Abstract
Background:
As the coronavirus disease 2019 (COVID-19) epidemic continues to spread, it is important to predict the clinical classification of COVID-19 and evaluate the progression of lung injury.Objectives:
To investigate the predictive factors of the outcome of moderate-stage coronavirus disease 2019 (COVID-19) and maximal extent of lung injury.Patients and Methods:
This study was a retrospective analysis of 97 patients with moderate-stage COVID-19 diagnosed in our hospital. We divided the patients into two groups according to disease progression: one group for moderate stage and another for both severe stage and critically severe stage COVID-19. We then analyzed the independent factors influencing changes in the course of the disease in moderate-stage patients using binary logistic regression. Next, we assessed the computed tomography (CT) score of maximal lung injury using follow-up images of the patients. We used multiple linear regression (MLR) to analyze the independent variables, and to predict the CT score of maximal lung injury in COVID-19 patients.Results:
The results were obtained using multivariate logistic regression analysis, and the independent factors affecting clinical classification were baseline CT score (P = 0.008), high-sensitivity C-reactive protein (hs-CRP) (P = 0.001), and diabetes (P = 0.04). MLR revealed that the factors predicting the extent of maximal lung injury in COVID-19 patients were age (P = 0.014), neutrophil percentage (P = 0.038), lymphocyte percentage (P = 0.031), hs-CRP (P = 0.010), and baseline CT score (P < 0.001). The optimal cut-off value of hs-CRP was 18.5, and the baseline CT score was 8.5.Conclusion:
Age, baseline CT score, hs-CRP, neutrophil percentage, and lymphocyte percentage could predict the CT score of maximal lung injury, and hs-CRP > 18.5, baseline CT score ≥ 9, and diabetes were independent factors of severe/critically severe COVID-19.Keywords
COVID-19 Acute Lung Injury Diabetes Mellitus C-Reactive Protein
1. Background
COVID-19 is an infectious disease that first broke out in Wuhan, China in 2019. It has presented a great threat to global public health due to its rapid spread and large-scale outbreaks worldwide. For newly confirmed COVID-19 patients, it is particularly important to determine which patients are prone to developing severe or critically severe disease.
2. Objectives
This study aims to predict and evaluate the maximal extent of lung injury and eventual clinical classification of COVID-19 patients from the baseline data of admitted patients in order to provide guidance for clinical treatment.
3. Patients and Methods
3.1. Patients
This study was approved by the local institutional review board (code: LW2020024). It is a retrospective analysis of 97 cases of moderate-stage COVID-19 admitted to our hospital from January to March 2020.
Case inclusion criteria were as follows: (1) A diagnostic tool indicated a positive nucleic acid result for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) under real-time fluorescence reverse transcription polymerase chain reaction (RT-PCR); (2) the patient was an inpatient making his/her first visit because of COVID-19; (3) the patient was in the moderate stage of COVID-19 as defined using clinical classification criteria; (4) the patient had complete CT follow-up images and laboratory data.
Exclusion criteria were as follows: (1) The patient had mild, severe, or critically severe-stage COVID-19 upon admission; (2) the patient had any other serious illness at the time of admission; (3) the patient had incomplete imaging or laboratory data.
Patients were clinically classified according to the Diagnosis and Treatment Plan of Coronavirus Disease 2019 (trial edition 7) issued by the National Health Commission of the Peoples Republic of China (1). Clinical stages were divided into four groups according to the following criteria. Mild stage: the clinical symptoms are mild, and imaging shows no manifestations of pneumonia. Moderate stage: patients have symptoms such as fever and respiratory tract symptoms, and pneumonia manifestations can be seen on imaging. Severe stage: patients show signs of respiratory distress, including respiratory rate ≥ 30 breaths/min, pulse oxygen saturation (SpO2) ≤ 93% on room air in the resting state, or arterial partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) ≤ 300 mmHg. At higher altitudes (above 1 km), PaO2/FiO2 values should be adjusted based on the equation PaO2/FiO2 × [atmospheric pressure (mmHg)/760], and patients with > 50% lesion progression within 24 h to 48 h as shown by pulmonary imaging should be treated as severe cases. Critically severe stage: respiratory failure occurs, and mechanical ventilation is required; shock occurs; and condition is complicated with other organ failure that requires monitoring and treatment in the intensive care unit (ICU).
During hospitalization, patients with moderate-stage COVID-19 who had not undergone any change in clinical classification were included in the moderate-stage group, while those who had passed into the severe or critically severe stage were included in the severe and critically severe group.
3.2. CT Examination
The Toshiba Aquilion One Vision 320-detecter row computed tomography (CT) Scanner (Toshiba Medical Systems, Otawara-shi, Japan) was chosen for screening, and the scanning parameters were as follows: collimator width 320 × 0.5 mm, tube voltage 120 kVp, current 200 mAs, slice thickness 5 mm, matrix 512 × 512, and interval 2 mm. The scanning range was continuous from the lung apex to the costophrenic angle.
3.3. Imaging Analysis
All of the CT images were analyzed independently by two radiologists with more than 10 years of experience, and agreement was obtained through discussion and negotiation when opinions differed. Baseline CT features included ground-glass opacity (GGO), consolidation, subpleural lines, crazy-paving pattern, reticular shadow, pleural thickening, and pleural effusion.
The semi-quantitative scores of chest CT were determined as follows (2). The lungs were divided into six areas, in which the upper and middle areas were bounded by the tracheal carina, and the middle and lower areas were bounded by the lower pulmonary veins. Each area was scored using the five-grade method according to the extent of the lesion, as follows: 0: normal lung tissue, (1) the extent of the lesion was < 25% of the area; (2) the extent of the lesion was 25% - 50% of the area, 3: the extent of the lesion was 50% - 75% of the area, and 4: the extent of the lesion was greater than 75% of the area. Then, the scores of the six areas were added to obtain the patients CT score. The baseline CT score was a semi-quantitative CT score of the first CT performed on admission, and the CT image with the most severe degree of intrapulmonary disease was selected as the CT score of maximal lung injury.
3.4. Laboratory Examinations
Laboratory examinations were obtained from patients upon admission, and fasting peripheral blood, which was venous blood containing anticoagulants (EDTA-K2), and was drawn from study subjects in the morning. Peripheral white blood cell count (WBC), neutrophil count, neutrophil percentage, monocyte count, monocyte percentage, lymphocyte count, lymphocyte percentage, red blood cell count (RBC), platelet count (PLT), and high-sensitivity C-reactive protein (hs-CRP) were measured using an automatic hematology analyzer.
3.5. Statistical Analysis
SPSS 19.0 software (IBM Corp. Released 2010 IBM SPSS Statistics for Windows version 19.0 Armonk, NY: IBM Corp) was used for statistical analysis. Means and standard deviations were used to describe the measurement data that conformed to a normal distribution, and two independent sample t-tests were used for comparisons between groups. Medians and quartiles were used to describe the measurement data that did not conform to a normal distribution, and non-parametric tests (such as the Mann-Whitney U-test) were used for comparison between groups. Frequencies and percentages were used for enumeration data, and chi-square tests were used for comparisons between groups. Multivariate logistic regression was used to analyze the factors influencing clinical classification (moderate stage or severe/critically severe stage). Using the CT score of maximal lung injury as the dependent variable, baseline data were used as the independent variables. Multiple linear regression (MLR) was used to analyze the factors related to the CT score of maximal lung injury. The optimal cut-off value of significant factors was obtained using a receiver operating characteristic (ROC) curve, and a P-value of < 0.05 was defined as statistically significant.
4. Results
All 97 patients included in this study were admitted to the hospital. The participants in the moderate-stage group had an age range of 57.69 ± 17.62. During hospitalization, 53 patients (54.6%) showed no deterioration in their conditions, 27 patients (27.8%) entered the severe stage of COVID-19, and 17 patients (17.5%) entered the critically severe stage. Fifty-three patients (54.6%) consisting of 23 males and 30 females with an average age of 52.25 ± 16.8 years remained classified as the moderate-stage group, and 44 cases (45.3%) made up of 29 males and 15 females with an average age of 64.25 ± 16.4 years were reclassified as the severe and critically severe group.
The baseline data of the patients were analyzed by single-factor analysis. Significant indicators in univariate analysis were age, gender, white blood cell count, neutrophil count, monocyte percentage, lymphocyte percentage, neutrophil percentage, hs-CRP, consolidation, crazy-paving pattern, reticular shadow, pleural effusion, diabetes, and baseline CT score (P < 0.05) (Table 1). Multivariate logistic regression analysis was performed using the stepwise method (forward: LR) with moderate-stage and severe or critically severe-stage COVID-19 as the dependent variables. Independent factors affecting clinical classification were hs-CRP (P = 0.01), baseline CT score (P = 0.008), and diabetes (P = 0.044) (Table 2).
| Moderate stage (n = 53) | Severe/critically severe stage (n = 44) | P | |
|---|---|---|---|
| Age | 52.25 ± 16.80 | 64.25 ± 16.46 | 0.001 |
| Baseline temperature | 37.51 ± 0.89 | 37.62 ± 0.85 | 0.300 |
| Sex (male) | 23 (43.39) | 29 (65.91) | 0.027 |
| Diabetes | 2 (3.77) | 9 (20.45) | 0.010 |
| Hypertension | 17 (32.07) | 22 (50.0) | 0.073 |
| RBC, ×1012/L | 4.16 ± 0.51 | 4.10 ± 0.60 | 0.576 |
| PLT, ×109/L | 159.51 ± 59.48 | 158.52 ± 81.56 | 0.945 |
| White blood cell count, ×109/L | 4.68 ± 1.88 | 6.02 ± 2.57 | 0.004 |
| Monocyte count, ×109/L | 0.67 ± 1.21 | 0.69 ± 0.97 | 0.929 |
| Lymphocyte count, ×109/L | 1.19 ± 0.41 | 1.02 ± 1.18 | 0.323 |
| Monocyte percentage, % | 11.66 ± 3.76 | 9.81 ± 4.06 | 0.022 |
| Lymphocyte percentage, % | 27.59 ± 10.52 | 18.9 ± 15.08 | 0.001 |
| Neutrophil percentage, % | 59.02 ± 13.68 | 70.18 ± 16.69 | 0.000 |
| Neutrophil count, ×109/L | 2.93 ± 1.84 | 4.39 ± 2.47 | 0.001 |
| hs-CRP, mg/L | 12.16 ± 11.76 | 24.05 ± 9.78 | 0.000 |
| Baseline CT score | 3 (1,6) | 9 (4,14.75) | 0.000 |
| GGO | 44 (83.01) | 38 (86.36) | 0.650 |
| Consolidation | 24 (45.28) | 29 (65.91) | 0.042 |
| Reticular shadow | 16 (30.18) | 22 (50) | 0.047 |
| Crazy-paving pattern | 13 (24.52) | 20 (45.45) | 0.03 |
| Subpleural line | 28 (52.83) | 24 (54.54) | 0.866 |
| Pleural effusion | 2 (3.77) | 7 (15.91) | 0.040 |
| Pleural thickening | 6 (11.32) | 9 (20.45) | 0.215 |
Multivariate Logistic Regression Analysis of Baseline Data and Outcomes for Moderate-Stage COVID-19
| B coefficient | SE | Exp (B) | 95% CI for Exp (B) | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Baseline CT score | 0.122 | 0.046 | 1.130 | 1.033 | 1.235 |
| hs-CRP, mg/L | 0.075 | 0.022 | 1.078 | 1.032 | 1.235 |
| Diabetes | 1.903 | 0.925 | 6.707 | 1.095 | 41.080 |
The disease course ranged from 10 to 47 days, and patients with COVID-19 underwent an average of five CT examinations. We assessed the baseline CT score and the CT score of maximal lung injury (Figure 1). Using the CT score of maximal lung injury as the dependent variable, for which the median was 10 and the interquartile range was (6, 18.5), and baseline data as the independent variable, MLR revealed that age, neutrophil percentage, lymphocyte percentage, hs-CRP, and baseline CT score were statistically significant for the CT score of maximal lung injury (P < 0.05). Among these factors, age, hs-CRP, and baseline score were positively correlated with the CT score of maximal lung injury, with B coefficients of 0.081, 0.129, and 0.407, respectively, while lymphocyte and neutrophil percentages were negatively correlated with dependent variable scores, with B coefficients of -0.125 and -0.124, respectively (Table 3). Based on these results, we wrote a model equation: CT score of maximal lung injury = 13.463 + 0.081 × age - 0.125 × lymphocyte percentage - 0.124 × neutrophil percentage + 0.129 × hs-CRP + 0.407 × baseline CT score. The significance test of the regression equation was as follows: F = 11.92, P < 0.001, multiple correlation coefficient R = 0.743, and adjusted R2 = 0.552.
CT scans of a 89-year-old female COVID-19 patient with type I respiratory failure. A-C, CT at first diagnosis shows scattered patches and nodular ground glass shadows in both lungs; baseline CT score of 9; D-F, Follow-up CT five days later shows that the lesion range has increased, partial lesion consolidation has occurred, and solid nodules are visible; CT score of maximal lung injury of 17.
. Multiple Linear Regression Analysis of Baseline Data and CT Score of Maximal Lung Injury
| Unstandardized coefficients | 95% CI for EXP(B) | |||
|---|---|---|---|---|
| B coefficient | SE | Lower | Upper | |
| Age | 0.081 | 0.033 | 0.017 | 0.146 |
| Lymphocyte percentage | -0.125 | 0.057 | -0.239 | -0.012 |
| Neutrophil percentage, % | -0.124 | 0.059 | -0.241 | -0.007 |
| hs-CRP | 0.129 | 0.049 | 0.032 | 0.226 |
| Baseline CT score | 0.407 | 0.092 | 0.223 | 0.590 |
According to ROC curve analysis of baseline CT score versus clinical classification, the area under the curve (AUC) was 0.762, the AUC of hs-CRP versus clinical classification was 0.778, the optimal cut-off value for hs-CRP was 18.5, and the optimal cut-off value for baseline CT score was 8.5 (Figure 2 and Table 4).
ROC curves Analysis of hs-CRP and baseline CT score as predictors for the progression of moderate-stage COVID-19 to severe/critically severe-stage. The results showed that hs-CRP (AUC = 0.778, P < 0.001) and baseline CT score (AUC = 0.762, P < 0.001) could well predict the progression of moderate-stage to severe/critically severe-stage.
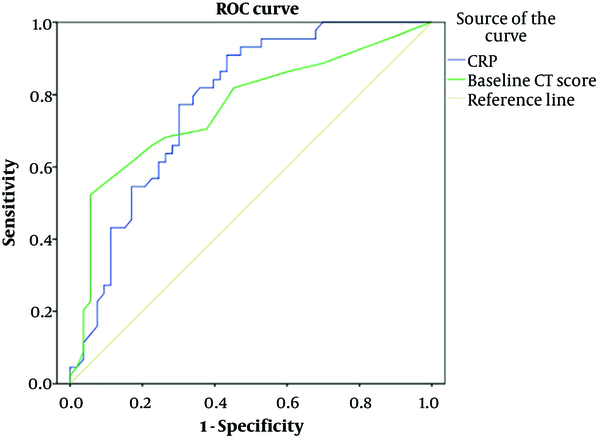
Receiver operating characteristic (ROC) Curve analysis of high-sensitivity C-reactive protein (hs-CRP) and CT Score Cut-Off Value of Severe and Critically Severe-Stage COVID-19
| AUC (95% CI) | Best cutoff value | Sensitivity, % | Specificity, % | |
|---|---|---|---|---|
| Baseline CT score | 0.762 | 8.5 | 52.30 | 99.43 |
| hs-CRP, mg/L | 0.778 | 18.5 | 77.30 | 67.80 |
5. Discussion
Patients with COVID-19 can be divided into four stages: early stage, progressive stage, peak stage, and absorption stage, according to chest CT findings (3). CT scans mainly show single or multiple localized ground-glass opacities and nodules in the early stage. In the progressive stage, new ground-glass lesions and progressive solid lesions coexist. In the peak stage, diffuse consolidation of the lesion occurs, and some patients present with a white lung. In the absorption stage, the lesion is gradually absorbed and dissipated, and some lesions can become fibrotic. For severe and critically severe-stage patients, the extent of tissue injury in lung CT may be greater at initial diagnosis, and interstitial lesions will occur more frequently than in moderate-stage patients (4). Most patients with COVID-19 infection have typical imaging characteristics, and imaging examination plays an important role in monitoring treatment effect, diagnosis, and disease progression (5). In terms of laboratory tests, severe and critically severe-stage patients mostly present with lower levels of lymphocytes, albumin, and serum sodium, and higher levels of total bilirubin, creatine kinase, lactate dehydrogenase, and hs-CRP (6). For most mild and moderate-stage patients, some indicators, such as blood routine and biochemical indicators, may be within the normal range at the time of initial diagnosis. Monitoring the patients’ laboratory parameters is equally helpful for clinical diagnosis and classification because these tests could be used to make a rough predictive assessment of the patients’ disease development at the time of initial diagnosis.
Semi-quantitative CT scoring of the maximum extent of lung injury was performed for 97 COVID-19 patients in this study, and the independent predictors of the maximum range of lung injury were evaluated by MLR. MLR analysis revealed that age, baseline CT score, hs-CRP, neutrophil percentage, and lymphocyte percentage had statistical significance. Age was positively correlated with the maximum range of lung injury, the older the patient, the greater the range of lung injury may be at the peak stage. Some studies have found that older age is associated with ICU admission and death (7). Additionally, there was a positive correlation between hs-CRP and the maximal extent of lung injury during follow-up in our study; hs-CRP was a non-specific marker in the acute phase of systemic inflammatory response, which could rapidly increase in the presence of infection. Some studies have found that there is a significant positive correlation between the CT score and hs-CRP (8). Our study further found that baseline hs-CRP could be used to predict the CT score of maximal lung injury. There was a positive correlation between baseline CT score and CT score of maximal lung injury. A higher baseline CT score may be associated with a faster progression of the range of pneumonia lesions, leading to a greater range of lung injury. Baseline neutrophil percentage and baseline lymphocyte percentage were negatively correlated with the maximal extent of lung injury by MLR, and this result was consistent with the study conducted by Liu et al. (9), which used correlation analysis to find that the lymphocyte and neutrophil percentages in blood samples from COVID-19 patients were highly correlated with the patients’ Murray score of lung injury. Furthermore, our study found that the maximal lung injury CT score could be predicted using the baseline neutrophil and lymphocyte percentages.
In this study, the clinical prognoses of 97 patients with moderate-stage COVID-19 were analyzed, and independent risk factors for the progression of moderate-stage to severe/critically severe-stage disease were evaluated. Results showed that hs-CRP > 18.5, baseline CT score ≥ 9, and diabetes could predict which patients would enter the severe stage or critically severe stage reasonably well. This study shows that diabetes is associated with a poor outcome for moderate-stage COVID-19. Long-term hyperglycemia in diabetic patients can lead to decreased immune function and other complications. COVID-19 patients with diabetes are more likely develop severe infection. Furthermore, meta-analysis revealed that diabetes was one of the major clinical risk factors for severe or fatal outcomes associated with COVID-19 (10). Thus, it is particularly important to improve the corresponding CT and laboratory examinations performed upon admission. The CT scores of COVID-19 pneumonia patients in the severe and critically severe disease stages were higher than the scores of patients in the moderate stage (11). Some studies calculated the percentage of whole lung volume occupied by lesions using an artificial intelligence (AI) platform, and they found that the volume percentage of pneumonia lesions for the whole lung for the diagnosis of severe/critical stage COVID-19 had high sensitivity and specificity (12). Although the AI algorithm is more accurate, the CT score is more clinically operable, and can be widely used in primary hospitals. hs-CRP elevation were independent significant predictors of COVID-19 severity, and this result was consistent with the study by Villard et al. (13). COVID-19 progresses rapidly, and patients with a baseline CT score ≥ 9, hs-CRP > 18.5, and diabetes should be closely observed for changes in condition to ensure timely response to possible deterioration.
The limitations of this study are as follows. (1) This study is a single-center, small-sample study, with inherent deficiencies; (2) patient selection was retrospective; therefore, the collected data could have selection bias.
In summary, the maximal extent of lung injury in COVID-19 patients was found in this study to be related to baseline CT score, hs-CRP, age, and neutrophil percentage. Multivariate logistic regression analysis of severe-stage and critically severe-stage patients found that hs-CRP > 18.5, baseline CT score ≥ 9, and diabetes were independent factors for severe and critically severe-stage disease. In conclusion, the condition of patients with COVID-19 pneumonia develops rapidly, and the maximal extent of lung injury and clinical classification of patients could be predicted by CT examination and laboratory examination of newly diagnosed patients, providing guidance for clinical treatment.
References
-
1.
National Health Commission of the People's Republic of China. Diagnosis and treatment of novel coronavirus. 2020. Available from: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml.
-
2.
Casarini M, Ameglio F, Alemanno L, Zangrilli P, Mattia P, Paone G, et al. Cytokine levels correlate with a radiologic score in active pulmonary tuberculosis. Am J Respir Crit Care Med. 1999;159(1):143-8. [PubMed ID: 9872832]. https://doi.org/10.1164/ajrccm.159.1.9803066.
-
3.
Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020;295(3):715-21. [PubMed ID: 32053470]. [PubMed Central ID: PMC7233367]. https://doi.org/10.1148/radiol.2020200370.
-
4.
Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. AJR Am J Roentgenol. 2020;214(5):1072-7. [PubMed ID: 32125873]. https://doi.org/10.2214/AJR.20.22976.
-
5.
Li B, Li X, Wang Y, Han Y, Wang Y, Wang C, et al. Diagnostic value and key features of computed tomography in Coronavirus Disease 2019. Emerg Microbes Infect. 2020;9(1):787-93. [PubMed ID: 32241244]. [PubMed Central ID: PMC7191895]. https://doi.org/10.1080/22221751.2020.1750307.
-
6.
Zhang X, Cai H, Hu J, Lian J, Gu J, Zhang S, et al. Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int J Infect Dis. 2020;94:81-7. [PubMed ID: 32205284]. [PubMed Central ID: PMC7270493]. https://doi.org/10.1016/j.ijid.2020.03.040.
-
7.
Henderson LA, Canna SW, Schulert GS, Volpi S, Lee PY, Kernan KF, et al. On the Alert for Cytokine Storm: Immunopathology in COVID-19. Arthritis Rheumatol. 2020;72(7):1059-63. [PubMed ID: 32293098]. [PubMed Central ID: PMC7262347]. https://doi.org/10.1002/art.41285.
-
8.
Sun D, Li X, Guo D, Wu L, Chen T, Fang Z, et al. CT Quantitative Analysis and Its Relationship with Clinical Features for Assessing the Severity of Patients with COVID-19. Korean J Radiol. 2020;21(7):859-68. [PubMed ID: 32524786]. [PubMed Central ID: PMC7289692]. https://doi.org/10.3348/kjr.2020.0293.
-
9.
Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63(3):364-74. [PubMed ID: 32048163]. [PubMed Central ID: PMC7088566]. https://doi.org/10.1007/s11427-020-1643-8.
-
10.
Liu H, Chen S, Liu M, Nie H, Lu H. Comorbid Chronic Diseases are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis. Aging Dis. 2020;11(3):668-78. [PubMed ID: 32489711]. [PubMed Central ID: PMC7220287]. https://doi.org/10.14336/AD.2020.0502.
-
11.
Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, et al. The Clinical and Chest CT Features Associated With Severe and Critical COVID-19 Pneumonia. Invest Radiol. 2020;55(6):327-31. [PubMed ID: 32118615]. [PubMed Central ID: PMC7147273]. https://doi.org/10.1097/RLI.0000000000000672.
-
12.
Ren HW, Wu Y, Dong JH, An WM, Yan T, Liu Y, et al. Analysis of clinical features and imaging signs of COVID-19 with the assistance of artificial intelligence. Eur Rev Med Pharmacol Sci. 2020;24(15):8210-8. [PubMed ID: 32767351]. https://doi.org/10.26355/eurrev_202008_22510.
-
13.
Villard O, Morquin D, Molinari N, Raingeard I, Nagot N, Cristol JP, et al. The Plasmatic Aldosterone and C-Reactive Protein Levels, and the Severity of Covid-19: The Dyhor-19 Study. J Clin Med. 2020;9(7). [PubMed ID: 32708205]. [PubMed Central ID: PMC7408691]. https://doi.org/10.3390/jcm9072315.