Abstract
Background:
Colon cancer is a leading cause of morbidity and mortality in developed countries. The early detection of colorectal cancer using screening programs is important for managing early-stage colorectal cancers and polyps. Modalities that allow examination of the entire colon are conventional colonoscopy, double contrast barium enema examination and multi-detector computed tomography (MDCT) colonography.Objectives:
To compare CT colonography and conventional colonoscopy results and to evaluate the accuracy of CT colonography for detecting colorectal lesions.Patients and Methods:
In a prospective study performed at Gastroenterology and Radiology Departments of Medical Faculty of Eskisehir Osmangazi University, CT colonography and colonoscopy results of 31 patients with family history of colorectal carcinoma, personal or family history of colorectal polyps, lower gastrointestinal tract bleeding, change in bowel habits, iron deficiency anemia and abdominal pain were compared. Regardless of the size, CT colonography and conventional colonoscopy findings for all the lesions were cross - tabulated and the sensitivity, specificity, and positive and negative predictive values were calculated. To assess the agreement between CT colonography and conventional colonoscopy examinations, the Kappa coefficient of agreementt was used. Statistical analysis was performed by SPSS ver 15.0.Results:
Regardless of the size, MDCT colonography showed 83% sensitivity and 95% specificity, with a positive predictive value of 95% and a negative predictive value of 83% for the detection of colorectal polyps and masses. MDCT colonography displayed 92% sensitivity and 95% specificity, with a positive predictive value of 92% and a negative predictive value of 95% for polyps ≥ 10 mm. For polyps between 6mm and 9 mm, MDCT colonography displayed 75% sensitivity and 100% specificity, with a positive predictive value of 100% and a negative predictive value of 90%. For polyps ≤ 5 mm MDCT colonography displayed 88% sensitivity and 100% specificity with a positive predictive value of 100% and a negative predictive value of 95%.Conclusions:
CT colonography is a safe and minimally invasive technique, a valuable diagnostic tool for examining the entire colon and a good alternative compared to other colorectal cancer screening tests because of its high sensitivity values in colorectal lesions over 1 cm.Keywords
Colonography Computed Tomographic Colonoscopy Colonic Polyps Colorectal Neoplasms
1. Background
Colon cancer is a leading cause of morbidity and mortality in developed countries (1). Because of the progression of colorectal polyps to carcinoma over time, the early diagnosis of premalignant lesions, such as polyps, is of great importance for patient survival (2). Screening and diagnostic methods, such as occult blood in the stool, single-and double-contrast barium enema, sigmoidoscopy and conventional colonoscopy, are used in diagnosing colorectal neoplasia (3). For detecting of colorectal neoplasia and imaging of asymptomatic high-risk individuals, conventional colonoscopy is considered as the gold standard. However, on average, it is not possible to view the entire colon using colonoscopy in 5% of the patients. Additionally, colonoscopy moves only in one direction, creating potential blind spots where several lesions may be missed. There is no likelihood of evaluating the liver and other organs through colonoscopy. Although complications of colonoscopy are more common during therapeutic procedures, colonoscopy has many life - threatening complications, such as perforation, major bleeding and bacteremia (2). Furthermore, the incidence of severe cardiopulmonary complications due to anesthesia administration during colonoscopy is 0.9%.
Computed tomography (CT) colonography is an imaging modality that has been rapidly developing since its discovery in 1994 by Vining (4). Its technique is based on helical thin-section CT scan imaging on cleansed and distended colon. Multi-planar two dimensional (2D) and virtual endoscopic three dimensional (3D) displays are obtained by processing these data using computer systems (5).
2. Objectives
The aims of our study were to compare the results of multi-detctor CT (MDCT) colonography and conventional colonoscopy to detect colorectal lesions and to investigate the effectiveness of MDCT colonography.
3. Patients and Methods
3.1. Patient Enrolment
Family history of colorectal cancer personal or family history of colorectal polyps, bleeding, change in bowel habits, abdominal pain and iron deficiency anemia were identified as inclusion criteria. Exclusion criteria were history of familial adenomatous polyposis or hereditary non-polypoid cancer, previous colorectal surgery, suspicion of inflammatory bowel disease, acute diverticulitis, intestinal obstruction, denial of CT colonography and pregnancy. The study included a total of 31 patients; (n = 15 females and 16 males). The patients ranged in age between 38 years and 74 years with a mean age of 45 years.
3.2. Ethics Committee
All of the patients were informed about the investigation and written informed consent was obtained. The study was approved (decision no. 219) by the ethics committee on June 26, 2006.
3.3. CT Colonography Technique
A total of 45 mL sodium phosphate, 250 mL 2.5% barium sulfate solution and 50 mL urografin was administered to the patients, with 3 hour intervals on the afternoon of the day before the CT colonography examination was conducted. Sodium phosphate solution was used for bowel cleansing, barium sulfate solution was used to mark fecaloid material and urographin was used to mark the residual liquid content of the bowels and to facilitate bowel cleansing.
CT colonography was performed using a 64-detector CT scanner (Toshiba Aquilion, Shimoishigami, Otawara-shi, Tochigi-ken, Japan). Medications for reducing smooth muscle spasm and intravenous contrast material were not administered. After placing the silicone tip into the rectum, the entire colon was inflated with room air as long as the patient could tolerate the procedure. The silicone tip was left in the rectum, and a scanogram was obtained to evaluate whether adequate bowel distension was available with the patient in the supine position. If adequate bowel distension was achieved, images of the entire colon and rectum were obtained with the patient in the supine and prone positions, respectively, in cranio-caudal direction. The MDCT examination was performed at 120 kV, 0.5 second gantry rotation time, and X-ray parameter was 102 mA. The images were obtained at 0.5 × 64 collimation and 5-mm slice thickness. CT images with 2mm to 5mm thickness were reconstructed at coronal and sagittal planes. To reduce the radiation dose received by the patients, the radiation dose reduction program that automatically adjusts mAs according to the thickness of the patient’s body was applied.
3.4. Evaluation of Images
CT images were sent to a separate workstation via the network. First, 5mm thick axial images and subsequently coronal and sagittal multiplanar reformatted images were evaluated with the patients in the supine and prone positions. The volume rendering technique (VRT) computer program was used to generate a virtual colonoscopy for all of the patients after selecting a position with better distension.
The presence of colorectal polyps, colonic localization and morphological features were evaluated by dividing the colon into six segments (cecum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum). The pathologic findings were re-evaluated by changing the window width and level values. Fecal waste was marked with barium and the separation of fecal waste materials from the polyps was performed by their heterogeneous internal structure and barium content. The abnormal densities that shifted their locations in the supine and prone positions were interpreted in favor of the residual stool.
The CT images were evaluated by the same radiologist with 25 years of experience in abdominal imaging.
3.5. Conventional Colonoscopy Technique
A conventional colonoscopy was performed within 1 week after CT colonography.The gastroenterologists had no information about CT colonography results and had a minimum 5-year experience in conventional colonoscopy. The colon was divided into six segments for evaluation, as performed in the CT colonography. All colonoscopies were successfully performed by visualizing the entire colon from rectum to cecum.
3.6. Comparison of CT Colonography and Conventional Colonoscopy Results
Lesions detected by CT colonography and conventional colonoscopy at the same anatomical segment with similar morphology and size were defined as true positive. If CT colonography and conventional colonoscopy had not detected any lesion in the same segment, this result was defined as true negative. If a finding noted by CT colonography was not detected in the same segment using conventional colonoscopy, this result was defined as false positive. If a lesion noted by conventional colonoscopy was not detected by CT colonography in the same region, conventional colonoscopy was repeated and if no lesions were detected again, this result was identified as false negative.
3.7. Statistical Analysis
Patients with pathological findings were divided into three groups according to the size of the lesions, 10 mm and above, between 6 mm and 9 mm, and 5 mm and below. The findings of CT colonography and conventional colonoscopy were evaluated for agreement and the results were calculated. In a statistical analysis for assessing the agreement between CT colonography and conventional colonoscopy examinations, the Kappa coefficient was used. The statistical analysis was done by SPSS ver 15.0 (SPSS Inc. Chicago, IL). For interpretation of Kappa coefficient, we used this guideline: K = 0 - 0.19 was considered as no agreement, K = 0.2 - 0.39 was considered as weak agreement, K = 0.4 - 0.59 was considered as moderate agreement, K = 0.6 - 0.79 was considered as good level of agreement, and K = 0.8 - 1 was considered as excellent level of agreement. Regardless of the size, CT colonography and conventional colonoscopy findings for all lesions were cross-tabulated and the sensitivity, specificity, and positive and negative predictive values were calculated.
4. Results
Regardless of size, MDCT colonography displayed 83% sensitivity and 95% specificity, with a positive predictive value of 95% and a negative predictive value of 83% for detecting colorectal polyps and masses. MDCT colonography displayed 92% sensitivity and 95% specificity, with a positive predictive value of 92% and a negative predictive value of 95% for polyps ≥ 10 mm. For polyps between 6 mm and 9 mm, MDCT colonography displayed 75% sensitivity and 100% specificity, with a positive predictive value of 100% and a negative predictive value of 90%. For polyps ≤ 5 mm, MDCT colonography displayed 88% sensitivity and 100% specificity with a positive predictive value of 100% positive and a negative predictive value of 95%. The statistical evaluation of MDCT colonography results according to the size of polypoid lesions and Kappa coefficient of the agreement between MDCT colonography and conventional colonoscopy are summarized in Tables 1 and 2.
| Size of Polypoid Lesions | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| ≤ 5, mm | 0.875 | 1 | 1 | 0.952 |
| 6 - 9, mm | 0.750 | 1 | 1 | 0.909 |
| ≥ 10, mm | 0.917 | 0.952 | 0.917 | 0.952 |
| All lesions | 0.833 | 0.952 | 0.952 | 0.833 |
Kappa Coefficient of Agreement Between MDCT Colonography and Conventional Colonoscopy
| Size of Polypoid Lesions | Kappa Coefficient | P Value |
|---|---|---|
| All lesions | 0.779 (0.542 - 0.851) | < 0.001 |
| ≥ 10, mm | 0.869 (0.581 - 0.964) | < 0.001 |
| 6 - 9, mm | 0.811 (0.455 - 0.811) | < 0.001 |
| ≤ 5, mm | 0.909 (0.577 - 0.909) | < 0.001 |
Four polyps detected using conventional colonoscopy were not determined at MDCT colonography (false negative). One polyp detected using MDCT colonography was not detected with conventional colonoscopy (false positive). One polyp over 10 mm and 2 polyps between 6 mm and 9 mm were not detected due to failure in distinguishing them from the mucosal folds and one polyp below 5 mm was not detected because of inadequate colon cleansing during MDCT colonography.
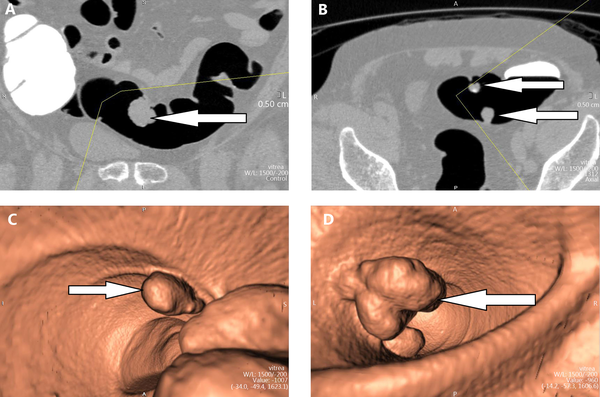
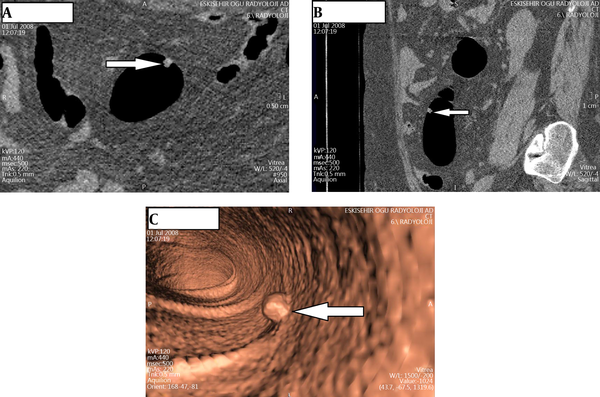
Among 11 patients with pathological findings, three patients had tumors, one patient had two polyps, one patient had three polyps, one patient had four polyps and one patient had six polyps. In one patient with a tumor, two polyps were detected in the adjacent lesion. The samples from MDCT colonography findings in the patients are shown in Figures 1 and 2. Seven of the total 24 polyps were ≤ 5 mm, six polyps were between 6 mm and 9 mm, and 11 polyps were ≥ 10 mm. In a histopathological examination of 24 polyps detected using MDCT colonography, nine polyps were diagnosed as tubular adenoma, two polyps were diagnosed as tubulovillous adenoma, and 10 polyps were diagnosed as hyperplastic polyp. Histopathological diagnosis of all three tumors was adenocarcinoma (Table 3). In addition to the detection of polyps, CT colonography was effective in diagnosing colorectal cancer in three cases in our study.
A 55-year-old man suffering from abdominal pain. A and B, Axial CT images: Tumor in the sigmoid colon and two adjacent polyps. C and D, Virtual colonoscopy appearance of tumors and polyps.
A 52-year-old man suffering from rectal bleeding. A, Axial CT image of 8 mm polyp in the sigmoid colon. B, Sagittal reformatted CT image. C, Virtual colonoscopy image.
Polypoid Lesions Classified According to Size, and Histopathology
| 1 - 5, mm | 6 - 9, mm | ≥ 10, mm | All of Them | |
|---|---|---|---|---|
| Tubular adenoma | - | 3 | 6 | 9 |
| Tubulovillous adenoma | - | - | 2 | 2 |
| Hyperplastic adenoma | 7 | 3 | - | 10 |
| Adenocarcinoma | - | - | 3 | 3 |
5. Discussion
Colorectal cancer is a major health problem causing significant morbidity and mortality. The majority of colorectal cancers develop from an ever-growing benign adenomatous polyp over the years (1). Detection of premalignant polyps and early-stage cancers using screening programs and follow-up resection can be lifesaving (6). Options for colorectal carcinoma screening include fecal occult blood test, sigmoidoscopy, double-contrast barium examination, colonoscopy, and combinations of these tests (3). Virtual colonoscopy, described by Vining and colleagues in 1994, gained popularity in a short time as a promising colorectal cancer screening method (4). CT colonography offers a reliable, effective and fast method for colonic examination. Many advantages of CT colonography include high levels of patient preference, absence of sedation and the ability to evaluate extra-colonic findings during imaging (7).
CT colonography is based on helical and thin-section CT scan of the cleansed and distended colon. Increased sensitivity in the detection of small lesions can be achieved through high spatial resolution and short scan time of the multi-detector CT colonography. Multiplanar 2D and virtual endoscopic 3D displays are obtained by processing the data using computer systems (5).
Colon cleansing is very important for obtaining quality CT colonography examinations. Residual stool/liquid could lead to false positive and false negative results (7). A large number of laxative solutions, such as polyethylene glycol, sodium phosphate and magnesium citrate, are used in colon cleansing (8). Polyethylene glycol solutions are not currently preferred because they cause significant residual liquid (9, 10). Macari et al. (10) compared the sodium phosphate laxative solution with the polyethylene solution and discovered that the sodium phosphate solution generates significantly less residual liquid. In our study, we used oral sodium phosphate solutions for colon cleansing.
Despite the use of maximum dose of colon cleansing solutions, residual stool causes difficulties in diagnosis. Residual fecal marking methods help to distinguish fecaloid material from the actual lesions and improve the accuracy of CT colonography (7). Lefere et al. (11) were able to achieve an average value of 85% sensitivity in their study of 50 patients through the use of oral contrast added to the low fiber diet and an average colon cleansing. Pickhardt et al. (12) achieved excellent results by using laxative cleaning with a combination of fluid and stool marking (for fecal marking, 500 mL of 2% barium; for liquid marking, 120 mL of water-soluble ionic contrast agent Gastrografin®). In our study, we used a 2% solution of barium for residual fecal marking and diatrizoate preparation (ionic water-soluble contrast agent) for residual liquid marking.
Several researchers have indicated that using intravenous contrast material will facilitate the detection of colorectal polyps in the presence of a large amount of residual liquid (13). Recent studies have reported that intravenous contrast material is successful in detecting traceable liver metastases rather than showing colorectal abnormalities. Due to the necessity of using an intravenous catheter and the risk of allergy development due to ionic contrast media, using intravenous contrast agents is not recommended (14). Because residual fluid/stool was readily marked or because there were potential limitations and contraindications of the intravenous contrast medium, we did not use intravenous contrast medium in our study.
Sufficient colon distension is essential for optimal CT colonography imaging. Room air or CO2 is used for colonic distension (7). Manually inflating the colon using room air occasionally leads to painful distension. The primary benefit of CO2 is the absorption of gas in the colon wall, which increases patient comfort after the procedure (8). In our study, although we used room air for distension, we did not detect significant patient complaints.
There is consensus on the use of supine and prone CT colonography images to separate moving residual stool from fixed polyps and cancer pathologies and to optimally evaluate the collapsed segments. Although Callstrom et al. (15) reported that the distension of the sigmoid colon is better in the supine position, Morrin et al. (16) found that rotating the patient from supine to prone position increased colonic distension, especially at the rectum and left colon. Studies have shown that the joint use of supine and prone positions increases the accuracy of detecting polyps compared to the sole use of supine position (16-18). In our study, we used both supine and prone positions and found that prone position increased the distension of the rectosigmoid region.
The radiation dose received by the patient during CT colonography is the primary disadvantage of the procedure. Screening in both supine and prone positions increases the dose of radiation received (19). Researchers reduced the tube current to lower the radiation dose. Dachman al. (20) discovered no significant difference in diagnostic accuracy between 70 mA and 140 mA X-ray parameters, whereas the radiation dosage received by the patient decreased by 75% with the administration of 70 mA. Considering the thickness of the patient’s body, we used the minimal mA values, which were automatically adjusted between 70 mA and 150 mA. The radiation dose received in CT colonography is lower than that received in conventional abdominal CT or barium enema examinations, although it will still contribute to the radiation dose received over the patient’s life span.
CT colonography is a minimally invasive technique that allows examination of the entire colon. Compared with single-slice CT, MDCT offers many advantages that improve the diagnostic performance of CT colonography. Large areas of the body are scanned using high spatial resolution in short periods. Fast-paced shooting time and high spatial resolution increase the sensitivity in detecting polyps and avoid artifacts due to voluntary-involuntary motion movements. MDCT procedure enables the formation of high-quality 3D images and thus increases the positive predictive value in the detection of small lesions (5).
The majority of studies in the literature assert that axial images need to be supplemented with 3D images. The study by Iannaccone et al. (21) reported a sensitivity of 83% in detecting 22 polyps sized 8 mm and more, where axial two-dimensional images are used together with 3D visualization. The majority of studies have primarily considered 2D images and used 3D images in problem solving (11, 15, 22, 23). Several studies have reported excellent results with the primary use of 3D images (12, 24). In fact, the use of 3D images serves mostly to distinguish between polyps and complex colonic folds that look similar in axial images (25, 26). The majority of researchers agree that 2D images are not sufficient for evaluating abnormalities. Pickhardt et al. (12) have shown that 3D points of view appear to be an effective and accurate method for identifying lesions. In our study, we also supplemented 2D images with 3D images in evaluating the lesions.
Today, new software algorithms that have been developed are replacing the traditional 2D and 3D endoluminal images. Virtual gross pathological imaging (virtual gross dissection) allows visualization of the colon on the long axis, so that flat lesions can be viewed in a tubular form as in actual pathological preparations (27, 28). Computer-aided detection systems (CAD) automatically detect polyps and masses in CT images. This method is used as a marker to determine localization of suspected lesions by the radiologist. Computer-aided detection, which can be used as a second reader, also improves the diagnostic performance of the radiologist (29). It has been reported that large-scale clinical trials are required to determine the performance characteristics of this method (30).
The European Society of Gastrointestinal and Abdominal Radiology (ESGAR) and European Association of Radiology (EAR) published the results of a meta-analysis including 24 studies and 4,181 patients and reported a sensitivity of 93% and a specificity of 97% for detecting polyps ≥ 10 mm using CT colonography. When polyps ≥ 6 mm were included in the analysis, specificity and sensitivity were reported to be 86% (31). Wessling et al. (32) must be corrected as Hara et al. (32) studied 30 polyps examined by MDCT and reported that CT colonography has 93% sensitivity for polyps ≥ 10 mm, 86% sensitivity for polyps between 6 mm and 9 mm, and 70% sensitivity for polyps ≤ 5 mm. According to the MDCT colonography study of 132 polyps, Macari et al. (33) revealed 93% sensitivity for polyps ≥ 10 mm, 70% sensitivity for polyps between 6 mm and 9 mm, and 52% sensitivity for polyps ≤ 5 mm. Studies showed that the sensitivity of MDCT colonography decreased for polyps below the size of 10 mm in general and decreased for polyps smaller than 5 mm in particular. However, the likelihood of cancer or the prospect of developing into cancer is low for polyps smaller than 10 mm (34, 35). Although the results of our study are consistent with the findings reported in the literature, the sensitivity and negative predictive value of MDCT colonoscopy for lesions below 5 mm are higher than lesions between 6 mm and 9 mm. This finding may be related to the improper detection of flat adenomas, which cannot be easily distinguished from mucosal folds, but can be distinguished from mucosal folds with chromoendoscopy and narrow band imaging techniques.
CT colonography, compared to colonoscopy, is a non-invasive and relatively painless procedure. Many studies investigating patient preferences between CT colonography and colonoscopy have reported that CT colonography is the preferred modality. Svensson et al. (36) reported patient preference in favor of CT colonography in 82% of cases where CT colonography was followed by conventional colonoscopy. In our study, MDCT colonography was the highly preferred modality.
In addition to detection of polyps, CT colonography is successful in diagnosing colorectal cancer. Fenlon et al. (37) studied 100 patients at high risk for colorectal neoplasia and reported 100% sensitivity in detecting cancer cases. Another advantage of CT colonography in patients with occlusive tumor is the assessment of the proximal part of the colon. In a study of 29 patients, CT colonography was successful in detecting all 29 cases of occlusive cancer as well as 24 polyps and two cancer cases observed in the proximal colon (37). Although there were no occlusive tumor cases in our study, all of the three adenocarcinoma cases were correctly detected. Two polyps concomitant of adenocarcinoma were also correctly identified.
Because the abdomen and pelvis are also screened with the colon during CT colonography, CT colonography offers the advantage of evaluating the extra-colonic findings. A study has classified the importance of extra-colonic findings of CT colonography according to clinical relevance as important (10%), moderately important (27%) and low importance (50%) (38). Hara et al. reported similar findings (39). This lifesaving advantage is not found in any of the other colorectal imaging procedures. In our study, a primary lung tumor was identified in the lower lobe of the left lung using MDCT colonography for a patient scheduled for a colonoscopy due to iron deficiency anemia.
CT colonography performance varies according to the expert experience. The ESGAR study has also shown that the more experienced assessors have identified significantly more lesions (66% vs. 51%) compared with less experienced assessors and their accuracy rates were higher (66% vs. 74%) (37).
Limitations of this study are the relatively low number of patients and the absence of occlusive tumoral cases. In daily practice, colonoscopic procedures are usually performed on patients with moderate bowel cleansing; however, patients with complete bowel cleansing were selected for this study.
In summary, CT colonography is a valuable diagnostic tool for examining the entire colon. MDCT colonography is a good alternative to other existing colorectal cancer screening tests because of its high sensitivity values in colorectal lesions over 1 cm and because it is a relatively safe and minimally invasive procedure. CT colonography appears to be an accurate and effective method for detecting polyps and early cancers in the selected patient population.
References
-
1.
Yee J, Akerkar GA, Hung RK, Steinauer-Gebauer AM, Wall SD, McQuaid KR. Colorectal neoplasia: performance characteristics of CT colonography for detection in 300 patients. Radiology. 2001;219(3):685-92. [PubMed ID: 11376255]. https://doi.org/10.1148/radiology.219.3.r01jn40685.
-
2.
Chung DJ, Huh KC, Choi WJ, Kim JK. CT colonography using 16-MDCT in the evaluation of colorectal cancer. AJR Am J Roentgenol. 2005;184(1):98-103. [PubMed ID: 15615957]. https://doi.org/10.2214/ajr.184.1.01840098.
-
3.
Waye JD, Bashkoff E. Total colonoscopy: is it always possible? Gastrointest Endosc. 1991;37(2):152-4. [PubMed ID: 2032598].
-
4.
Vining DJ, Gelfand DW. Technical feasibility of colon imaging with helical CT and virtual reality. Am J Roentgenol. 1994;162:104.
-
5.
Bakir B, Yekeler E, Tunaci M, Tunaci A, Acunas B, Acunas G. [Diagnostic efficiency of multislice computed tomography colonography in the detection of colorectal tumors: comparison with conventional colonography]. Tani Girisim Radyol. 2004;10(3):218-29. [PubMed ID: 15470625].
-
6.
Ferrucci JT. Colon cancer screening with virtual colonoscopy: promise, polyps, politics. AJR Am J Roentgenol. 2001;177(5):975-88. [PubMed ID: 11641151]. https://doi.org/10.2214/ajr.177.5.1770975.
-
7.
Barish MA, Rocha TC. Multislice CT colonography: current status and limitations. Radiol Clin North Am. 2005;43(6):1049-62. viii. [PubMed ID: 16253661]. https://doi.org/10.1016/j.rcl.2005.07.008.
-
8.
Barish MA, Soto JA, Ferrucci JT. Consensus on current clinical practice of virtual colonoscopy. AJR Am J Roentgenol. 2005;184(3):786-92. [PubMed ID: 15728598]. https://doi.org/10.2214/ajr.184.3.01840786.
-
9.
Fletcher JG, Johnson CD, MacCarty RL, Welch TJ, Reed JE, Hara AK. CT colonography: potential pitfalls and problem-solving techniques. AJR Am J Roentgenol. 1999;172(5):1271-8. [PubMed ID: 10227501]. https://doi.org/10.2214/ajr.172.5.10227501.
-
10.
Macari M, Lavelle M, Pedrosa I, Milano A, Dicker M, Megibow AJ, et al. Effect of different bowel preparations on residual fluid at CT colonography. Radiology. 2001;218(1):274-7. [PubMed ID: 11152814]. https://doi.org/10.1148/radiology.218.1.r01ja31274.
-
11.
Lefere PA, Gryspeerdt SS, Dewyspelaere J, Baekelandt M, Van Holsbeeck BG. Dietary fecal tagging as a cleansing method before CT colonography: initial results polyp detection and patient acceptance. Radiology. 2002;224(2):393-403. [PubMed ID: 12147834]. https://doi.org/10.1148/radiol.2241011222.
-
12.
Pickhardt PJ, Choi JR, Hwang I, Butler JA, Puckett ML, Hildebrandt HA, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349(23):2191-200. [PubMed ID: 14657426]. https://doi.org/10.1056/NEJMoa031618.
-
13.
Morrin MM, Farrell RJ, Kruskal JB, Reynolds K, McGee JB, Raptopoulos V. Utility of intravenously administered contrast material at CT colonography. Radiology. 2000;217(3):765-71. [PubMed ID: 11110941]. https://doi.org/10.1148/radiology.217.3.r00nv42765.
-
14.
Macari M, Bini EJ. CT colonography: where have we been and where are we going? Radiology. 2005;237(3):819-33. [PubMed ID: 16237143]. https://doi.org/10.1148/radiol.2373041717.
-
15.
Callstrom MR, Johnson CD, Fletcher JG, Reed JE, Ahlquist DA, Harmsen WS, et al. CT colonography without cathartic preparation: feasibility study. Radiology. 2001;219(3):693-8. [PubMed ID: 11376256]. https://doi.org/10.1148/radiology.219.3.r01jn22693.
-
16.
Morrin MM, Farrell RJ, Keogan MT, Kruskal JB, Yam CS, Raptopoulos V. CT colonography: colonic distention improved by dual positioning but not intravenous glucagon. Eur Radiol. 2002;12(3):525-30. [PubMed ID: 11870464]. https://doi.org/10.1007/s003300100954.
-
17.
Fenlon HM, Barish MA, Ferrucci JT. Virtual colonoscopy--technique and applications. Ital J Gastroenterol Hepatol. 1999;31(8):713-20. [PubMed ID: 10730564].
-
18.
Pescatore P, Glucker T, Delarive J, Meuli R, Pantoflickova D, Duvoisin B, et al. Diagnostic accuracy and interobserver agreement of CT colonography (virtual colonoscopy). Gut. 2000;47(1):126-30. [PubMed ID: 10861274].
-
19.
Hara AK, Johnson CD, Reed JE, Ahlquist DA, Nelson H, Ehman RL, et al. Reducing data size and radiation dose for CT colonography. AJR Am J Roentgenol. 1997;168(5):1181-4. [PubMed ID: 9129408]. https://doi.org/10.2214/ajr.168.5.9129408.
-
20.
Dachman AH, Kuniyoshi JK, Boyle CM, Samara Y, Hoffmann KR, Rubin DT, et al. CT colonography with three-dimensional problem solving for detection of colonic polyps. AJR Am J Roentgenol. 1998;171(4):989-95. [PubMed ID: 9762982]. https://doi.org/10.2214/ajr.171.4.9762982.
-
21.
Iannaccone R, Laghi A, Catalano C, Mangiapane F, Lamazza A, Schillaci A, et al. Computed tomographic colonography without cathartic preparation for the detection of colorectal polyps. Gastroenterology. 2004;127(5):1300-11. [PubMed ID: 15520999].
-
22.
Fletcher JG, Johnson CD, Welch TJ, MacCarty RL, Ahlquist DA, Reed JE, et al. Optimization of CT colonography technique: prospective trial in 180 patients. Radiology. 2000;216(3):704-11. [PubMed ID: 10966698]. https://doi.org/10.1148/radiology.216.3.r00au41704.
-
23.
Yee J, Hung RK, Akerkar GA, Wall SD. The usefulness of glucagon hydrochloride for colonic distention in CT colonography. AJR Am J Roentgenol. 1999;173(1):169-72. [PubMed ID: 10397121]. https://doi.org/10.2214/ajr.173.1.10397121.
-
24.
Vos FM, van Gelder RE, Serlie IW, Florie J, Nio CY, Glas AS, et al. Three-dimensional display modes for CT colonography: conventional 3D virtual colonoscopy versus unfolded cube projection. Radiology. 2003;228(3):878-85. [PubMed ID: 12954902]. https://doi.org/10.1148/radiol.2283020846.
-
25.
McFarland EG. Reader strategies for CT colonography. Abdom Imaging. 2002;27(3):275-83. [PubMed ID: 12173358].
-
26.
Rottgen R, Fischbach F, Plotkin M, Lorenz M, Freund T, Schroder RJ, et al. CT colonography using different reconstruction modi. Clin Imaging. 2005;29(3):195-9. [PubMed ID: 15855065]. https://doi.org/10.1016/j.clinimag.2004.07.005.
-
27.
Sorantin E, Werkgartner G, Balogh E, Vilanova i Bartroli A, Palagyi K, Nyul LG, et al. Virtual Dissection and Automated Polyp Detection of the Colon Based on Spiral CT - Techniques and Preliminary Experience on a Cadaveric Phantom. European Surg Acta Chir Austriaca. 2002;34(2):143-9. https://doi.org/10.1046/j.1563-2563.2002.02018.x.
-
28.
Yoshida H, Dachman AH. CAD techniques, challenges, and controversies in computed tomographic colonography. Abdom Imaging. 2005;30(1):26-41. [PubMed ID: 15647868]. https://doi.org/10.1007/s00261-004-0244-x.
-
29.
Nicholson FB, Taylor S, Halligan S, Kamm MA. Recent developments in CT colonography. Clin Radiol. 2005;60(1):1-7. [PubMed ID: 15642287]. https://doi.org/10.1016/j.crad.2004.07.010.
-
30.
Halligan S, Taylor SA. CT colonography: results and limitations. Eur J Radiol. 2007;61(3):400-8. [PubMed ID: 17174055]. https://doi.org/10.1016/j.ejrad.2006.07.030.
-
31.
Wessling J, Fischbach R, Domagk D, Lugering N, Neumann E, Heindel W. Colorectal polyps: Detection with multi-slice CT colonography. Rofo. 2001;173(12):1069-71. [PubMed ID: 11740665]. https://doi.org/10.1055/s-2001-18894.
-
32.
Hara AK, Johnson CD, Reed JE, Ehman RL, Ilstrup DM. Colorectal polyp detection with CT colography: two- versus three-dimensional techniques. Work in progress. Radiology. 1996;200(1):49-54. [PubMed ID: 8657944]. https://doi.org/10.1148/radiology.200.1.8657944.
-
33.
Macari M, Bini EJ, Xue X, Milano A, Katz SS, Resnick D, et al. Colorectal neoplasms: prospective comparison of thin-section low-dose multi-detector row CT colonography and conventional colonoscopy for detection. Radiology. 2002;224(2):383-92. [PubMed ID: 12147833]. https://doi.org/10.1148/radiol.2242011382.
-
34.
Fenlon HM, Nunes DP, Schroy P3, Barish MA, Clarke PD, Ferrucci JT. A comparison of virtual and conventional colonoscopy for the detection of colorectal polyps. N Engl J Med. 1999;341(20):1496-503. [PubMed ID: 10559450]. https://doi.org/10.1056/NEJM199911113412003.
-
35.
Halligan S, Altman DG, Taylor SA, Mallett S, Deeks JJ, Bartram CI, et al. CT colonography in the detection of colorectal polyps and cancer: systematic review, meta-analysis, and proposed minimum data set for study level reporting. Radiology. 2005;237(3):893-904. [PubMed ID: 16304111]. https://doi.org/10.1148/radiol.2373050176.
-
36.
Svensson MH, Svensson E, Lasson A, Hellstrom M. Patient acceptance of CT colonography and conventional colonoscopy: prospective comparative study in patients with or suspected of having colorectal disease. Radiology. 2002;222(2):337-45. [PubMed ID: 11818597]. https://doi.org/10.1148/radiol.2222010669.
-
37.
Fenlon HM, McAneny DB, Nunes DP, Clarke PD, Ferrucci JT. Occlusive colon carcinoma: virtual colonoscopy in the preoperative evaluation of the proximal colon. Radiology. 1999;210(2):423-8. [PubMed ID: 10207425]. https://doi.org/10.1148/radiology.210.2.r99fe21423.
-
38.
Gluecker TM, Johnson CD, Wilson LA, Maccarty RL, Welch TJ, Vanness DJ, et al. Extracolonic findings at CT colonography: evaluation of prevalence and cost in a screening population. Gastroenterology. 2003;124(4):911-6. [PubMed ID: 12671887]. https://doi.org/10.1053/gast.2003.50158.
-
39.
Hara AK, Johnson CD, MacCarty RL, Welch TJ. Incidental extracolonic findings at CT colonography. Radiology. 2000;215(2):353-7. [PubMed ID: 10796907]. https://doi.org/10.1148/radiology.215.2.r00ap33353.