Abstract
Background:
The existence of residual aneurysm after intracranial aneurysm clipping bears the risk of re-bleeding, which worsens with the passage of time. Digital subtraction angiography (DSA) is accepted as the gold standard for evaluation of residual aneurysm, but it is invasive, costly, and serious complications are possible.Objectives:
The aim of this study was to compare DSA to 64-slice CT angiography for assessing residual aneurysm.Patients and Methods:
Forty patients with 43 clipped aneurysms from which 36 were torn, were evaluated by DSA after improvement in clinical status, and after a month they were evaluated by 64-slice CT angiography. The pictures were assessed by two neuroradiologists separately, in terms of quality, artifact due to the clips, and the completion of aneurysm closing.Results:
In multislice computed tomographic angiography (MSCT) analysis, 36 pictures (90%) had good quality and four pictures (10%) had poor quality. In case of good quality pictures in MSCT and angiography, the 2- and 3-millimeter residual aneurysms were approved for two patients based on which, sensitivity, feature and positive/negative predictive value for diagnosis of residual aneurysm was 100 for good-quality pictures by MSCT. The level of agreement between the two neuroradiologists was 1 for diagnosing residual aneurysm and 0.86 for vasospasm. The average time for doing MSCT was 12 minutes compared to 45 minutes for DSA angiography, which was cost effective.Conclusion:
CT angiography is a less invasive method with high sensitivity and capabilities for diagnosing residual aneurysm. It is cheaper, quicker and can be accomplished for critical patients. Therefore, it can be taken as the first choice and a replacement for DSA in post-surgery evaluation of patients with clipped brain aneurysm.Keywords
Intracranial Aneurysm CT Angiography Digital Subtraction Angiography
1. Background
Intracranial aneurysm is a very important cause of non-traumatic subarachnoid hemorrhage (SAH) with a mortality rate of 40 to 60 percent (1). After aneurysmal SAH the quick intervention is necessary due to the mortality rate of re-rupture in 32 to 67% of cases. More than one third of the survivors of an aneurysm rupture had neurological deficits and 10 - 20% required long-term care (2). Approximately 10% of cases in which morbidity and mortality occur after SAH from a ruptured intracranial aneurysm result from surgical complications such as major vessel occlusion and re-bleeding (3, 4).
Clipping the adjacent vessels is a short-term complication in these patients, while incomplete clipping of an aneurysm and additional aneurysms are long-term risk factors (5). Incomplete aneurysm clipping leads to re-bleeding with fatal complications (6, 7). Residual aneurysm rate varied from 5.7% to 18% in previous articles (8). Previously it seemed that small neck remnants were not important, but it has been shown that these small neck remnants grow again and become dangerous in long term (7).
Many patients die from primary bleeding or next bleedings. Proper treatment can reduce the re-bleeding risk. Therefore, finding a way to evaluate and find the aneurysm is necessary for endovascular or surgical intervention (1).
Digital subtraction angiography (DSA) has been accepted as the gold standard to evaluate the successful clipping and the correct positioning of the clip (6, 8), but it increases the risk of aneurysm re-bleeding (9) and for this reason it is not used in many centers as routine (4). In a study, up to 90% of patients chose not to follow up when conventional angiography was used as the follow-up procedure (10). As conventional angiography can be unpleasant for patients, a less invasive procedure such as CT may lead to increased patient compliance with follow-up (2). DSA is invasive, time consuming and costly, but CT angiography is non-invasive and requires less contrast and low radiation dose (11, 12).
Due to technological advances, in many centers, magnetic resonance angiography (MRA) and 3-dimensional (3-D) CT angiography are replaced by DSA for pre-operative assessments of the brain aneurysm (6). Computed tomography angiography (CTA) is a good candidate to replace DSA in the acute postoperative setting to evaluate the success of surgery. It is also easy and less costly (1, 5).
Although the risk for clipped aneurysm recurrence is low, there is imaging evidence of aneurysm recurrence with SAH even after successful surgical treatment. These data support the use of routine periodic imaging after successful surgical clipping (13). Having the aneurysm shape, size and adjacent blood vessels before surgery is essential for successful surgery. The incidence of aneurysms remnant has been reported as 3.8% - 8% in previous studies (3).
The major limitation of CT angiography is artifacts of used clips as well as the neck of the aneurysm may be hidden by the clip artifact (2). In some centers 4- slice CT angiography has been used to evaluate aneurysm recurrence after surgery, but the sensitivity and accuracy of 4- slice CT angiography to find the aneurysm remainder is limited. Recently, implementation of 16-slice CT angiography has led to considerable progress in the field of CTA. 16-slice CT angiography improved the quality of three-dimensional reconstructions and reduced times (4).
2. Objectives
Compared to CT angiography, DSA is time consuming, costly and also has complications, the aim of this study was to evaluate the diagnostic value of 64-slice CT angiography than DSA in brain aneurysms after clipping.
3. Patients and Methods
This diagnostic clinical trial study was conducted on 40 patients with brain aneurysm and SAH referred to Imam Hossein Hospital, Tehran, Iran from 2013 to 2014 who underwent brain aneurysm clipping. Patients were enrolled after obtaining written consent.
Yasargil titanium aneurysm clips; Aesculap AG, Tuttlingen and Germany clips were used for patients. After improving the general condition of the patient, DSA was performed for patients with Artis zee biplane system; Siemens Medical Systems Forchheim, Germany.
Within a month after surgery, CT angiography with 64-row multiple detector computed tomography (MDCT) system (Lightspeed; GE Medical Systems, Milwaukee, WI, USA) was done for patients. The results were evaluated as blind by two neuro-radiologists with 12 years of experience. Images were reconstructed by Imam Khomeini hospital neuro-radiologists and were reviewed and interpreted separately.
Written consent was obtained from all patients and data were recorded in checklists confidentially. CT scan settings to perform CT angiography were as follows: 120kvp/250 mA; section thickness, 0.625 mm; 0.5 rotation per second.
Data were collected from patient’s medical records and interviews and were recorded in questionnaires.
Data were analyzed using SPSS Released 2009. PASW Statistics for Windows, Version 18.0. Chicago.USA. Descriptive statistics, chi-square test, Fisher exact test were used. As well as sensitivity and specificity, positive predictive value and negative predictive value were calculated.
4. Results
In this study, 40 patients and 43 brain aneurysms were studied. Twenty-one (52.5%) patients were men and 19 (47.5%) were women. The mean age of patients was 48.35 ± 15 years with the range of 14 to 75 years. The mean aneurysm size was 6.3 ± 2.1 mm and the number of hospitalization days was 21 ± 9 days (Table 1).
Baseline and Clinical Data
| Variables | Mean ± SD | Range |
|---|---|---|
| Aneurysm size, mm | 6.3 ± 2.1 | 4 - 15 |
| Hospitalization days | 21 ± 9 | 10 - 57 |
| From onset of symptoms to referral, Days | 6.5 ± 14.6 | 1 - 86 |
| Referral to perform surgery, Days | 10.8 ± 9.4 | 2 - 46 |
| From Surgery to perform cerebral angiography, Days | 8.1 ± 11.1 | 2 - 20 |
| From Surgery to perform CT angiography, Days | 9.5 ± 4.5 | 2 - 21 |
Distribution of Patients Based on Symptoms and Classification
| Variables | N (%) | |
|---|---|---|
| Symptoms in CT | SAH | 36 (90) |
| Hydrocephalia | 9 (22.5) | |
| Infraction | 3 (7.5) | |
| ICH | 3 (7.5) | |
| IVH | 2 (5) | |
| HUNT and HESS Classification | Grade 1 | 15 (37.5) |
| Grade 2 | 19 (47.5) | |
| Grade 3 | 4 (10) | |
| Grade 4 | 2 (5) | |
| Grade 5 | 0 | |
| Fisher Classification | Grade 1 | 4 (10) |
| Grade 2 | 25 (62.5) | |
| Grade 3 | 9 (22.5) | |
| Grade 4 | 2 (5) | |
| Severity | Vasospasm in DSA, N (%) | Vasospasm in CTA, N (%) | Artifacts in CTA, N (%) |
|---|---|---|---|
| No | 15 (37.5) | 17 (42.5) | 12 (30) |
| Mild | 14 (35) | 12 (30) | 18 (45) |
| Moderate | 8 (20) | 6 (15) | 6 (15) |
| Severe | 3 (7.5) | 5 (12.5) | 4 (10) |
Comparing the Results of Digital Subtraction Angiography (DSA) and Computed Tomography Angiography (CTA) for the Diagnosis of Residual Brain Aneurysm
| Test | DSA | Total | ||
|---|---|---|---|---|
| Result | + | - | ||
| CTA | + | 2 | 0 | 2 |
| - | 0 | 36 | 36 | |
| Total | 2 | 36 | 38 | |
In terms of symptoms in CT, 36 cases (90%) had SAH, nine cases had hydrocephalia, three cases had intracerebral hemorrhage (ICH), and two cases had intraventricular hemorrhage (IVH) (Table 2). Regarding coexisting diseases 26 (65%) patients had a history of hypertension, 13 (32.5%) patients had a history of smoking and seven (17.5%) were diabetics. Frequency of vasospasm severity and artifacts in cerebral arteries are shown in Table 3.
In terms of symptoms on admission, all 40 (100%) patients had headache, and 18 (48%) patients had nausea and vomiting. Five (12.5%) patients were admitted with neurological impairment and four (10%) patients with seizures. The average number of clips used per aneurysms was 1.3 clips. The average level of GCS on admission was 13.6 ± 2.4 which reached to 14.85 ± 0.01 in discharge (P = 0.001).
In terms of location of aneurysms; 15 were in anterior communicating artery (ACOA), 21 in middle cerebral artery (MCA), of which 12 were on the right side, three were on the left side, and three were bilateral. Also six aneurysms were in posterior communicating artery (PCOM) which 5 were in left side and 1 was in right side and there was one aneurysm in the left carotid.
The results of DSA and CTA detecting residual brain aneurysm are compared in Table 4.
Intra-observer error for vasospasm between the two observers was 0.08. But there was no difference between them in the detection of residual aneurysm.
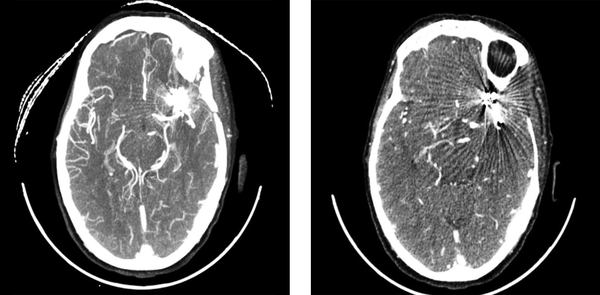
Total of 36 good quality images in which 38 aneurysm were seen took under final review and 4 images were eliminated due to the bad quality and artifacts intensity (Figure 1).
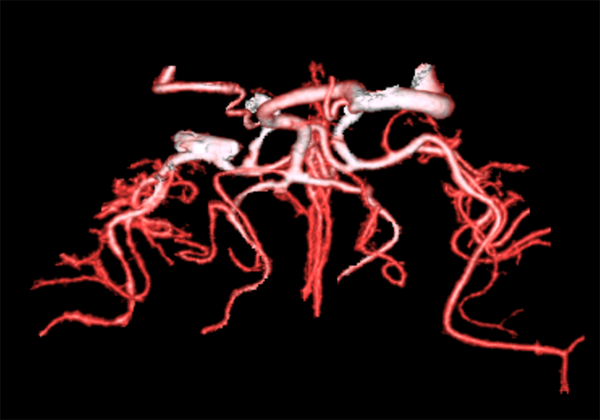
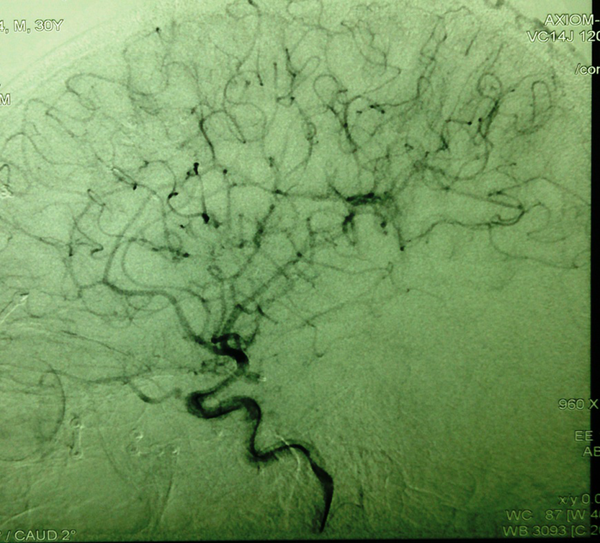
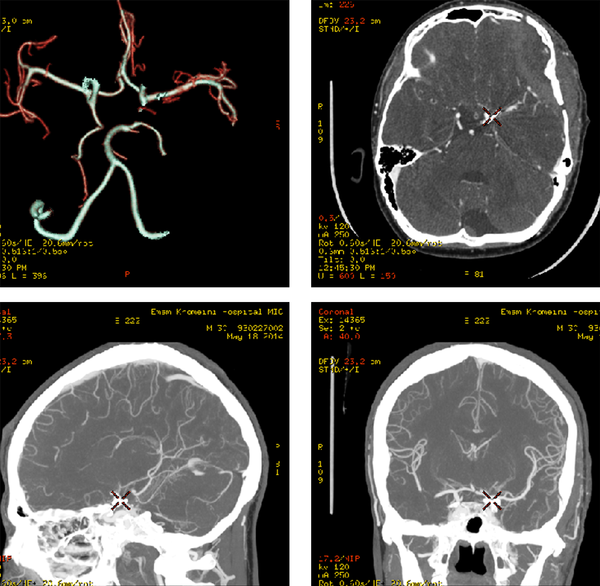
From two cases of aneurysm remaining, a case in the right MCA with 2 mm size and one case in left PCOM with 3 mm size were seen which was confirmed by CT Angiography (Figures 2-4).
Sensitivity = 2/(0+2)=1
Specificity = 36/(0+36)=1
Positive predictive value = 2/(0+2)=1
Negative predictive value = 36/(0+36)=1
Two cases of CT angiography with severe artifacts
CT angiography of a patient with residual aneurysm in the right middle cerebral artery (MCA)
Angiography of a patient with residual aneurysm in the left posterior communicating artery (PCOM)
CT angiography of a patient with residual aneurysm in the left posterior communicating artery (PCOM)
5. Discussion
Use of a noninvasive assessment method to control the status of cerebral aneurysms after surgery is one of the goals of medical centers. From the beginning of modern imaging techniques, attempts have been made to find an alternative for DSA. Efforts are being made to replace it with non-invasive methods.
In the present study, the mean number of days from the onset of symptoms to hospital admission was 6.5 ± 14.6 days with the range of 1 - 86 days. Most patients were admitted in the early days and a number of cases were referred to the center from other provinces. The reason for delay was the referral process and in some cases waiting for the patients to become stable.
Our effort was to perform brain CT angiography for patients during a month after surgery that lasted for an average of 9.5 ± 4.5 days. The reason for prolongation in some cases was adverse conditions of the patients and also the patients’ prolonged stay in ICU or ward.
In this study, the mean age of patients was 48.3 years, but in similar studies, the mean age of patients was estimated as 49 - 55 years which was higher than our study (1, 3, 6, 11, 14). In our study, the mean size of aneurysms was 6.3 ± 2.1 mm. The mean size of aneurysms in a study performed by Luo et al. was 6.4 mm (15) and in a study performed by Chen et al. was 5.5 mm (4), both of which were less than our study.
In 30% of CT angiography images, there was no artifact, but in a study conducted by Golitz et al., 70% of CT angiography images had no artifact (16). The reason for the difference may be related to the type of CT angiography because Gullitz et al. used dual CT angiography to detect the aneurysms (16).
According to both neuroradiologists, the image quality was good in 36 patients (90%), and poor in four cases (10%). In Zhang et al. study the image quality was good in 92% and poor in 8% (12). By increasing the number of CT angiography detectors, thinner and sharper images were achieved and also clip artifacts were minimized (6).
To enhance the diagnostic value of CT angiography in cases in which image quality is poor and there is an abundance of artifacts in the environment, DSA could be performed. In the studies carried out by Zachenhofer and Westerlaan, in cases where CT angiography images did not have sufficient resolution, DSA was performed for patients in the later stages (5, 17).
In the present study, sensitivity, specificity, positive and negative predictive value of CT angiography in the diagnosis of residual aneurysm was 100%. In a study conducted by Luo et al., sensitivity, specificity, positive and negative predictive value of CT angiography in the diagnosis of residual aneurysm was 100% too (15), but in a study performed by Zhang et al., sensitivity, specificity, positive predictive value and negative predictive value were 97%, 100%, 100%, and 97.1 %, respectively (12). Dehdashti et al. reported CT angiography sensitivity and specificity as 100 % (18).
In a meta analysis by Guo et al., a sensitivity of 97% and specificity of 91% was found for 64-slice CT angiography (19). The sensitivity, specificity and accuracy of CT angiography were 95.1%, 94.1%, and 95%, respectively in Donmez et al. study (14). Chen et al. reported the sensitivity, specificity and accuracy of CT angiography as 98.3%, 98% and 97.9%, respectively (1). In a study performed by Teksam, accuracy, sensitivity, and specificity of detecting residual or recurrent aneurysms on MSCTA were 0.80, 0.60, and 1.00, respectively also positive and negative predictive values were 1.00 and 0.71, respectively (6). The sensitivity, specificity, accuracy, positive predictive value and negative predictive value for CT angiography was achieved as 99, 99, 90, 96, and 98 by Westerlaan et al. (17). Uysal et al. reported the sensitivity and specificity of CT angiography in detecting aneurysm as 98.6 and 97.6, respectively (9).
In all previous mentioned studies, the sensitivity and specificity were high and were largely consistent with our study. The differences may relate to the type of device, image quality and neuroradiologists.
Image quality in DSA is better than CT angiography and MRA, but its complications caused long-term problems and hospitalization. Satisfying the patients for angiography is very difficult and in some cases up to 90 percent of the patients avoid angiography in the three-year follow-up.
In relation to the cost of diagnostic methods, now the cost of CT angiography in the public sector is about 3 million Iranian Rials (100 US $) and DSA is about 15 million Iranian Rials (500 US $). Although CT angiography is less invasive, its cost in Iran is one-fifth the cost of DSA. In addition, the time of performing 64-slice CT angiography is about 12 minutes, while DSA takes about 45 minutes. High cost of DSA angiography and also CT angiography were limitations of our study. Consequently, we conducted the study with fewer samples. Further studies with larger samples are suggested.
Regarding that CT angiography is a less invasive method with high sensitivity and capabilities for diagnosing residual aneurysm and considering it is cheaper, quicker and can be accomplished for critical patients, it can be taken as the first choice and a replacement for DSA in post-surgery evaluation of patients with clipped brain aneurysm. The diagnostic value of DSA angiography for the diagnosis of brain aneurysm instead of CT angiography has been noted and mentioned in previous studies, but it was under question after the surgery due to clip artifacts. Therefore, based on the results of the present study it can be concluded that in the case of good quality CT angiography images, they can be low-risk alternative to DSA angiography in the diagnosis of residual aneurysm.
References
-
1.
Chen W, Yang Y, Xing W, Qiu J, Peng Y. Application of multislice computed tomographic angiography in diagnosis and treatment of intracranial aneurysms. Clin Neurol Neurosurg. 2010;112(7):563-71. [PubMed ID: 20510501]. https://doi.org/10.1016/j.clineuro.2010.04.022.
-
2.
Roach CJ, Russell CL, Hanson EH, Bluett B, Orrison WJ. Appearance and impact of post-operative intracranial clips and coils on whole-brain CT angiography and perfusion. Eur J Radiol. 2012;81(5):960-7. [PubMed ID: 21367552]. https://doi.org/10.1016/j.ejrad.2011.01.118.
-
3.
Chen W, Yang Y, Qiu J, Peng Y, Xing W. Clinical application of 16-row multislice computed tomographic angiography in the preoperative and postoperative evaluation of intracranial aneurysms for surgical clipping. Surg Neurol. 2009;71(5):559-65. [PubMed ID: 18786701]. https://doi.org/10.1016/j.surneu.2008.05.014.
-
4.
Chen W, Yang Y, Qiu J, Peng Y, Xing W. Sixteen-row multislice computerized tomography angiography in the postoperative evaluation of patients with intracranial aneurysms. Br J Neurosurg. 2008;22(1):63-70. [PubMed ID: 17952720]. https://doi.org/10.1080/02688690701630108.
-
5.
Zachenhofer I, Cejna M, Schuster A, Donat M, Roessler K. Image quality and artefact generation post-cerebral aneurysm clipping using a 64-row multislice computer tomography angiography (MSCTA) technology: A retrospective study and review of the literature. Clin Neurol Neurosurg. 2010;112(5):386-91. [PubMed ID: 20189713]. https://doi.org/10.1016/j.clineuro.2010.02.001.
-
6.
Teksam M, McKinney A, Cakir B, Truwit CL. Multi-slice computed tomography angiography in the detection of residual or recurrent cerebral aneurysms after surgical clipping. Acta Radiol. 2004;45(5):571-6. [PubMed ID: 15515521].
-
7.
Tomura N, Sakuma I, Otani T, Nisii T, Sugawara M, Koga M, et al. Evaluation of postoperative status after clipping surgery in patients with cerebral aneurysm on 3-dimensional-CT angiography with elimination of clips. J Neuroimaging. 2011;21(1):10-5. [PubMed ID: 19888935]. https://doi.org/10.1111/j.1552-6569.2009.00435.x.
-
8.
Gerardin E, Tollard E, Derrey S, Langlois O, Dacher JN, Douvrin F, et al. Usefulness of multislice computerized tomographic angiography in the postoperative evaluation of patients with clipped aneurysms. Acta Neurochir (Wien). 2010;152(5):793-802. [PubMed ID: 19639249]. https://doi.org/10.1007/s00701-009-0465-4.
-
9.
Uysal E, Ozel A, Erturk SM, Kirdar O, Basak M. Comparison of multislice computed tomography angiography and digital subtraction angiography in the detection of residual or recurrent aneurysm after surgical clipping with titanium clips. Acta Neurochir (Wien). 2009;151(2):131-5. [PubMed ID: 19194652]. https://doi.org/10.1007/s00701-009-0184-x.
-
10.
David CA, Vishteh AG, Spetzler RF, Lemole M, Lawton MT, Partovi S. Late angiographic follow-up review of surgically treated aneurysms. J Neurosurg. 1999;91(3):396-401. [PubMed ID: 10470813]. https://doi.org/10.3171/jns.1999.91.3.0396.
-
11.
Xing W, Chen W, Sheng J, Peng Y, Lu J, Wu X, et al. Sixty-four-row multislice computed tomographic angiography in the diagnosis and characterization of intracranial aneurysms: comparison with 3D rotational angiography. World Neurosurg. 2011;76(1-2):105-13. [PubMed ID: 21839961]. https://doi.org/10.1016/j.wneu.2011.01.046.
-
12.
Zhang LJ, Wu SY, Niu JB, Zhang ZL, Wang HZ, Zhao YE, et al. Dual-energy CT angiography in the evaluation of intracranial aneurysms: image quality, radiation dose, and comparison with 3D rotational digital subtraction angiography. AJR Am J Roentgenol. 2010;194(1):23-30. [PubMed ID: 20028901]. https://doi.org/10.2214/AJR.08.2290.
-
13.
Wallace RC, Karis JP, Partovi S, Fiorella D. Noninvasive imaging of treated cerebral aneurysms, Part II: CT angiographic follow-up of surgically clipped aneurysms. AJNR Am J Neuroradiol. 2007;28(7):1207-12. [PubMed ID: 17698518]. https://doi.org/10.3174/ajnr.A0664.
-
14.
Donmez H, Serifov E, Kahriman G, Mavili E, Durak AC, Menku A. Comparison of 16-row multislice CT angiography with conventional angiography for detection and evaluation of intracranial aneurysms. Eur J Radiol. 2011;80(2):455-61. [PubMed ID: 20729022]. https://doi.org/10.1016/j.ejrad.2010.07.012.
-
15.
Luo Z, Wang D, Sun X, Zhang T, Liu F, Dong D, et al. Comparison of the accuracy of subtraction CT angiography performed on 320-detector row volume CT with conventional CT angiography for diagnosis of intracranial aneurysms. Eur J Radiol. 2012;81(1):118-22. [PubMed ID: 21632193]. https://doi.org/10.1016/j.ejrad.2011.05.003.
-
16.
Golitz P, Struffert T, Ganslandt O, Saake M, Lucking H, Rosch J, et al. Optimized angiographic computed tomography with intravenous contrast injection: an alternative to conventional angiography in the follow-up of clipped aneurysms? J Neurosurg. 2012;117(1):29-36. [PubMed ID: 22519433]. https://doi.org/10.3171/2012.3.JNS111895.
-
17.
Westerlaan HE. "Multislice CT angiography in the selection of patients with ruptured intracranial aneurysms suitable for clipping or coiling. ". Neuroradiol. 2007;49(12):997-1007.
-
18.
Dehdashti AR, Binaghi S, Uske A, Regli L. Comparison of multislice computerized tomography angiography and digital subtraction angiography in the postoperative evaluation of patients with clipped aneurysms. J Neurosurg. 2006;104(3):395-403. [PubMed ID: 16572652]. https://doi.org/10.3171/jns.2006.104.3.395.
-
19.
Guo W, He XY, Li XF, Qian DX, Yan JQ, Bu DL, et al. Meta-analysis of diagnostic significance of sixty-four-row multi-section computed tomography angiography and three-dimensional digital subtraction angiography in patients with cerebral artery aneurysm. J Neurol Sci. 2014;346(1-2):197-203. [PubMed ID: 25194636]. https://doi.org/10.1016/j.jns.2014.08.023.


