Abstract
Background:
Sporting activity promotes healthy living, increases health benefits, mitigates some chronic disease conditions and prevents premature death. Cardiovascular disease risks during sports activities and exercises are low but in some instances of undiagnosed pathological cardiac conditions, players could be at the risk of tragic cardiovascular events.Objectives:
The aim of the study was to determine the prevalence of high blood pressure, abnormal fasting blood sugar and lipid profiles, as probable cardiovascular disease risk factors among male soccer players.Methods:
A cross-sectional study was used and 86 football players of the premier, 1st and 2nd divisions’ teams were used for the study. The blood pressure and biochemical markers such as fasting blood glucose and lipid profiles of the players were assessed.Results:
Out of the 86 players, 8 (9.3%) were goalkeepers, 29 (33.7%) were defenders, 34 (39.5%) were midfielders, while 15 (17.4%) were strikers. The prevalence of hypertension and diabetes among the study population were 9.3% each. The most prevalent abnormality was reduced high density lipoprotein (38.4%), followed by hypercholesterolemia (27.9%) and (7.0%) high low density lipoprotein respectively.Conclusions:
The incidence of high blood pressure, high blood glucose, reduced high density lipoprotein and hypercholesterolemia observed in the study indicate that the players are at increased risks of cardiovascular diseases.Keywords
Cardiovascular Disease Blood Pressure Fasting Plasma Glucose Lipid Profiles Football Players
1. Background
Physical activity promotes healthy living and prevents premature death. It provides increased benefits of health in individuals and can mitigate some chronic disease conditions (1). Several benefits can be derived from physical activity and regular exercise. For example, according to Stern et al. (2), cardiovascular disease risks during sports activities and exercises are low but in some instances of athletes who have undiagnosed pathological cardiac conditions, they could be at the mercy of tragic cardiovascular events (3).
According to Harmon et al. (4), there has been increasing prevalence of sudden cardiac death and it was the primary contributory factor to death among student athletes of the National Collegiate Athletic Association in the United States (4). Even though athletes are physically active, the preventive measures against the incidence of cardiovascular diseases do not rely on physical activity alone (5).
Lipids perform important functions in the body. In spite of their enormous contributions to the functions of the body, abnormally high levels of lipids and their lipoprotein carriers in the blood contribute greatly to the development of atherosclerosis (6). Lipid profiles of athletes should be such that they are likely to reduce the occurrence of atherosclerotic cardiovascular disease (ASCVD) (7, 8). In general, compared to their sedentary counterparts, athletes have a 40% - 50% higher HDL-C, 5% - 10% lower LDL-C and a 20% - 40% lower TG, with a lower prevalence of hypercholesterolemia (total cholesterol > 200 mg/dL) and hypertriglyceridemia (TG > 150 mg/dL) (9, 10).
Athletes, like football players and rugby players, endure intense physical training which frequently exceeds the energy expenditure requirements which is normally recognized to alter lipids and lipoproteins. According to Durstine et al. (7), a relationship exists between the training intensity and blood lipids. This implies that exercising at low training volume can significantly change blood lipids levels (7). Even though athletes undergo intense level of physical exercise with significant effect on lipid and lipoprotein carriers, evidence from a number of studies have reported an increase in CVD risks associated with dyslipidemia (7, 11, 12).
2. Objectives
The main objective of this study was to determine the prevalence of high blood pressure and dyslipidemis, as cardiovascular disease risk factors, among male football players of some selected soccer clubs in the Ashanti region of Ghana. The specific objectives were to assess the biochemical markers (lipid profile and FBS) and blood pressure of the players.
3. Methods
3.1. Study Design
This research was a cross sectional study. The subjects of the study consisted of players in the Premier, First and Second divisions soccer teams.
3.2. Sample Size
A sample size of 86 football players was recruited from all the teams. A convenience sampling technique was used in selecting the players for the study. All players registered by the teams for the season were included in the study. Each team had at least 30 players who had registered for the season.
3.3. Ethical Approval
Ethical approval (CHRPE/AP/470/16) for the study was granted by the Committee on Human Research, Publications and Ethics (CHRPE), School of Medical Science, Kwame Nkrumah University of Science and Technology (KNUST). Permission was also sought from the management of the teams whose players participated in the study. A consent form was signed by each of the players who participated in the study before they were recruited for the study.
3.4. Inclusion and Exclusion Criteria
All players who were registered by the selected clubs for the league season were included in the study. Players, who agreed to allow their blood samples to be taken. Players, who were on trials but had not been registered by the clubs at the Ghana Football Association, were excluded from the study. Players who had eaten on the day of the data collection were also excluded.
3.5. Data Collection
Information on the demographic features and the positions of the players were collected, using a pre-tested questionnaire. The pre-test was to find out the relevance of the questions to be asked and to have a fair idea about the time to be used for answering the questionnaire.
3.6. Measurement of Biochemical Parameters
Five milliliters of fasting venous blood samples of study participants were taken around 7 am in the morning by a phlebotomist, through venipuncture. The blood samples collected were put into fluoride tubes and clot activator tubes. They were subsequently transported and analysed at the CanLab, KNUST for fasting blood glucose and the serum lipid profiles [triglycerides, total cholesterol, high density lipoprotein (HDL), and low density lipoproteins (LDL)]
3.7. Measurement of Blood Pressure
Players were asked to rest for 30 minutes prior to the measurement of the blood pressure. They were then asked to sit on a chair upright with the back straight and the feet flat on the floor. The blood pressure was measured with the Omron automatic blood pressure monitor (Model M2 Basic). The arm cuff was placed on the arm at the same level of the heart and then start/stop button was then pressed.
3.8. Data Analysis
Data collected were analyzed using Statistical Package for Social Sciences (SPSS), version 23 of IBM Corporation, United States. For continuous variables, mean and standard deviations were calculated, while percentages were calculated for categorical variables. ANOVA was used to compare the means of the players of particular teams and their biochemical data. A cross-tabulation analysis was also done to assess the players and their teams against their respective biochemical and anthropometry data. A P value of ≤ 0.05 was reckoned to be statistically significant.
4. Results
Eighty-six (86) players were recruited for the study. Out of the total number of players recruited, more than half of them (51.6%) were between 20 - 25 years. Majority of the players (40.0%) were also midfielders (Table 1). According to Table 2, Eight (8) of the players (9.3%) had hypertension, while 8 (9.3%) of the players were diabetics. More than a third of the players (38.4%) had lowered HDL levels, 27.9% of them had high TC, while 1 (1.2%) had a high TG and 7.0% of the players had high LDL.
Age Profile, Playing Positions and Teams of Players
| Variable | No. (%) |
|---|---|
| Age, y | |
| < 20 | 22 (25.6) |
| 20 -25 | 49 (51.6) |
| 26 - 30 | 15 (15.8) |
| Total | 86 (100.0) |
| Playing position | |
| Goalkeepers | 8 (9.3) |
| Defenders | 29 (33.7) |
| Midfielders | 34 (39.5) |
| Strikers | 15 (17.4) |
| Total | 86 (100) |
| Variable | No. (%) |
|---|---|
| Blood pressure, mmHg | |
| Normal | 58 (67.4) |
| Pre-hypertension | 20 (23.3) |
| Hypertension | 8 (9.3) |
| Total | 86 (100.0) |
| Fasting blood glucose | |
| Normal | 68 (79.1) |
| Prediabetes | 10 (11.6) |
| Diabetes | 8 (9.3) |
| Total | 86 (100.0) |
| Total cholesterol | |
| Normal | 62 (72.1) |
| High | 24 (27.9) |
| Total | 86 (100.0) |
| Triglycerides | |
| Normal | 85 (98.8) |
| High | 1 (1.2) |
| Total | 86 (100.0) |
| High density lipoproteins | |
| Low | 33 (38.4) |
| Optimal | 53 (61.6) |
| Total | 86 (100.0) |
| Low density lipoproteins | |
| Normal | 80 (93.0) |
| High | 6 (7.0) |
| Total | 86 (100.0) |
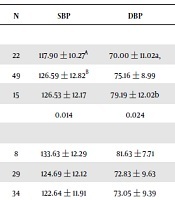
From Table 3, SBP did depend on age; 20 - 25 years’ age group had the highest SBP. DBP also increased with age; the highest mean DBP was found in the oldest age group. The mean FBS, TC and HDL did not show any difference, based on age and playing positions. The mean LDL was dependent on playing positions; defenders had the highest LDL and goalkeepers had the lowest. On the other hand, the mean TG was also dependent on playing positions; goalkeepers had the highest mean TG and Strikers had the lowest.
| N | SBP | DBP | FBS | TC | TG | HDL | LDL | |
|---|---|---|---|---|---|---|---|---|
| Age, y | ||||||||
| < 20 | 22 | 117.90 ± 10.27A | 70.00 ± 11.02a, | 6.10 ± 2.02 | 4.75 ± 0.86 | 0.74 ± 0.24 | 1.57 ± 0.26 | 2.80 ± 0.68 |
| 20 - 25 | 49 | 126.59 ± 12.82B | 75.16 ± 8.99 | 5.50 ± 1.20 | 4.60 ± 0.90 | 0.70 ± 0.19 | 1.53 ± 0.22 | 2.70 ± 0.81 |
| 26 - 30 | 15 | 126.53 ± 12.17 | 79.19 ± 12.02b | 5.55 ± 0.49 | 4.31 ± 0.81 | 0.81 ± 0.46 | 1.55 ± 0.24 | 2.35 ± 0.64 |
| P value | 0.014 | 0.024 | 0.215 | 0.318 | 0.412 | 0.853 | 0.185 | |
| Playing positions | ||||||||
| Goalkeepers | 8 | 133.63 ± 12.29 | 81.63 ± 7.71 | 5.40 ± 0.51 | 4.09 ± 0.73 | 1.03 ± 0.57A | 1.46 ± 0.12 | 2.11 ± 0.67A,C,D |
| Defenders | 29 | 124.69 ± 12.12 | 72.83 ± 9.63 | 5.99 ± 1.75 | 4.81 ± 0.80 | 0.69 ± 0.20B,C,D | 1.57 ± 0.19 | 2.88 ± 0.70B,C,D |
| Midfielders | 34 | 122.64 ± 11.91 | 73.05 ± 9.39 | 5.62 ± 1.40 | 4.69 ± 0.97 | 0.74 ± 0.22C,B,D | 1.58 ± 0.24 | 2.74 ± 0.84C,A,B,D |
| Strikers | 15 | 122.67 ± 11.64 | 77.47 ± 13.74 | 5.24 ± 0.51 | 4.22 ± 0.69 | 0.66 ± 0.15D,B,C | 1.50 ± 0.31 | 2.38 ± 0.52D,A,B,C |
| P value | 0.130 | 0.094 | 0.340 | 0.053 | 0.008 | 0.502 | 0.026 |
According to Table 4, whether a player would have high TG was dependent on playing positions; all players that had high TG were goalkeepers. Age and playing positions did not have any statistically significant effect on BP, FBS, TC, HDL and LDL.
Relationship Among Blood Pressure and Biochemical Markers and Age, Playing Positions and Teamsa
| Age, No. (%) | Playing Positions, No. (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| < 20 | 20 - 25 | 26 - 30 | P Value | GKS | DFDS | MDS | STKS | P Value | |
| Blood pressure | 0.070 | 0.086 | |||||||
| Normal | 20 (23.3) | 29 (33.7) | 9 (10.5) | 2 (2.3) | 21 (24.4) | 24 (27.9) | 11 (12.8) | ||
| Pre-hypertensive | 2 (2.3) | 13 (15.1) | 5 (5.8) | 5 (5.8) | 4 (4.7) | 7 (8.1) | 4 (4.7) | ||
| Hypertension | 0 (0.0) | 7 (8.1) | 1 (1.2) | 1 (1.2) | 4 (4.7) | 3 (3.5) | 0 (0.0) | ||
| FBS | 0.101 | 0.495 | |||||||
| Normal | 15 (17.4) | 41 (47.7) | 12 (14.0) | 7 (8.1) | 20 (23.3) | 27 (31.4) | 14 (16.3) | ||
| Pre-diabetes | 2 (2.3) | 5 (5.8) | 3 (3.5) | 1 (1.2) | 4 (4.7) | 4 (4.7) | 1 (1.2) | ||
| Diabetes | 5 (5.8) | 3 (3.5) | 0 (0.0) | 0 (0.0) | 5 (5.8) | 3 (3.5) | 0 (0.0) | ||
| TC | 0.130 | 0.107 | |||||||
| Normal | 15 (17.4) | 33 (38.4) | 14 (16.3) | 7 (8.1) | 18 (20.9) | 23 (26.7) | 14 (16.3) | ||
| High | 7 (8.1) | 16 (18.6) | 1 (1.2) | 1 (1.2) | 11 (12.8) | 11 (12.8) | 1 (1.2) | ||
| Triglyceride | 0.091 | 0.020 | |||||||
| Normal | 22 (25.6) | 49 (57.0) | 14 (16.3) | 7 (8.1) | 29 (33.7) | 34 (39.5) | 15 (17.4) | ||
| High | 0 (0.0) | 0 (0.0) | 1 (1.2) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| HDL | 0.171 | 0.248 | |||||||
| Low | 6 (7.0) | 23 (26.7) | 4 (4.7) | 3 (3.5) | 11 (12.8) | 10 (11.6) | 9 (10.5) | ||
| High | 16 (18.6) | 26 (30.2) | 11 (12.8) | 5 (5.8) | 18 (20.9) | 24 (27.9) | 6 (7.0) | ||
| LDL | 0.901 | 0.492 | |||||||
| Optimal | 20 (23.3) | 46 (53.5) | 14 (16.3) | 8 (9.3) | 26 (30.2) | 31 (36.0) | 15 (17.4) | ||
| High | 2 (2.3) | 3 (3.5) | 1 (1.2) | 0 (0.0) | 3 (3.5) | 3 (3.5) | 0 (0.0) | ||
5. Discussion
This study was aimed at finding how football players are predisposed to cardiovascular diseases, through the measurement of their lipid profiles, fasting blood glucose and blood pressure. It involved using some 86 players of four teams from the Ashanti region. It was a cross-sectional study in which anthropometric measurements of the players were done, blood pressure measured and blood samples taken to determine FBS and lipid profile.
Majority of players fell within the age range of 20 to 25 years. This was similar to a study by Abdulai (13), which reported that 58% of football players in the division 1 teams in Tamale, Ghana were between 20 - 29 years of age. This means that the players were young and have more playing days ahead of them in their career. For the players who were recruited, defenders and midfielders were the playing positions that were very dominant (constituting 71.6%). The high number of defenders and midfielders could be due to the traditional tactical approach (4-4-2) used by most of the football coaches in the country which make use of mainly midfielders and defenders.
The prevalence of hypertension among the players was 9.3%. This is a little higher than the 7% reported by Berge et al. (14), even though lower than the 13.8% and 19.2% reported by Tucker et al. (5), and Karpinos et al. (15), respectively. The high rate of hypertension among the players could be due to over-training and poor dietary intake. Over-training is thought to have a negative impact on the autonomic cardiovascular control (16). Overtraining results when there is an imbalance between training and competition and recovery. In Ghana, most teams train at least 3 hours a day and 5 times in a week. This could affect the heart muscles as they are not able to get enough recovery between their training and competition. The training and exercise routine of the players could mask the symptoms of hypertension which can lead to a sudden cardiac death on the field. Healthy dietary patterns are related to significant reduction in cardiovascular disease risks factors (17). Poor dietary pattern could increase their risk to cardiovascular diseases.
The prevalence rates of prediabetes and diabetes were 11.6% and 9.3% respectively. Hyperglycemia is one of the prevalent risk factor among the players who participated in the study. Chronic hyperglycemia destroys the endothelial cells of blood vessels which can further develop into atherosclerosis and increase the players’ risk of cardiovascular disease (18). This accounts for why some of the players may be susceptible to cardiovascular diseases. The high prevalence of prediabetes and diabetes among the players could be due to inadequacy of their dietary intake and bad dietary pattern. Lack of good nutritional knowledge and other bad lifestyle activities such as smoking and alcoholism could also be a reason why prediabetes and diabetes were found among the players.
The pattern of dyslipidemia in the players was as follows; 38.4% reduced HDL, 27.9% high levels of cholesterol and 1.2% of high triglyceride. Thus the two key components of the dyslipidemia among the players were reduced HDL and increased cholesterol. This was in contradiction to a study by de Araujo et al. (2012), which found prevalence of hypercholesterolemia (29.2%), hypertriglyceridemia (16.7%), low HDL (4.2%) and High LDL (20.8%) among football players in Brazil. Several investigations conducted have reported a relationship between hypertriglyceridemia and coronary artery disease (19, 20). Dyslipidemia is a major cardiovascular disease risk factor (21). The reduced HDL but increased levels of cholesterol are noteworthy, as these can contribute to atherosclerosis in the players. There is induction of inflammatory response and extensive vascular remodeling when plasma lipids are accumulated in the anterior intima. This results in the development of atherosclerotic plaques which increases the risk for cardiovascular diseases (22).
There was a direct association between age and both systolic and diastolic blood pressures. Players between the ages of 26 - 30 had a higher diastolic blood pressure, while those between the ages of 20 - 25 had a higher systolic blood pressure. This finding supports the work by Sharma (23), which reported that age affects the size of the heart muscles of athletes.
Total cholesterol and low density lipoprotein also have direct association with playing positions. It was also revealed that goalkeepers had a higher mean TG than the other playing positions. The difference in the lipid profiles of the players by their playing positions could be due to their personal lifestyle such as dietary intake.
5.1. Conclusions
In conclusion, high blood pressure, high blood glucose, reduced HDL and hypercholesterolemia may put the players at an increased risk of cardiovascular disease and hence football team managers and players should make conscious effort to check their blood pressures, fasting plasma glucoses and lipid profiles.
References
-
1.
Shiroma EJ, Lee IM. Physical activity and cardiovascular health: Lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. 2010;122(7):743-52. [PubMed ID: 20713909]. https://doi.org/10.1161/CIRCULATIONAHA.109.914721.
-
2.
Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, McKee AC. Long-term consequences of repetitive brain trauma: Chronic traumatic encephalopathy. PM R. 2011;3(10 Suppl 2):S460-7. [PubMed ID: 22035690]. https://doi.org/10.1016/j.pmrj.2011.08.008.
-
3.
Thompson PD, Franklin BA, Balady GJ, Blair SN, Corrado D, Estes NA 3rd, et al. Exercise and acute cardiovascular events placing the risks into perspective: A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation. 2007;115(17):2358-68. [PubMed ID: 17468391]. https://doi.org/10.1161/CIRCULATIONAHA.107.181485.
-
4.
Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in National Collegiate Athletic Association athletes. Circulation. 2011;123(15):1594-600. [PubMed ID: 21464047]. https://doi.org/10.1161/CIRCULATIONAHA.110.004622.
-
5.
Tucker AM, Vogel RA, Lincoln AE, Dunn RE, Ahrensfield DC, Allen TW, et al. Prevalence of cardiovascular disease risk factors among National Football League players. JAMA. 2009;301(20):2111-9. [PubMed ID: 19470988]. https://doi.org/10.1001/jama.2009.716.
-
6.
Leon AS, Bronas UG. Dyslipidemia and risk of coronary heart disease: Role of lifestyle approaches for its management. Am J Lifestyle Med. 2009;3(4):257-73. https://doi.org/10.1177/1559827609334518.
-
7.
Durstine JL, Grandjean PW, Davis PG, Ferguson MA, Alderson NL, DuBose KD. Blood lipid and lipoprotein adaptations to exercise: A quantitative analysis. Sports Med. 2001;31(15):1033-62. [PubMed ID: 11735685]. https://doi.org/10.2165/00007256-200131150-00002.
-
8.
Srinath Reddy K, Katan MB. Diet, nutrition and the prevention of hypertension and cardiovascular diseases. Public Health Nutr. 2004;7(1A):167-86. [PubMed ID: 14972059].
-
9.
Thompson PD, Cullinane E, Henderson LO, Herbert PN. Acute effects of prolonged exercise on serum lipids. Metabolism. 1980;29(7):662-5. [PubMed ID: 7382830]. https://doi.org/10.1016/0026-0495(80)90111-0.
-
10.
Deshaies Y, Allard C. Serum high-density lipoprotein cholesterol in male and female Olympic athletes. Med Sci Sports Exerc. 1982;14(3):207-11. [PubMed ID: 7109888].
-
11.
Buell JL, Calland D, Hanks F, Johnston B, Pester B, Sweeney R, et al. Presence of metabolic syndrome in football linemen. J Athl Train. 2008;43(6):608-16. [PubMed ID: 19030139]. [PubMed Central ID: PMC2582553]. https://doi.org/10.4085/1062-6050-43.6.608.
-
12.
Chang AY, FitzGerald SJ, Cannaday J, Zhang S, Patel A, Palmer MD, et al. Cardiovascular risk factors and coronary atherosclerosis in retired National Football League players. Am J Cardiol. 2009;104(6):805-11. [PubMed ID: 19733715]. [PubMed Central ID: PMC3733174]. https://doi.org/10.1016/j.amjcard.2009.05.008.
-
13.
Abdulai K. Assessment of nutritional status and dietary behaviour of division one league footballers in tamale metropolis. University of Ghana; 2015, [cited 21/08/2017]. Available from: http://ugspace.ug.edu.gh.
-
14.
Berge HM, Gjerdalen GF, Andersen TE, Solberg EE, Steine K. Blood pressure in professional male football players in Norway. J Hypertens. 2013;31(4):672-9. [PubMed ID: 23442990]. https://doi.org/10.1097/HJH.0b013e32835eb5fe.
-
15.
Karpinos AR, Roumie CL, Nian H, Diamond AB, Rothman RL. High prevalence of hypertension among collegiate football athletes. Circ Cardiovasc Qual Outcomes. 2013;6(6):716-23. [PubMed ID: 24221829]. [PubMed Central ID: PMC3975920]. https://doi.org/10.1161/CIRCOUTCOMES.113.000463.
-
16.
Baumert M, Brechtel L, Lock J, Hermsdorf M, Wolff R, Baier V, et al. Heart rate variability, blood pressure variability, and baroreflex sensitivity in overtrained athletes. Clin J Sport Med. 2006;16(5):412-7. [PubMed ID: 17016118]. https://doi.org/10.1097/01.jsm.0000244610.34594.07.
-
17.
American Heart Association Nutrition Committee, Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, et al. Diet and lifestyle recommendations revision 2006: A scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006;114(1):82-96. [PubMed ID: 16785338]. https://doi.org/10.1161/CIRCULATIONAHA.106.176158.
-
18.
Bhutto MG, Lokesh MR, Shah SKD, Afroze MKH, Ghouse P, Abhilash D. Association between lipid profile and silent coronary artery disease in south indian patients with type 2 diabetes mellitus. Int J Adv Med. 2017;4(1):1.
-
19.
Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation. 2007;115(4):450-8. [PubMed ID: 17190864]. https://doi.org/10.1161/CIRCULATIONAHA.106.637793.
-
20.
Shai I, Rimm EB, Hankinson SE, Curhan G, Manson JE, Rifai N, et al. Multivariate assessment of lipid parameters as predictors of coronary heart disease among postmenopausal women: potential implications for clinical guidelines. Circulation. 2004;110(18):2824-30. [PubMed ID: 15492318]. https://doi.org/10.1161/01.CIR.0000146339.57154.9B.
-
21.
Porez G, Prawitt J, Gross B, Staels B. Bile acid receptors as targets for the treatment of dyslipidemia and cardiovascular disease. J Lipid Res. 2012;53(9):1723-37. [PubMed ID: 22550135]. [PubMed Central ID: PMC3413216]. https://doi.org/10.1194/jlr.R024794.
-
22.
Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473(7347):317-25. [PubMed ID: 21593864]. https://doi.org/10.1038/nature10146.
-
23.
Sharma S. Athlete's heart--effect of age, sex, ethnicity and sporting discipline. Exp Physiol. 2003;88(5):665-9. [PubMed ID: 12955167].