean value, so we could assume our data are normally distributed. Hence, t-test was run in RStudio to analysed our data. We run the test for barefoot and running show, barefoot and non-prescription orthotics, and running shoe with non-prescription orthotics. We looked at running shoe data to avoid underestimate its effect in case of having any changes. Then, comparing the results would show any differences are from which phase.
4. Results
Table 1, shows the means and SD from our data. Furthermore, see t-test result can be seen in Table 2.
Mean Values ± Standard Division of the Data for Different Analysing Factors
| Variables | Barefoot | Running Shoe | Non-prescription Orthotics |
|---|---|---|---|
| Cadence (steps/min) | 0.903 ± 0.065 | 0.858 ± 0.064 | 0.854 ± 0.855 |
| Step length (cm) | 0.663 ± 0.057 | 0.686 ± 0.048 | 0.691 ± 0.572 |
| Stride length (cm) | 1.313 ± 0.114 | 1.370 ± 0.106 | 1.377 ± 0.120 |
| Hip angle at HS (degree) | 150.803 ± 11.057 | 150.932 ± 12.977 | 150.134 ± 14.057 |
| Knee angle at TO (degree) | 130.847 ± 3.139 | 127.188 ± 6.778 | 128.776 ± 8.443 |
| Ankle angle at HS (degree) | 80.121 ± 8.217 | 79.415 ± 7.965 | 78.642 ± 7.432 |
| Ankle angle at midstance X (degree) | 78.818 ± 8.553 | 78.983 ± 8.183 | 77.756 ± 8.169 |
| Ankle angle at midstance Z (degree) | -16.838 ± 6.773 | -16.971 ± 7.174 | -17.832 ± 8.432 |
t-test Result
| Variables | Bare Foot and Running Shoe | Bare Foot and Non-prescription Orthotics | Non-prescription Orthotics and Running Shoe | |||
|---|---|---|---|---|---|---|
| P-Value | t-Value | P-Value | t-Value | P-Value | t-Value | |
| Right foot cadence | 0.001 | 7.09 | 0.001 | 4.458 | 0.686 | 0.416 |
| Right foot step length | 0.05 | -2.941 | 0.001 | -4.259 | 0.35 | -0.975 |
| Stride length | 0.001 | -3.323 | 0.001 | -3.163 | 0.825 | 0.226 |
| Hip angle at heel strike | 0.974 | -0.032 | 0.877 | 0.158 | 0.648 | 0.469 |
| Right knee angle at toe-off | 0.05 | 2.773 | 0.305 | 1.077 | 0.178 | -1.44 |
| Right ankle angle at heel strike | 0.78 | 0.287 | 0.526 | 0.654 | 0.201 | 1.358 |
| Right ankle angle at midstance at X axis | 0.943 | -0.0731 | 0.688 | 0.412 | 0.08 | 1.875 |
| Right ankle angle at midstance at Y axis | 0.951 | 0.063 | 0.686 | 0.415 | 0.154 | 1.529 |
As demonstrated in Table 2, the results showed three differences in cadence in both the barefoot-running shoe and barefoot-non-prescription orthotics phases, smaller cadence in non-prescription orthotics than running shoe. Also, there were significant differences in right foot step length among barefoot-running shoe and barefoot-non-prescription orthotics, higher step length in non-prescription orthotics than running shoe. And, there was significant differences in right foot stride length again in both the barefoot-running shoe and barefoot-orthotics, higher stride length in non-prescription orthotics than running she. Then, for right knee angle at toe-off our results showed significant difference just in barefoot-running shoe. Analysing the final t-test result and looking at mean (Table 1), it seems that the number of steps decreased in walking for non-prescription orthotics phase compared to cadence in barefoot walking. It seems as a logical result and can be supported more by the other two results from step length and stride length significant differences. Comparing the mean of running shoe and non-prescription orthotics, these 2 factors have increased compared to walking barefoot. As there is negative correlation between cadence and stride length, we can expect to have an increase in step length regarding decrease in cadence. To summarise, the cadence decreased by applying non-prescription orthotics, and both the stride length and stride length increased following applying non-prescription orthotics. However, there were no significant differences in comparing running shoe and non-prescription orthotics outcome results. Hence, we cannot confirm the efficiency of the non-prescription orthotics in this study.
5. Discussion
The results indicate significant differences in cadence, step length and stride length in both the running shoe and non-prescription orthotics group. But there were not any significant differences between running shoe and non-prescription orthotics for all three results. Here, one question comes up. Can we accept the differences in orthotics group as the effect streaming from non-prescription orthotics? In other words, if the non-prescription orthotics could make a significant difference in cadence, step length and stride length, then it was expected to find significant differences in comparing group of running shoe and non-prescription orthotics. Nowadays, most of running shoes are being design to provide customers with better comfort and safer condition in stand and motion position. Indeed, they are designed with anti-pronation features, such as: Cushioning, stiff counters and etc. But, despite non-prescription orthotics, overpronation treatment is not the main purpose of their production. Participants in this study suffered from overpronation. Non-prescription orthotics was applied in their shoes to see if it can make any changes as it promised. In terms of cadence, step length and stride length, non-prescription orthotics is not making any specific significant differences. However, there was a big SD around mean average age and big difference in their height in this study which showed the research has some limitations. In other words, all the cadence, step length and stride length are closely correlated with age, gender, height, body weight or body mass index. So, this difference between participants’ age can be the reason of not getting our expected important changes in non-prescription orthotics. However, from my point of view, more studies with bigger sample sizes and less distribution in age and body index should be done to answer this question better. Paired t test showed there was no significant difference in ankle angle at both the toe-off and heel strike. We know that age and speed are two important factors in angular changes in lower body joints such as ankle, knee, and the hip. So, this can be another factor for not seeing significant differences in our analysis.
Moreover, there is a positive correlation in gait speed and joint kinematics, joint kinetics, and ground reaction forces (18). Hence, we can assume participants did not walk fast enough to bring about the angular changes in the joints. To prevent this, instead of walking with self-selected speed, we would ask participants walk faster, say 60% - 70% their maximum heart rate, if we could do the experiment again. This assumption can be applied for hip angle and knee angle as well. Because they are being counted in this correlation. Reviewing survey results, nine participants out of twelve recorded that they had experienced changes by wearing non-prescription orthotics. All nine participants said that did feel more arch in their feet and more support during walking. Also, they announced that as a result of support increase, they could experience balance improvement during walking. But we could not find any non-prescription orthotics results to support their claims. If they had felt more arch support during walking, then it would be more logical if there were any changes in sagittal and horizontal plane at midstance for the ankle angle where body lack support and have one leg backing. It can be as a result of applying non-prescription orthotics for the short time. Non-prescription orthotics might not show us any immediate effect, because it has been announced any overpronation improvement takes time around 12 weeks and we should not expect immediate effect (19).
For right knee angle at toe-off test result, we found significant difference in running shoe phase. There were no significant changes in non-prescription and its comparing test with running shoe. This result indicates that for the running shoe condition could have made the knee angle at toe-off change compared to walking barefoot, and non-prescription orthotics. The mean value of the running shoe shows that it decreased knee flexion although running shoe has been on during walking with non-prescription orthotics, its data did not differ, and we did not get any significant differences following applying non-prescription orthotics. Apart from the above-mentioned reasons, it might be because the amount or degree of overpronation in participants in this study was not big enough to bring about any important changes. It seems that unlike other results, non-prescription orthotics destroyed the effect of running shoe for knee flexion. Because, all three differences in this study happened when running shoe was on. But it is just a hypothesis and may not be correct and have some other reason such as error in data. More studies should be done to help us understand better this result. There were some limitations in this study. First, our sample size was not big enough. We would have more reliable results if there were more volunteer participants in this study. Second, both the mean average age and height of participants, which are seen as important factors in our analysing factors, had much differences, and this might be one of the reasons to not having our predicted results. Because people with different age are not treating, walking same. In fact, we were limitation to have participants all with same gender, height and age. And, we could not provide all the participants with same running shoe. They all had their own running shoe with different style and features, such as: Different cushioning, length and flexibility. There were some errors in data. And, we had to do some events manually for all trials. Doing events manually can cause misjudged and impressed our final results.
Acknowledgements
References
-
1.
Okamoto H, Taniguchi H. Development of Pneumatic Exercise Device for the Range of Motion in the Ankle Joint. 2022 IEEE/SICE International Symposium on System Integration (SII). city of Narvik, Norway. IEEE; 2022. p. 585-9.
-
2.
Ghani NS, Abd Razak NA, Usman J, Gholizadeh H. Foot over Pronation Problem among Undergraduate Students: A Preliminary Study. Sains Malays. 2020;49(7):1651-62. https://doi.org/10.17576/jsm-2020-4907-16.
-
3.
Donatelli RA, Hurlburt C, Conaway D, St Pierre R. Biomechanical foot orthotics: a retrospective study. J Orthop Sports Phys Ther. 1988;10(6):205-12. [PubMed ID: 18796957]. https://doi.org/10.2519/jospt.1988.10.6.205.
-
4.
Tiberio D. Pathomechanics of structural foot deformities. Phys Ther. 1988;68(12):1840-9. [PubMed ID: 3194451]. https://doi.org/10.1093/ptj/68.12.1840.
-
5.
Stergiou N, Decker LM. Human movement variability, nonlinear dynamics, and pathology: is there a connection? Hum Mov Sci. 2011;30(5):869-88. [PubMed ID: 21802756]. [PubMed Central ID: PMC3183280]. https://doi.org/10.1016/j.humov.2011.06.002.
-
6.
Dahle LK, Mueller MJ, Delitto A, Diamond JE. Visual assessment of foot type and relationship of foot type to lower extremity injury. J Orthop Sports Phys Ther. 1991;14(2):70-4. [PubMed ID: 18796826]. https://doi.org/10.2519/jospt.1991.14.2.70.
-
7.
Bhuyan D, Kumar K; Information Resources Management Association (USA). A Brief History of Prosthetics and Orthotics of the Lower Body and Their Types. Research Anthology on Emerging Technologies and Ethical Implications in Human Enhancement. Hershey, USA: IGI Global; 2021. p. 365-80. https://doi.org/10.4018/978-1-7998-8050-9.ch018.
-
8.
Bennell KL, Bowles KA, Payne C, Cicuttini F, Williamson E, Forbes A, et al. Lateral wedge insoles for medial knee osteoarthritis: 12 month randomised controlled trial. BMJ. 2011;342:d2912. [PubMed ID: 21593096]. [PubMed Central ID: PMC3100910]. https://doi.org/10.1136/bmj.d2912.
-
9.
Collins N, Crossley K, Beller E, Darnell R, McPoil T, Vicenzino B. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. BMJ. 2008;337. a1735. [PubMed ID: 18952682]. [PubMed Central ID: PMC2572211]. https://doi.org/10.1136/bmj.a1735.
-
10.
Chapman C. Chairside orthoses—the end of casting. Podiatry Now. 1999;4.
-
11.
McCourt FJ. To cast or not to cast? The comparative effectiveness of casted and non-casted orthoses. The Chiropodist. 1990;45(12):239-43.
-
12.
Castro-Mendez A, Munuera PV, Albornoz-Cabello M. The short-term effect of custom-made foot orthoses in subjects with excessive foot pronation and lower back pain: a randomized, double-blinded, clinical trial. Prosthet Orthot Int. 2013;37(5):384-90. [PubMed ID: 23327838]. https://doi.org/10.1177/0309364612471370.
-
13.
Becerro de Bengoa Vallejo R, Sanchez Gomez R, Losa Iglesias ME. Clinical improvement in functional hallux limitus using a cut-out orthosis. Prosthet Orthot Int. 2016;40(2):215-23. [PubMed ID: 25261491]. https://doi.org/10.1177/0309364614550262.
-
14.
Holden MA, Callaghan M, Felson D, Birrell F, Nicholls E, Jowett S, et al. Clinical and cost-effectiveness of bracing in symptomatic knee osteoarthritis management: protocol for a multicentre, primary care, randomised, parallel-group, superiority trial. BMJ Open. 2021;11(3). e048196. [PubMed ID: 33771832]. [PubMed Central ID: PMC8006841]. https://doi.org/10.1136/bmjopen-2020-048196.
-
15.
Genova JM, Gross MT. Effect of foot orthotics on calcaneal eversion during standing and treadmill walking for subjects with abnormal pronation. J Orthop Sports Phys Ther. 2000;30(11):664-75. [PubMed ID: 11104377]. https://doi.org/10.2519/jospt.2000.30.11.664.
-
16.
Wong L, Hunt A, Burns J, Crosbie J. Effect of foot morphology on center-of-pressure excursion during barefoot walking. J Am Podiatr Med Assoc. 2008;98(2):112-7. [PubMed ID: 18347119]. https://doi.org/10.7547/0980112.
-
17.
Branthwaite HR, Payton CJ, Chockalingam N. The effect of simple insoles on three-dimensional foot motion during normal walking. Clin Biomech (Bristol, Avon). 2004;19(9):972-7. [PubMed ID: 15475131]. https://doi.org/10.1016/j.clinbiomech.2004.06.009.
-
18.
Fukuchi CA, Fukuchi RK, Duarte M. Effects of walking speed on gait biomechanics in healthy participants: a systematic review and meta-analysis. Syst Rev. 2019;8(1):153. [PubMed ID: 31248456]. [PubMed Central ID: PMC6595586]. https://doi.org/10.1186/s13643-019-1063-z.
-
19.
Mendes A, Silva HJA, Costa ARA, Pinheiro YT, Lins CAA, de Souza MC. Main types of insoles described in the literature and their applicability for musculoskeletal disorders of the lower limbs: A systematic review of clinical studies. J Bodyw Mov Ther. 2020;24(4):29-36. [PubMed ID: 33218525]. https://doi.org/10.1016/j.jbmt.2020.06.001.
